-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 471-474
doi:10.5923/j.ajmms.20231304.24
Received: Mar. 30, 2023; Accepted: Apr. 20, 2023; Published: Apr. 22, 2023

Results of Assessment of Morphometric Indicators of Respiratory Bronchial Walls in Newborn Babies in the Neonatal Period
Sultanov Ravshan, Sadikova Zumrat, Yusupova Shakhnozakhan, Yuldosheva Malika, Mukhammadaliyev Khasan
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this article, the research was conducted on the development dynamics and structure of the wall tissue structures of respiratory bronchioles in the neonatal period of babies. During the study, the following was proven: all the layers of the respiratory bronchioles are not well developed when babies are one month old, under the age of one year, the covering epithelium is multi-layered to single-layered, the transformation of the connective tissue from the unformed connective tissue to the forming tissue, from the sparse chondroid and cellular structure to the dense chondromatous tissue with small cells.
Keywords: Infant, Lung, Respiratory bronchiole, Postnatal ontogenetic stage, Histochemical, Histological, Hemotoxylin-eosin, Van-Gieson
Cite this paper: Sultanov Ravshan, Sadikova Zumrat, Yusupova Shakhnozakhan, Yuldosheva Malika, Mukhammadaliyev Khasan, Results of Assessment of Morphometric Indicators of Respiratory Bronchial Walls in Newborn Babies in the Neonatal Period, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 471-474. doi: 10.5923/j.ajmms.20231304.24.
1. Introduction
- It is known from the world health information that the death of children is one of the main problems in the world medical field. Today, the child mortality rate is 15.6% per 1,000 live births, but the birth rate is very low at 9.1% [10].Respiratory distress syndrome (RDS) in the neonatal period of the fetus is caused by pulmonary and non-pulmonary diseases. Respiratory system, diseases related to lungs: Narrowing of nasal passages, micrognathia, Pera-Robena syndrome, macroglossia, laryngeal and tracheal atresia, vocal fold paralysis, laryngeal cyst, laryngomalacia, tracheobronchomalacia, tracheo-erythral fistula, transient tachypnea of stillbirth, meconium aspiration syndrome, stillbirth pneumonia, pneumothorax, lung hypoplasia, lobar emphysema, surfactant protein deficiency.Respiratory system, non-pulmonary diseases: congenital heart defects, cardiomyopathy, cardiac tamponade, severe heart failure, pneumomediastinum, diaphragmatic hernia, birth trauma, hypoxic-ischemic encephalopathy, central malformation, chromosomal diseases, torch infection, meningitis, urinary syndrome (seizure), arthrogryposis, sepsis, hypoglycemia, metabolic acidosis, hypo- and hyperthermia, hypermagnesemia, hypo- and hypernatremia, hemolytic anemia [5,6,7,8].Ultrasonography of the lungs in infants from birth to 9 months of age, the conclusions and characteristics of the lung are statistically sufficiently correlated for the diagnosis of all lung segments, and "interstitial syndrome" is noted in the first 14-16 hours of life in premature infants without diseases of the respiratory system [1].Minimally invasive administration of airway surfactant (LISA) in preterm infants with respiratory distress syndrome (RDS) is a method of administering surfactant without endotracheal intubation that has shown promise in reducing the incidence of bronchopulmonary dysplasia (BPD) in preterm infants [2].In babies under 1 month, the mucous membrane of the trachea is thin, delicate, the glands are poorly developed, the number of smooth epithelia with a smooth surface compared to the ciliated epithelium in the covering epithelium was found to be 1.5 times higher. This causes a lot of acute respiratory diseases among children [3].After the larynx in the airways, the pulmonary-bronchial tree begins, and up to the alveoli of the lungs, there is a special respiratory system in humans, which becomes smaller and narrower until it reaches the parenchyma of the lungs, and the respiratory bronchioles connect to the alveoli. These tree-like structures branch 23 times at a distance, forming branches of the pulmonary-bronchial tree [4].There are 2 types of secretory cells in bronchial epithelium. Mastoid and Serous Secretory Glands: Mastoid cells are typical in shape, less often in newborns, and later increase in number.The study of age-related features and morphometric features of fetal and newborn organs is of interest not only for morphological sciences, but also for clinical sciences such as neonatology and pediatrics [9].In recent years, the negative impact of bronchopulmonary dysplasia on the overall development of the lungs, including the pulmonary vascular system, has been increasing. Recent studies have shown that having BPD increases the risk of developing pulmonary hypertension. Current international guidelines call for improved screening for this complication [10].Pulmonary hypertension and heart defects are among the most severe complications of bronchopulmonary dysplasia (BPD) and are associated with difficulty in diagnosis and high mortality. Doppler echocardiography was performed on 100 pediatric patients with bronchopulmonary dysplasia (BPD). Based on it, the level of development of pulmonary hypertension and the mechanisms of action of drugs were evaluated. The safety and efficacy of sildenafil in pulmonary hypertension with bronchopulmonary dysplasia (BPD) have been evaluated [12].Macroscopic and microscopic examination of the study revealed asymmetry in the distribution of respiratory system glands. The distribution number and density of respiratory system glands is 1.5-2.1 times higher in the left bronchus than in the right bronchus (p<0.05), the number of glands belonging to the upper part is 1.56-2.91 times (p<0.05) more. In terms of age, the number of glands and their size increased to a maximum at the age of 21-35 and then decreased with old age. At the same time, the distribution density decreased during the entire period of human life [11].Premature babies are the main part of the patients of neonatal intensive care and intensive care units. Respiratory distress is a leading cause of neonatal morbidity and infant mortality among premature infants. In order to improve the quality of medical care and reduce radiation exposure, the relevance advantage of using lung ultrasound is discussed [15].The purpose of the study: to evaluate the morphometric parameters of the postnatal ontogenetic morphology of the respiratory bronchiole wall in one-month-old babies.
2. Materials and Methods
- The examination was carried out on the corpses of one-month-old infants admitted in the first quarter of 2020-2022 at the Center for Pathological Anatomy of the Republic. Infants who died under the influence of various factors, but whose respiratory system did not change, were studied in the cadavers of children without diseases of the pulmonary bronchial passages, who died mainly from heart defects and other causes. The causes of death and the main disease were determined in the results of pathological anatomy. Examination materials were taken from the following part of the lungs: a macropreparation was studied by taking a respiratory bronchiole. Instrumental (with the help of barbell), general histological, histochemical, morphometric and statistical research methods were used in our research. The obtained materials were placed in formalin and then 3-5 m.km sections were prepared. They were stained with hemotoxylin-eosin, Schick's reaction, and Van-Gieson methods.
3. Research Results
- The respiratory system consists of the airways and two lungs. Respiratory tracts are divided into upper and lower respiratory tracts depending on their location in the body. The upper respiratory tract includes the nasal cavity, the larynx, the nose and mouth, and the lower respiratory tract includes the larynx, trachea (throat), bronchi, and lungs. Due to the presence of bone and cartilage in the wall of the respiratory tract, it has a characteristic tube-like structure that keeps the cavity at the same level. The inner surface of the airways consists of a mucous membrane with glands that synthesize mucus, and its surface is covered with floating epithelium. Therefore, the mucous membrane, along with its protective function, cleans the air and warms and moistens the air in the respiratory tract. The respiratory tract consists of the following parts: trachea, bronchi of lung lobes, segmental bronchi, interlobular bronchi, lobe bronchi, intralobular bronchioles and terminal bronchioles.To study the characteristics of the anatomy of the lower respiratory tract in the fetus, 50 fetuses from 15 to 23 weeks of age were examined. They were obtained during the termination of a normal pregnancy for social reasons and as a result of ante-intranatal fetal death from acute hypoxia. New information was obtained about the features of the macro-microscopic structure of the lower respiratory system, their microtopography, skelotope, syntopy, which required microsurgical intervention in fetal surgery [13-14].In this study, we aimed to study the microscopic image of specific changes in the respiratory bronchiole wall located in the lung parenchyma.
|
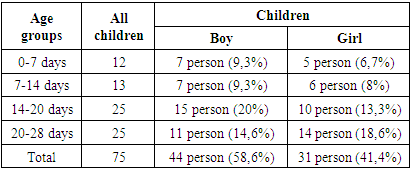
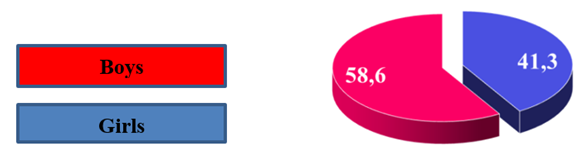 | Figure 2. Distribution by gender of the corpses of infants who died in the postnatal period of one month (%) |
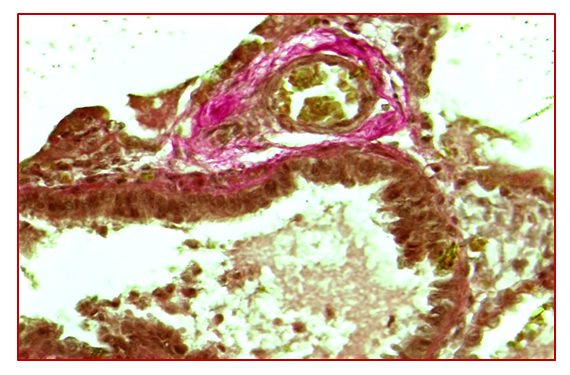
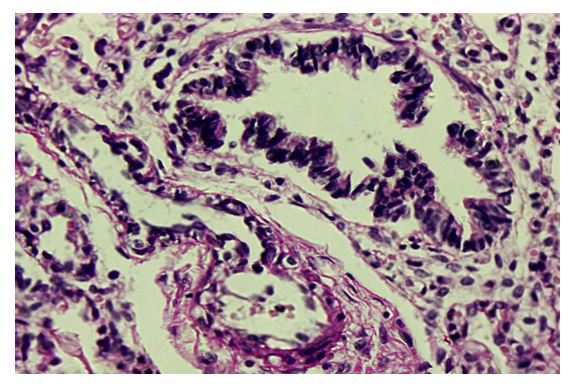
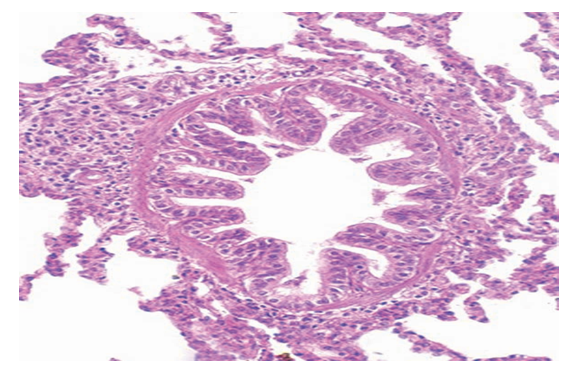
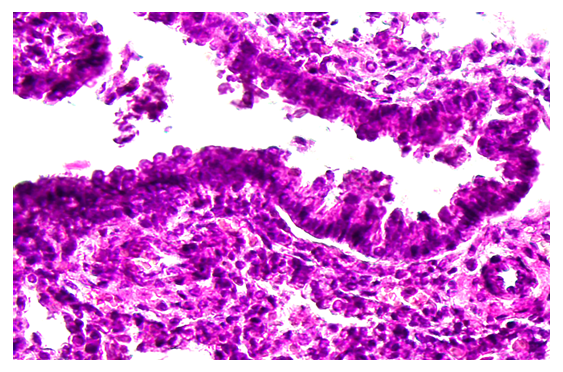 | Figure 3. Respiratory bronchiola, one month period. The wall of the bronchiole consists only of lining epithelium. Stained by hemotoxylin-eosin method. 10x40 enlarged image |
4. Conclusions
- The fetus goes through 3 periods in the stages of preparation for birth. At 20 weeks, the bronchial tree is fully formed. By the 28th week, the bronchi grow 1.7 times both in length and in width. By the 36th week, the bronchi expand mainly in width.The respiratory bronchiole is located directly in the lung tissue, and its wall consists of only one-layer prismatic epithelium, and it was found that the basement membrane is even attached to the lung tissue.After the larynx in the airways, the bronchial tree begins, and it branches 23 times in the distance to the alveoli, creating branches of the bronchial tree. The bronchial tree is a special ventilation system in humans, which becomes smaller and narrower until it reaches the lungs, and the respiratory bronchioles connect to the alveoli. The narrowing of these tree-like structures to such an extent ensures that air reaches the alveoli easily and completely during breathing.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML