-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 435-439
doi:10.5923/j.ajmms.20231304.17
Received: Mar. 22, 2023; Accepted: Apr. 14, 2023; Published: Apr. 22, 2023

CO2 Laser and Imiquimod in Treatment of Condyloma Accuminata
Yusupova Sh. A.
Basic Doctoral Student of Tashkent Medical Academy, Uzbekistan
Correspondence to: Yusupova Sh. A., Basic Doctoral Student of Tashkent Medical Academy, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

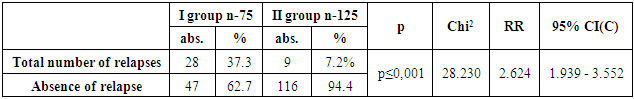
Objectives: Recurrence rate of condyloma acuminata are an issue, study was performed to evaluate better therapy. How laser treatment for external anogenital warts affected the continued clearance of treated lesions and the safety of topical Imiquimod used by the patient. Methods: Asses 2 type of treatment: monotherapy by laser with combined therapy - after laser treatment of visible external anogenital warts, the ablated region(s) were treated with Imiquimod 5% cream, in the following order: three times per week over the course of 12 weeks, starting once when the wound healing process was considered complete, followed by a six-month observation period for the assessment of sustained clearance of treated lesions. Results: 28 (37.3%) of the patients in the first group experienced relapses during the course of the study, according to a correlative assessment of the clinical competence of the treatment. The recurrence rate within 6 months was only 9 (7.2%) and clinical recovery without a recurrence was 116 (92.8%) in group II patients, which is a statistically significant (p≤0.05) reduction in the relapse rate with the complex method therapy. Conclusions: Administration of Imiquimod 5% cream three times per week seems to be safe and to lower the likelihood of wart recurrences after laser therapy and adequate wound healing.
Keywords: Condylomata acuminata, Immune response modifier, Recurrences
Cite this paper: Yusupova Sh. A., CO2 Laser and Imiquimod in Treatment of Condyloma Accuminata, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 435-439. doi: 10.5923/j.ajmms.20231304.17.
1. Introduction
- Human papillomavirus (HPV) anogenital infections are the most prevalent viral sexually transmitted disease (STD) among young people worldwide [1]. Treatments that have demonstrated good to moderate efficacy in eliminating genital warts include patient-applied topical medications (podophyllotoxin, interferon (IFN)), as well as ablative or cytodestructive techniques [1,2]. Due to anesthesia or many therapeutic interventions required to completely eliminate the wart region, the majority of ablative therapy techniques have the potential to be uncomfortable and painful for the patient. Yet, the high rate of wart recurrences after effective first treatment is thought to be the most source of frustration. The recorded recurrence rates for ablative techniques range from 20% with surgical excision to 50% with alternative destructive therapies. The lack of antiviral action with the majority of the suggested therapy is one theory for the recurrent recurrence of warts. As a result, only the wart itself is physically eliminated, leaving the surrounding tissue still harboring latent HPV that could reactivate [3,4].Since Imiquimod is known to generate many subtypes of IFN-a and IFN-g as well as a variety of cytokines linked to Th1-cell-mediated immunity, it is a more comprehensive and natural approach. The first member of a novel class of immune response modifiers with significant antiviral and anticancer action is Imiquimod, an imidazoquinolinamine derivate [5,6]. It has been demonstrated that Imiquimod 5% cream, used three times per week for a maximum of 16 weeks, is both extremely effective and secure for use in the primary treatment of external genital warts [7-9]. In one research, with three weekly doses and a 12-week treatment-free follow-up period, the recurrence rate was as low as 13% [8]. Recurrence rates following wart ablation may be lowered by adjuvant IFN therapy, which would also improve the patient's resistance to viral infections. The majority of study findings, however, did not consistently demonstrate the advantages of combination therapy [10]. This clinical trial examined whether the incidence of recurring warts following laser therapy may be decreased by using laser therapy followed by Imiquimod 5% cream for 4–16 weeks.
2. Methods
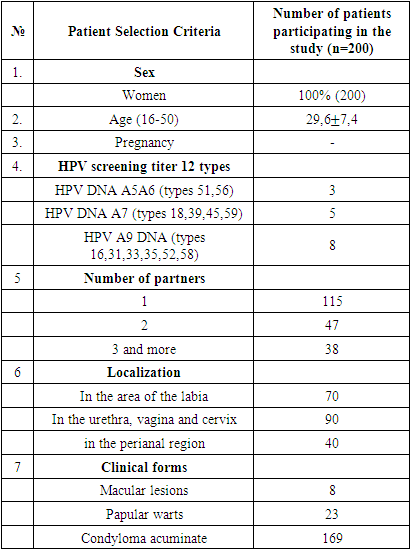
- Patients (n=200) were chosen from the university's laser dermato-venerology department. The main goal of the study was to analyze the efficacy and sustained clearance of anogenital warts following laser treatment as a monotherapy and combined therapy [laser+Imiquimod] as determined by clinical visual examination.PatientsThe trial was open to female patients with external anogenital warts aged 16 to 50. Patients were not eligible for the study if they had previously received Imiquimod, IFN, IFN-inducers, immunomodulators, oral antiviral medications (aside from oral acyclovir for suppressive or acute therapy), topical antiviral medications applied to the wart site, cytotoxic medications, other investigational medications, drugs known to have major organ toxicity, chemical and/or surgical wart therapy within four weeks of enrolling in the study, or any combination of these treatments (within two weeks of initiation visit). Also, patients with inflammatory skin disorders or those who required concurrent topical medication in the wart location were excluded, as were women who were expecting or nursing. 215 patients were enlisted at the start of the trial, but by the time it was over, only 200 remained. 15 patients were excluded for the following reasons: 8 patients voluntarily withdrew during the study; 3 patients required immunomodulators for acute illnesses; and 4 patients became pregnant while participating in the study. (Flowchart 1)
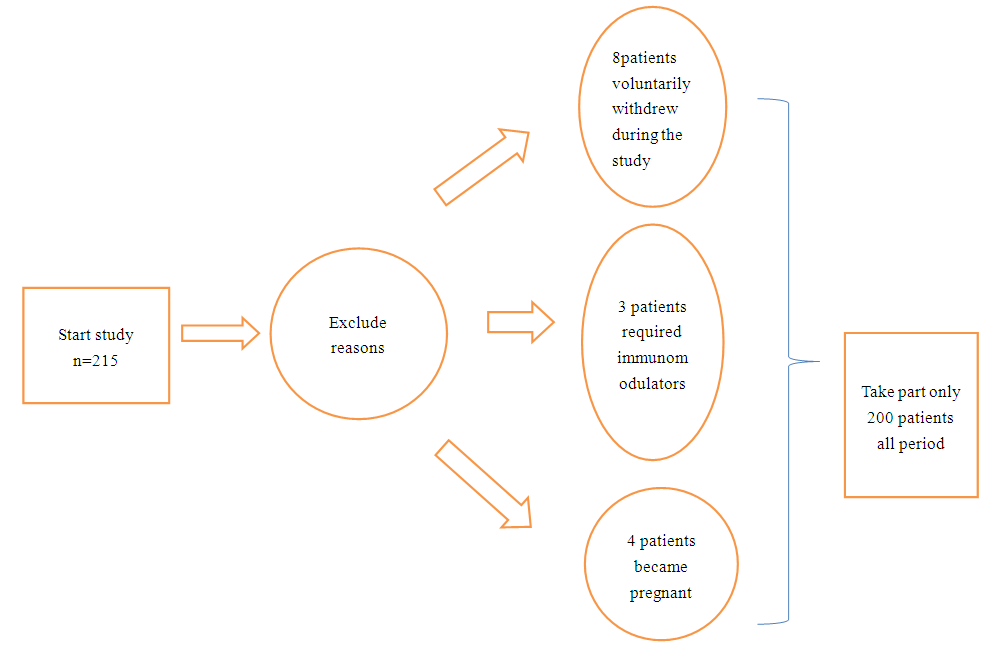 | Flowchart 1. Of enrolled excluded patients |
|
|
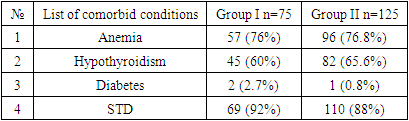
3. Results
|
|
4. Discussion
- With the complicated method therapy, there was a statistically significant (p≤0.05) decrease in the relapse rate, with the recurrence rate within 6 months being only 9 (7.2%) and clinical recovery without a recurrence being 116 (92.8%) in group II patients.More than 80% of patients had skin conditions, including burning, itching, soreness, and redness, in the locations where the warts were treated, as the most common side effects. In general, they were well tolerated and promptly subsided if the dosage was reduced or a break was taken.Recurrence rates after laser therapy for genital warts are vary, according to data from the literature, and they tend to happen more often around the edges of previously ablated areas. It has been suggested that the outcome could be enhanced by extending the ablation to surrounding, clinically unaffected regions that carry latent HPV beyond the apparent lesion [11]. Immune response modifiers allow for an alternative strategy by improving the cutaneous antiviral immune response. The outcomes of this open-label, prospective study show that Imiquimod 5% cream, an adjuvant topical immunomodulatory medication, can prolong the effects of laser therapy for external genital warts. In this study, laser therapy combined with Imiquimod 5% cream produced better benefits than laser therapy alone as reported in the literature [7,14].According to the literatures local cellular immune response is activated by adjuvant Imiquimod 5% cream treatment, and this response is principally mediated by the stimulation of specific pro-inflammatory and antiviral cytokines, primarily IFN-a, tumor necrosis factor-a (TNF-a), and various interleukines (e.g. IL-6, -8, -10, -12). A molecular investigation with HPV-infected patients has shown the mechanism of action in HPV-related genital warts [7]. Changes in the tissue levels of these cytokines and a considerable drop in viral load, as indicated by tissue levels of E7-mRNA and capsid protein L1-mRNA, were directly associated with wart regression. Most intriguingly, one trial participant who received placebo also completely cleared his warts, and the alterations in immunological markers that were observed in this participant were very identical to those in the patients who received Imiquimod. Similar to the immunological process that takes place during spontaneous regression, this improvement in the local immune response also has a long-term effect on cutaneous HPV-infections, preventing recurrences and new infections with the same HPV type or subtype [12].It is known from earlier research that Imiquimod 5% cream causes local skin reactions often, especially during the first month of treatment. These reactions are thought to be caused by local immune induction and are a crucial component of the medication's antiviral and anticancer activities [7-9]. In this study, Imiquimod 5% cream was used after laser therapy, and the first month of treatment was when skin responses were most common. The process of wound healing itself is connected to particular changes in skin immunology. It has been shown that over the 42 days following surgery.Simple study design is one of the strengths of this descriptive type of the research. Weaknesses of the study are single center study, Pamirid race, uzbek nation and small size of sample.
5. Conclusions
- The results of this study clearly show that topical Imiquimod 5% cream treatment for 12 weeks after laser treatment of genital warts is safe and appears to be an effective therapeutic approach to reduce the incidence of wart recurrences, which is one of the least desirable aspects of conventional treatment modalities.Using a combined approach to treat genital warts is a better technique of treatment since it allows for deeper penetration of the local 5% Imiquimod cream, which is where this medication's immunomodulatory properties are active, by reducing hyperkeratosis through laser vaporization. In turn, this cream affects the lesion's site-specific clinical and subclinical HPV forms, which cannot be treated by laser light. This result implies that these two approaches complement one another and lower the recurrence rate.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML