Jasur Rizaev1, Ravshan Fattakhov2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Ravshan Fattakhov, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article describes the results of applying the burnout syndrome correction scheme among dentists in Uzbekistan. Medications and progressive muscle relaxation by Jacobson were used as correction measures. For an objective assessment of the effectiveness of the proposed scheme, the following salivary biomarkers were used: sIgA, cortisol, α-amylase, and chromogranin A.
Keywords:
Burnout syndrome, Biomarkers, Stress, Dentists
Cite this paper: Jasur Rizaev, Ravshan Fattakhov, Evaluation of the Efficiency of the Application of the Burnout Syndrome Correction Scheme in Dentists, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 364-366. doi: 10.5923/j.ajmms.20231304.05.
1. Introduction
Communicative professions, which include dentists, are largely prone to burnout syndrome [1]. Various factors influence the development and progression of burnout syndrome, making it difficult to diagnose and prevent. The development of the burnout process can take decades. It appears and progresses almost imperceptibly, and the affected person is usually not even aware of the problem [2]. However, the consequences of BS (burnout syndrome) have a great impact on the health of specialists. The problem of BS is very urgent and the testing of the scheme for the correction of the syndrome was the goal of this study.
2. Materials and Methods
150 dentists were selected to participate in the study. They were divided into the following groups:1) basic, 75 people (with BS correction);2) control group, 75 people (without correction).Biochemical research methods were used: the evaluation stages consisted of saliva collection at baseline, before the application of the scheme and immediately after the application of the BS correction scheme. The time of collection of saliva samples in sterile tubes was from 8 to 10 am. To do this, participants were advised to abstain from food and drink (other than water), as well as the use of caffeine, alcohol, or any other drug for 60 minutes prior to these sessions. Saliva samples were frozen at -20°C immediately after they arrived at the laboratory, and they were kept in this state until analysis. Quantitative measurement of sIgA was performed according to the Mancini method (radial immunodiffusion). Salivary cortisol concentration and α-amylase activity were measured using a Mindray BS 230 biochemical analyzer (PRC) by spectrophotometric method. HUMAN reagents (Germany) were used.Suggested burnout syndrome (BS) correction scheme:Drug treatment scheme: stage 11. Vitamin therapy (vit. groups B1, B6, B12) -Neurorubin-Forte 1-2 tablets per day.2. Magnesium salts (magne B6-forte) - 2-3 tablets with meals for a month.Stage 2:1. In the morning, taking adaptogens: Eleutherococcus extract (30-40 minutes before meals, 20-40 drops 2-3 times a day) or ginseng (30-40 minutes before meals, 15-25 drops 2-3 times a day. The course of treatment is 30 days.). For hypertension, doctors started with 3-5 drops and increased the dose to 30-40 drops.2. In the evening sedatives: valerian (1 tablet 2-3 times a day, 1 month).Progressive muscle relaxation according to Jacobson was also used - this is a non-pharmacological method of deep muscle relaxation. It is based on the premise that muscle tension is the body's psychological response to anxiety-producing thoughts, and that muscle relaxation blocks anxiety. The technique involves learning to control tension in specific muscle groups by tensing each muscle group first. This tension is then released as attention is directed to the differences felt during tension and relaxation. Ethics approval: The study has been conducted in full accordance with the Helsinki declaration by World Medical Association. Tashkent state dental institute Institutional Review Board gave the approval for conducting the study and verbal informed consent from the all dentists was also obtained prior to the survey. Information from all the participating dentists was collected ensuring anonymity of the information provided.
3. Results and Discussion
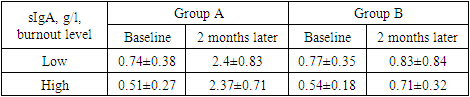
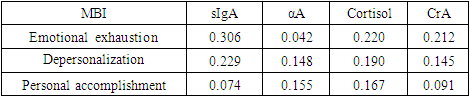
Salivary stress markers were chosen as an objective way to test the effectiveness of the program, since they can be collected in a non-invasive way, which creates psychological comfort for the subject.Cortisol, α-amylase, and chromogranin A were chosen as stress markers. In addition, the state of local oral immunity was studied in doctors with BS (sIgA), because fluctuations in sIgA concentration can also be considered as signs of occupational stress.The collection of markers was carried out twice: at the time when doctors received appointments and after 3 months from the start of measures to correct the BS.Salivary immunoglobulin A (sIgA). Immunoglobulin A is an indicator of the state of immune function and a reliable and widely used biomarker that interacts with the stress response. Constant and untreated work stress lowers sIgA levels. A sustained decrease in IgA secretion was found to be associated with an increase in salivary cortisol levels, suggesting that high cortisol levels may act as a factor in suppressing local oral immunity. This may explain the higher prevalence of colds in stressed individuals.Table 1. Dynamics of changes in the concentration of sIgA in doctors with BS
 |
| |
|
The table shows mean sIgA values and standard deviations before and after the first and last BS sessions. From the beginning to the end of the first and last sessions, participants who applied correction measures had a statistically significant increase in sIgA levels (3.24 times for low risk of burnout and 4.65 for high risk). As for the control group, the participants' sIgA levels increased slightly in the last session. But before the first session, the level of sIgA did not differ significantly between the two groups.The results of the differences between the groups showed that the participants in the main group had a greater improvement in the average perceived stress and burnout (emotional exhaustion) than in the control group.The study of the concentration of sIgA showed that the use of the proposed measures to combat occupational stress and BS in dentists reduces the level of emotional burnout and stress and has a positive effect on mental health.Moreover, participants who completed the program noted a significant improvement in their average psychological flexibility and improved self-esteem. Improving self-esteem affects work productivity and emotional exhaustion.Our results confirm that sIgA is a biomarker capable of measuring changes in immune function status in physicians with occupational stress and BS. In this study, participants in the main group experienced an increase in their immune function in the last sessions. This means that the corrective measures were able to counteract the effect of work-related stress on sIgA in sessions in which we could evaluate it.Table 2. Dynamics of changes in the concentration of salivary cortisol in doctors with BS
 |
| |
|
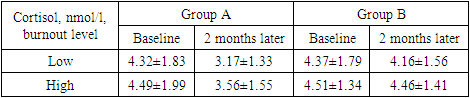
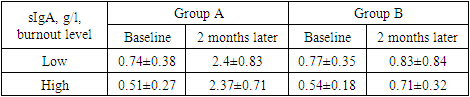
Initially, cortisol scores were not significantly different in both groups at the first session. However, after the application of correction measures, significant differences in cortisol concentrations were revealed: if before the start of the program, the cortisol concentration in both groups of dentists did not have a significant difference (p<0.005) and corresponded to 4.32±1.83 and 4.37± 1.79 nmol/l at a low level of burnout, at a high level - 4.49±1.99 and 4.51±1.34 nmol/l. After 2 months, which in group A corresponded to the last session of applying BS correction measures, the concentration of salivary cortisol in group B did not have a significant difference from the initial values, while in group A it decreased in individuals with an initially low level of BS - by 36.27%, and with a high BS - by 26.12%.Cortisol is a steroid hormone that is a member of the glucocorticoid family. It is secreted by the adrenal cortex through the hypothalamic-pituitary-adrenal (HPA) axis and its concentration changes in response to stress factors, increasing proportionally their duration and intensity. Table 3. Dynamics of changes in the concentration of salivary α-amylase in doctors with BS
 |
| |
|
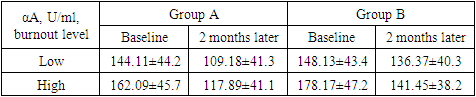
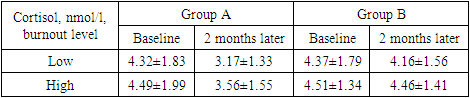
Salivary cortisol concentration serves as a proxy for serum cortisol concentration, whether at rest or during the exercise. Salivary cortisol reflects the biologically active fraction of total serum cortisol, and some studies have shown that the change in cortisol in response to stress in saliva is more dramatic than in blood, making salivary cortisol more sensitive and providing a more accurate measure of the dynamic activity of the HPA axis.At a low level of burnout, the α-amylase indices did not have significant differences in both groups at the first session, while at a high level there was a slight difference of 9.92% between the groups. However, after the application of correction measures, significant differences in cortisol concentrations were revealed: if before the start, the concentration of α-amylase in both groups of dentists did not have a significant difference (p<0.005) and corresponded to 144.11±44.2 and 148.13±43 .4 U/l at a low level of burnout, at a high level - 162.09±45.7 and 178.17±47.2 U/l. After 2 months, which in group A corresponded to the last session of the application of measures to correct BS, the concentration of α-amylase in group B, like cortisol, did not have a significant difference from the initial values, while in group A there was a decrease in persons with initially low level of BS - by 24.9%.Based on the available data, it can be argued that chronic stress may impair the functioning of the sympathoadrenal system or the HPA axis, or the interaction between the two systems. Because salivary α-amylase is less affected by variables such as age, habitual smoking, coffee and drug intake than cortisol, it may be a more reliable indicator of psychological stress. Daily production of salivary α-amylase is inversely related to salivary cortisol, and typically salivary α-amylase levels decrease upon waking and then rise steadily throughout the day. Salivary α-amylase has been found to be associated with stress in a number of contexts, including professional activities. In one of the few studies comparing salivary cortisol and α-amylase in the context of occupational stress.There is a positive correlation between salivary amylase concentration and burnout scores, and women show a significant increase in salivary α-amylase activity in the presence of a stressor compared to men.Table 4. Dynamics of changes in the concentration of salivary chromogranin A in doctors with BS
 |
| |
|
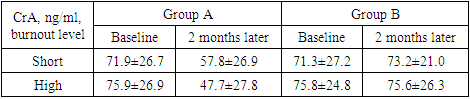
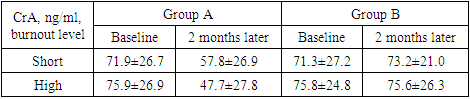
At low and high levels of burnout, the indices of chromogranin A did not have significant differences in both groups at the first examination. However, after completing the program, significant differences in CrA concentrations were revealed: if before the application of the scheme, the concentration of chromogranin A in both groups of dentists did not have a significant difference (p<0.005) and corresponded to 71.9±26.7 and 71.3±27.2 ng/ml at a low level of burnout, at a high level - 75.9±26.9 and 75.8±24.8 ng/ml. After 2 months. in group A, the use of burnout correction measures, the concentration of chromogranin A in group B, did not have a significant difference from the initial values, while in group A, it decreased in persons with an initially low level of burnout by 24.39%, and with a high burnout - by 59.12%.Salivary CrA levels increased significantly in individuals with BS and decreased after the regimen. This result indicates that salivary CrA can be used to diagnose BS.We have noted a strong relationship between BS and stress biomarkers in dentists. Further research is required to establish concrete links between work load and salivary biomarker ratios. Knowledge of these associations would shed light on the specific mechanisms underlying the links between burnout and adverse health outcomes.Table 5. Pearson correlation between burnout parameters and stress biomarkers
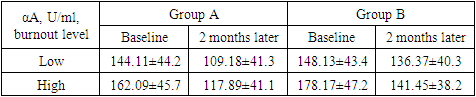
 |
| |
|
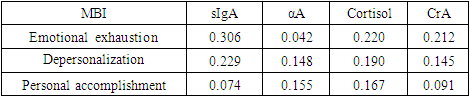
The results show that chromogranin A, cortisol, α-amylase, or sIgA levels can be predictive of burnout or stress, as expected. The data support the hypothesis that self-reported burnout may be related to physiological measures of stress.
ACKNOWLEDGEMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
| [1] | Stanetić K., Petrović V., et al. The Presence of Stress, Burnout Syndrome and the Most Important Causes of Working Stress Among Physicians in Primary Health Care – an Observational Study from Banja Luka, Bosnia and Herzegovina // Acta Medica Academica, - 2019, - No. 2(48), - P 159-166 doi: 10.5644/ama2006-124.254. |
| [2] | Frey R. When Professional Burnout Syndrome Leads to Dysthymia. Journal of the Canadian Dental Association January 2000, Vol. 66, no. 1 33-34. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML