-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 407-411
doi:10.5923/j.ajmms.20231304.13
Received: Mar. 22, 2023; Accepted: Apr. 6, 2023; Published: Apr. 13, 2023

Cytokines as Predictors of Adverse Conditions in Premature Children from Complicated Pregnancy
Yuldasheva Gulnoz Giozovna1, Niyozova Durdona Shavkatovna2, Khamidova Nozima Komilovna3, Rustamov Bakhtiyor Bobokulovich2
1PhD., Assistant of the Department of Pediatrics, Bukhara State Medical Institute, Bukhara, Uzbekistan
2Assistant, Department of Pediatrics, Bukhara State Medical Institute, Bukhara, Uzbekistan
3Doctoral Student, Department of Pediatrics, Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This paper presents information on the cytokines IL-6 and IL-8 in premature newborns with perinatal CNS lesions and intrauterine infection, depending on gestational age and the severity of preeclampsia in pregnant women. It has been established that an increase in blood IL-6 has a diagnostic value in the pathogenesis of perinatal CNS lesions, and an increase in blood IL-8 indicates the progression of neonatal infections in premature babies from mothers with preeclampsia. An increase in IL-6 in the blood has been proven to be of diagnostic value in the pathogenesis of perinatal lesions of the central nervous system with the highest probability at a gestational age of 34-37 weeks, and an increase in IL-8 in the blood indicates the progression of neonatal infections in premature infants born at a gestation period of 28-33 weeks from mothers with severe preeclampsia and has a high correlation between gestational age and severity of preeclampsia.
Keywords: Preeclampsia, Preterm infants, Perinatal CNS damage, Intrauterine infection, Cytokines
Cite this paper: Yuldasheva Gulnoz Giozovna, Niyozova Durdona Shavkatovna, Khamidova Nozima Komilovna, Rustamov Bakhtiyor Bobokulovich, Cytokines as Predictors of Adverse Conditions in Premature Children from Complicated Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 407-411. doi: 10.5923/j.ajmms.20231304.13.
1. Introduction
- Premature birth remains an urgent medical and social health problem. Statistical indicators of preterm birth have not tended to decrease for many years [1,5,6]. The onset of pregnancy on an unfavorable background contributes to its burdened course. Prerequisites are being created for the onset of premature birth. Preeclampsia is one of the most common causes of premature birth [7]. The problem of infectious and inflammatory diseases of newborns remains extremely urgent, which is associated with a high level of neonatal mortality from infections, where they are the main cause of death or complicate the course of the underlying disease. The development of infectious and inflammatory diseases, according to many authors, is largely due to the peculiarities of the immunological resistance of newborns. There are data on changes in the immune system in the literature, but all changes in the links of immunity in infectious and inflammatory diseases in newborns have not been fully studied. Cytokines regulate many processes in the body of a pregnant woman, including termination of pregnancy. During pregnancy, changes in the cytokine content resulting from the development of an immune response have a direct effect on the vascular endothelium, which reacts to various humoral stimuli with the production of vasoconstrictor and vasodilator factors, the balance of which determines the tone of smooth muscle cells, being very important in the regulation of vascular tone. Endothelial cells are both producers and effectors of IL-1, IL-6, and IL-8 and, when activated, contribute to the production of these cytokines [4].The main regulator of the immune response, reactions of the acute phase of inflammation and hematopoiesis is IL-6, it acts as a mediator of protective processes against infection and tissue damage. The main source of IL-6 is macrophages, it is also produced by fibroblasts, monocytes, endothelial cells and endometrial stromal cells. Its production is stimulated by other cytokines: IL-1, IL-2, TNF-α, as well as interferon—α. Normally, there is minimal production of IL-6, but when encountering pathogens, its content in the circulatory bed increases. IL-6 activates the synthesis of acute phase proteins in the liver, while IL-1 and TNF-α stimulate their synthesis and act on this process indirectly, through IL-6. IL-6 is a marker of intrauterine infection during pregnancy, while its high content is detected in amniotic fluid and umbilical cord blood newborns. Increased production of TNF-α and IL-6 causes a violation of the regulation of cellular energy exchange and metabolism in children with myocardial ischemia with severe perinatal hypoxia. In deeply premature newborns whose mothers were diagnosed with chorioamnionitis, a significant increase in TNF-α and IL-8 levels is noted in the first week of life, which is a prognostically unfavorable factor in the development of bronchopulmonary dysplasia. In this group of children, signs of DN persist for a long time, and the time of ventilation is significantly increased [3]. Determination of the level of IL-6 in newborns is necessary to confirm bacterial sepsis, because this cytokine has high sensitivity and specificity. The production of cytokines by the fetus depends on the condition of the placenta. According to the literature, an increase in the level of IL-6 in the residual umbilical cord blood of a newborn has a certain pathogenetic relationship with the nature of inflammatory reactions in the afterbirth. An increase in the concentration of IL-6 in residual umbilical cord blood is a non-specific reaction that occurs in response to the development of an inflammatory process in the placenta, which is confirmed by morphological studies of the placenta [9].In-depth study of the immunopathogenesis of neonatal infectious diseases of bacterial and mixed etiology will improve the quality of diagnosis and prognosis of the course of the disease, justify and use rational methods of immunocorrection in complex intensive care in newborn children. The immune system of newborns is in a state of physiological depression. Immune regulation is carried out by anti–inflammatory cytokines - IL-1, IL-6, IL-8, IL-12, tumor necrosis factor (TNF-α), alpha and gamma interferons, etc., as well as cytokines that directly regulate the direction and spectrum of the immune response (IL-2, IL-5, IL-7). Others are involved at the stage of earlier regulation of myelomonocytopoiesis and lymphopoiesis IL-3, colony-stimulating factors). In clinical practice, the definition of a limited set of cytokines is usually used, reflecting the intensity of the local and/or systemic response to infection. The infectious nature of complications is confirmed by a significant increase in the level of IL-6 with a reduced TNF-α content, while non–infectious complications are accompanied by increased concentrations of IL-1 without changes in the content of TNF-α and IL-6. Mortality rates from neonatal sepsis remain high and, according to various authors, range from 30 to 60%. The highest rates are observed in deeply premature infants with extremely low birth weight (less than 1000 g) [7].With cerebral lesions in newborns from mothers with gestosis, the concentrations of proinflammatory cytokines in the blood serum increase, and as the complication progresses in pregnant women, the cytokine imbalance in their infants worsens. In newborns with severe brain damage, manifested by convulsive and progressive hypertensive-hydrocephalic syndromes, the level of IL-1ß in the cerebrospinal fluid significantly exceeds the corresponding indicator in the blood serum, which is probably a consequence of local cytokine synthesis in the central nervous system by activated microglia.The revealed violations indicate a significant contribution of proinflammatory cytokines in the pathogenesis of perinatal CNS lesions in newborns from mothers with gestosis. In conditions of pathology, including ischemia, an increased IL-1 content in the central nervous system is the main signal for the induction of other pro-inflammatory cytokines, as well as stimulation of astrocytes to produce potential neurotoxic substances, such as nitric oxide and arachidonic acid metabolites. The participation of the main trigger of inflammatory reactions, IL–1ß, in the processes of apoptosis is important [8], which indicates a unified induction of the long-term consequences of ischemia, as well as the fact that programmed cell death is closely dependent on the local inflammatory reaction in the ischemic region of the brain and necrosis processes. The expression of genes encoding IL-1ß – converting enzymes, caspases, causes the synthesis of proteins that determine the survival or death of cells. IL-6 induces and increases stress, that is, it forms a vicious circle leading to the hyperproduction of adrenaline, ACTH and glucocorticoids. IL-1 and TNFa are powerful inducers of IL-6 synthetase in astrocytes, while IL-6 suppresses the synthesis of IL-1 and TNFa. This feature determines its dual role in the development of inflammation: being a typical pro-inflammatory cytokine in its effects, it also has an anti-inflammatory effect, limiting the production of other pro-inflammatory cytokines [8].The aim of the study: to study cytokines IL-6 and IL-8 in premature newborns with perinatal lesions of the central nervous system and neonatal infection, depending on gestational age and severity of preeclampsia in pregnant women to improve therapeutic and preventive measures.
2. Materials and Methods
- The results of a prospective clinical examination of 40 newborns born to mothers with severe preeclampsia at gestation from 28-37 weeks were analyzed, which are divided into 2 subgroups: 1a (n=20) – premature babies born at gestation from 28-33 weeks, 1b (n=20) premature babies born at gestation from 34-37 weeks. The control group consisted of 20 (n=20) newborns from healthy mothers with a physiological course of the adaptation period. These children had no somatic and neurological disorders and were discharged home in a satisfactory condition for 4-5 days of life. Depending on the severity of preeclampsia, the children were divided into 2 groups. Group 1 included 15 infants from mothers with moderate preeclampsia, group 2 included 25 premature infants from mothers with severe preeclampsia. To determine the concentrations of IL-6, IL-8, umbilical blood serum was used. Immunological examination was performed by the standard method of solid-phase ("sandwich" variant) enzyme immunoassay at the Institute of Human Immunology and Genomics of the Academy of Sciences of the Russian Academy of Sciences. Exclusion criteria: severe fetal malformations, shock states, extreme low body weight, unwillingness of the child's parents to participate in the study. The children underwent laboratory and instrumental examination (general analysis of blood, urine, biochemical blood analysis, ultrasound examination of the brain and abdominal organs), sedative therapy was prescribed according to the indications.
3. Results and Their Discussion
- The diagnosis was made based on the classification of perinatal lesions of the central nervous system. Cerebral ischemia of the first degree was diagnosed in 12 (30%) newborns, grade II – in 13 (32.5%), grade III – in 15 (37.5%). Periventricular hemorrhage was detected in 15 (37%) infants, intraventricular hemorrhage of the II degree had 17 (42%) newborns.
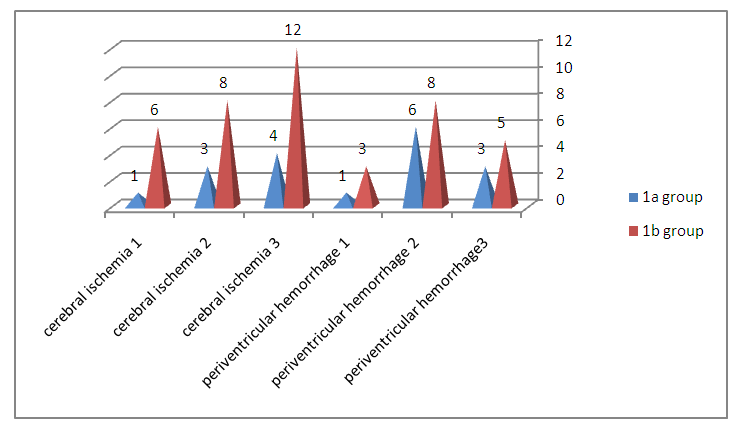 | Figure 1. The structure of perinatal lesions in the main groups |
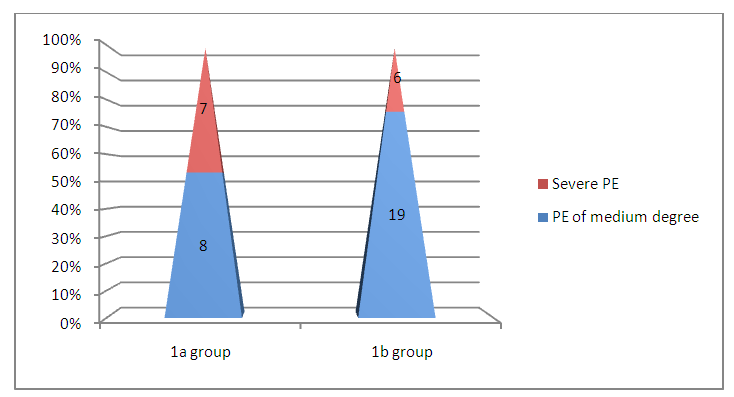 | Figure 2. Distribution by severity of preeclampsia in the main groups |
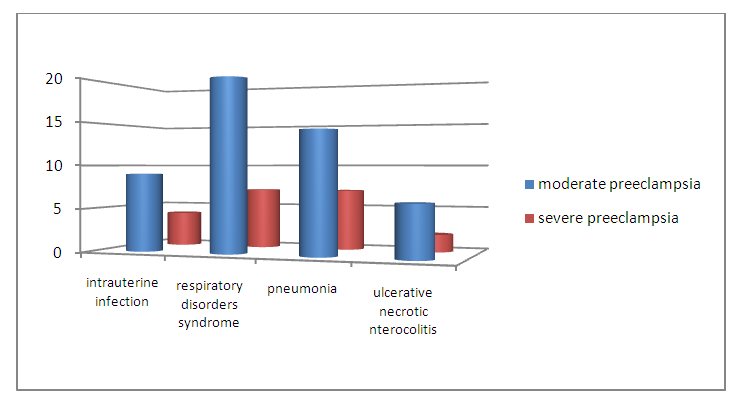 | Figure 3. Structure of neonatal infections in the main groups |
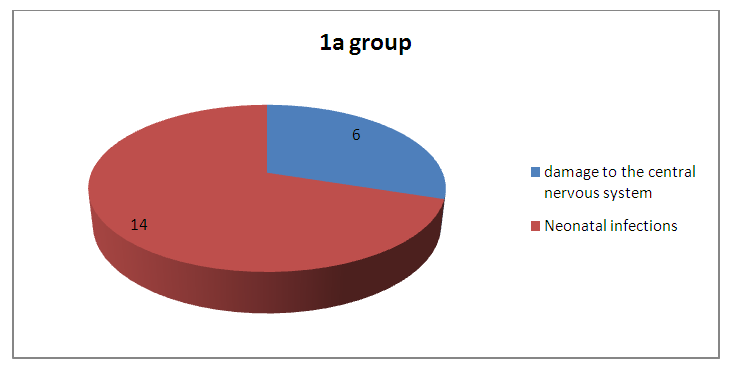 | Figure 4. Frequency of occurrence of CNS lesions and neonatal infections in group 1a |
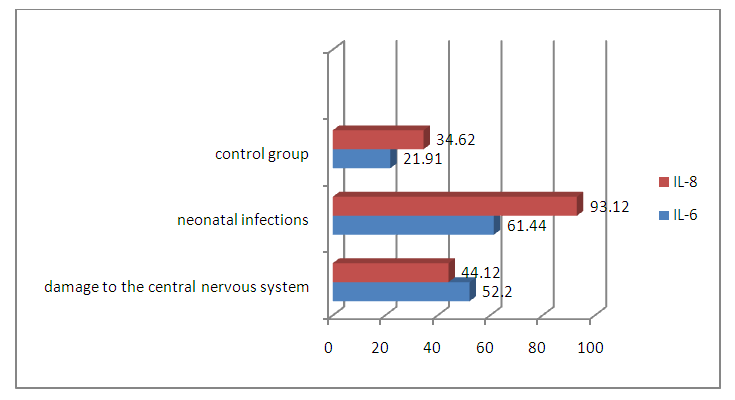 | Figure 5. The concentration of interleukins in CNS lesions and neonatal infections in group 1a |
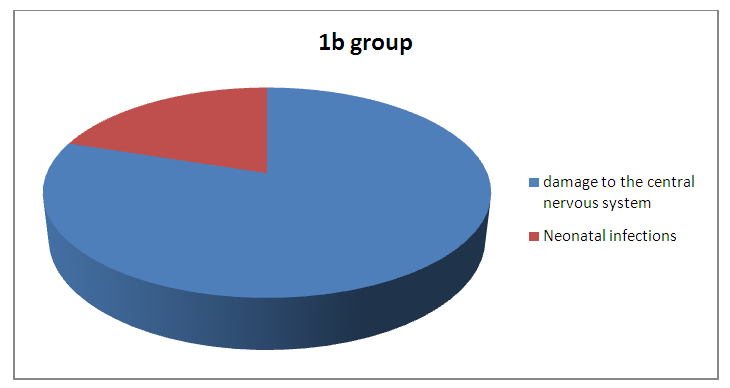 | Figure 6. Frequency of occurrence of CNS lesions and neonatal infections in group 1b |
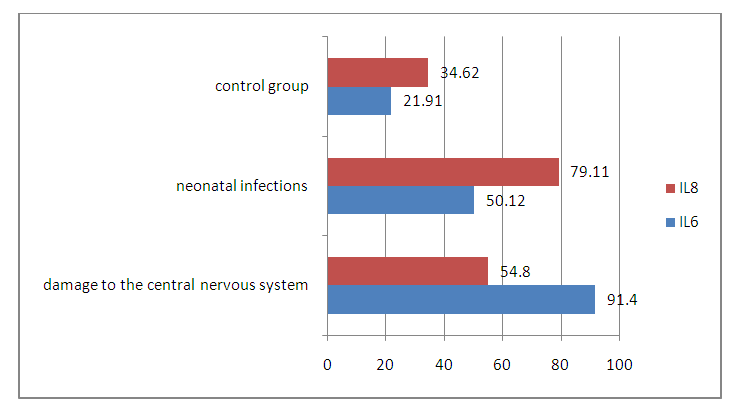 | Figure 7. The concentration of interleukins in CNS lesions and neonatal infections in group 1b |
4. Conclusions
- Thus, with cerebral lesions in newborns from mothers with preeclampsia, the concentrations of pro-inflammatory cytokines in the blood serum increase, and as the complication progresses in pregnant women, the cytokine imbalance in their infants worsens. An increase in IL-6 in the blood is of diagnostic importance in the pathogenesis of perinatal CNS lesions with the greatest probability at a gestation period of 34-37 weeks, and an increase in IL-8 in the blood indicates the progression of neonatal infections in premature infants born at a gestation period of 28-33 weeks from mothers with severe preeclampsia and has a high correlation between the gestation period and severity of preeclampsia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML