-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 355-358
doi:10.5923/j.ajmms.20231304.03
Received: Feb. 26, 2023; Accepted: Mar. 25, 2023; Published: Apr. 13, 2023

Methods to Improve a Surgical Treatment of Impression Fractures of the Proximal Humerus
Khodzhanov I. Y.1, Tadjinazarov M. B.1, Elov D. R.2
1SE “Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Uzbekistan
2Ilyas Irgashev City Clinical Hospital No 4, Uzbekistan
Correspondence to: Tadjinazarov M. B., SE “Republican Specialized Scientific and Practical Medical Center of Traumatology and Orthopedics, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective. Surgical treatment of patients with impression fractures of the epimetaphysis of long tubular bones has not been studied widely and still presents difficulties in methods. The aim of the work of impressions of the humerus is to improve the results of treatment, based on the distribution of impression defects and the filling of residual cavities, by using a combination of plastic materials. Material and methods. The work is based on observations of 15 patients who were on treatment in 2017-2021 at the trauma department of the 4th city hospital of acute intra- and periarticular fractures of the metaphyses of the humerus. Results. The range of motion of the shoulder joint was started in a month and the full volume was achieved by the 50th day of the postoperative period. The mean healing time for defective fractures was 82.5 days. From the clinical aspect, good results were obtained in 13 patients with impression fractures of the shoulder, satisfactory results in two patients, which were associated with additional trauma. Conclusion. Autoosseous grafting, being the gold standard for filling bone cavities, is practically applicable for defects of more than 1 cm. For larger defects (fistula 3 cm) of the metaphyseal zone, it is better to use a combination of the method with platelet-rich PRP (Platelet Rich Plasma) therapy together with the use of whole erythrocyte mass.
Keywords: Tubular bones, Fractures, Distal epimetaphysis, Proximal epimetaphysis
Cite this paper: Khodzhanov I. Y., Tadjinazarov M. B., Elov D. R., Methods to Improve a Surgical Treatment of Impression Fractures of the Proximal Humerus, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 355-358. doi: 10.5923/j.ajmms.20231304.03.
Article Outline
1. Introduction
- Intra-articular and periarticular fractures of the humerus, in fact, metaphyseal and metadiaphyseal fractures are severe injuries of this limb and range from 7-10,2% of all fractures of the humerus. Fractures of the proximal humerus, distal radius, and including the proximal ulna, are especially common in the elderly patients. The presence of bone osteoporosis in the elderly patients, that is softening of the bone tissue compared to young people, leads to an impact fracture of the bone and a lack of bone tissue [1,2].Some studies have found a trend towards an increase in the incidence of fractures of the proximal humerus in the age group over 70 years. Fractures are more common in women, with those over 60 years of age and life expectancy up to 82 years, the risk of fracture of the humerus reaches 8%. Some researchers have noted an exponential increase in the number of fractures of the proximal humerus since the age of 50. There is a point of view that fractures of the proximal humerus will increase exponentially [8,9].This type of damage is often accompanied by bone tissue impression from the articular surface and damage to important soft tissue structures, which follows from the structural features of the joint (significant muscle mass, close location of the main vessels, nerves). The more bone mineral density is reduced, the more pronounced the impression to the epimetaphyseal cancellous bone. Most surgeons consider an impression fracture an indication for osteoplastic surgery, since these fractures in 78% of cases are accompanied by a violation of the congruence of the articular surfaces. The relevance of the problem under consideration is also determined by the fact that these fractures are characterized by a high frequency of adverse functional outcomes: osteoarthritis of the shoulder joint and contractures often develop in the long-term period after injury [3].The bones of the spongy structure of the extremities have a periarticular localization, as a result of which, with a slight impression, the diagnosis of fractures of these bones is very difficult, and with a significant impression, problems arise in filling the bone defect and fixing the fracture. The main method for diagnosing a fracture and its complications is an X-ray examination, including the use of various styling. The data of the authors confirm the expediency of using computed tomography, MRI, which is especially important for detecting intra-articular displacement of small fragments [4,5,6].Despite the development of new diagnostic methods and principles of treatment, the results obtained after the use of modern fixators are low, there are complications and high disability. There are many questions about the indications for surgical correction of impression fractures, the use of bone grafting and fixation of bone fragments, especially in comminuted fractures [7].
2. Objective
- The aim of the work of impression fractures of the humerus is to improve the results of treatment, based on the distribution of impression defects and the filling of residual cavities, by using a combination of plastic materials.
3. Material and Research Methods
- The work is based on observations of 15 patients with with an acute inside and periarticular fractures of the metaphyses of the humerus, who were treated in 2017-2021 in the traumatology department of the 4th city hospital of Tashkent city named after Irgashev. Clinical, radiological, computed tomography, biomechanical, statistical research methods were applied. To fill small cavities, we have undertaken the PRP (Platelet Rich Plasma) therapy technique with platelet-rich platelets using a whole erythrocyte mass in the future. The technique is as follows: 10-20 ml of whole blood is taken from the patient's vein into a vacuum container, 2-3 drops of heparin are added and centrifuged at 2000 rpm for up to 7 minutes. Then, the separated plasma with about 5 ml of platelets is removed from the container and injected into a predetermined location of the fracture. After the 3rd or 4th session, a whole erythrocyte mass is administered 2 times in an amount of about 2-3 ml. (therefore, when describing clinical cases, (4 + 2) value is used). The erythrocyte mass is also taken from the same container, only it is taken from the deep layers of centrifuged blood. The sampling and management technique is quite simple and has the option of sharing with any osteosynthesis methods and under aseptic conditions without infectious complications. The technique is carried out mainly in stationary conditions or the last injections can be performed on an outpatient basis.
4. Results and Discussion
- Treatment of patients with fractures of the proximal end of the humerus (15), small impression defects were found in 8 patients. They received PRP therapy in the amount of 5-6 ml. 6 (4+2) times and bone fragments were fixed with LCP plates, three of them were filled with bone metaphyseal mass. In the remaining 7 patients, crater- shaped impression defects up to 2 cm were found. These patients underwent bone grafting according to the shape of the iliac wing with one cortical plate, fixation also with LCP plates. Large bone defects (more than 3 cm) were not found in the observed patients. In 8 patients with small defects, the results were good and excellent (from 65 to 75 points). In 5 patients out of 7 with impression defects from 1 cm to 1.7 cm, the results in points ranged from 65 to 72 points, i.e. good, and 2 patients it was 56 and 57 points i.e., were satisfactory.With small defects in 8 patients, during osteosynthesis and PRP therapy in the amount of 5-6 ml. 6 (4+2) times and 3 patients filling with a bone metaphyseal mass did not notice great difficulties, osteosynthesis turned out to be stable and full-volume plasty of defects. They did not need additional fixation, and the next day passive and on the 15th day active development of the shoulder joint was started. The full volume of movement was achieved within a month. Their fusion time was 68.7 days. Multifragmented fractures (3 or more fragments) with impression defects up to 2 cm created certain difficulties in determining the shape of the defect and its volume. Almost managed to close the weight of the defect completely without additional manipulations. When the fragments were stabilized, the plate could be placed over the plastic material, which created a strong fixation of the fragments. Care should be taken not to dislodge the plastic material as the screws pass through it. The range of motion of the shoulder joint was started in a month and the full volume was achieved by the 50th day of the postoperative period. Average healing time for defective fractures was 82.5 days. In the clinical aspect, good results were obtained in 13 patients with impression fractures of the shoulder, satisfactory results in two patients, which were associated with additional trauma.
5. Clinical Example
- Patient S. was injured in a fall on her left shoulder at home. The radiograph revealed a comminuted impression fracture of the surgical neck of the left humerus with displacement of bone fragments (Fig. 1). An open reposition and osteosynthesis with a blocking plate (Fig. 2) and filling of the defect with autologous bone from the ilium were performed. After surgery, an X-ray of the left shoulder joint was taken. The bone fragments are in a satisfactory position (Fig. 3). On the damaged joint, he began early development, late loading. The plaster bandage was removed after 3 weeks and development of the shoulder joint was started. After 2 months, he began active movements in the shoulder joint. On the 3rd month after the operation, the patient moved in full volume.
 | Figure 1. X-ray before surgery of the left shoulder joint |
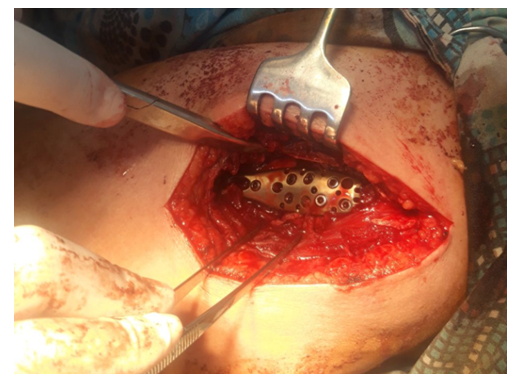 | Figure 2. Osteosynthesis with a blocking plate and filling of the defect with an bony autograph from the ilium |
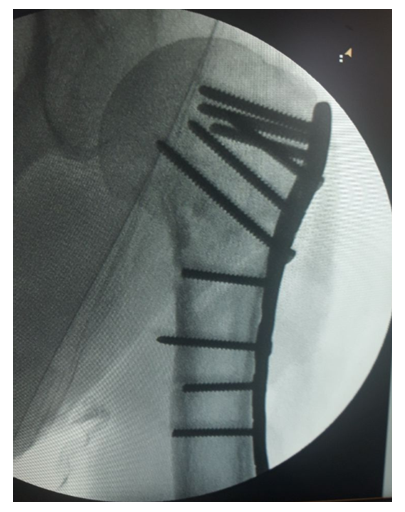 | Figure 3. X-ray after surgery of the left shoulder joint |
6. Conclusions
- 1. Digital x-rays are a fairly informative diagnostic study for impression fractures of metaphyseal localizations. To determine the volume and shape of impression cavities or to determine residual defects after bone grafting, it is best to use MSCT studies. MRI studies are indispensable for impressions associated with damage to intraarticular structures.2. One of the fundamental therapeutic tactics in the treatment of impression fractures is the identification and filling of the resulting cavities (a bone fragment or PRP -therapy enriched with platelets together with the use of whole erythrocyte mass) which restores the interrupted connection between the fragments, reducing the time of the reparative process.3. Autoosseous grafting, being the gold standard for filling bone cavities, is practically applicable for defects larger than 1 cm. For larger defects (3 cm fistula) of the metaphyseal zone, it is better to use a combination of the method with the technique PRPtherapy enriched with platelets in conjunction with the use of whole erythrocyte mass.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML