-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(4): 347-350
doi:10.5923/j.ajmms.20231304.01
Received: Feb. 12, 2023; Accepted: Mar. 6, 2023; Published: Apr. 13, 2023

Results of Coronary Artery Stenting in Elderly People with Chronic Heart Failure
Yarasheva Zarrina Hikmatillaevna1, Ismoilova Yulduz Abduvohidovna1, Yusupov Tokhir Shomirza Ugli2
1Samarkand State Medical University, Samarkand, Uzbekistan
2Regional Branch of the Republican Specialized Cardiology Scientific and Practical Medical Center Samarkand, Uzbekistan
Correspondence to: Yarasheva Zarrina Hikmatillaevna, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective. To evaluate the benefits of percutaneous coronary intervention (PCI) in reducing NT-proBNP and increasing left ventricular ejection fraction in elderly patients. Materials and methods. The study included patients aged 60-74 years (mean age 63.46±3.29 years) who underwent coronary artery stenting in patients diagnosed with postinfarction cardiosclerosis (PICS) - 40% (n=32), with subacute myocardial infarction 42.5% (n=34), unstable angina FC 3-4 17.5% (n=14). An assessment was made of the nature of postoperative changes in echocardiographic values, the level of NT-proBNP. Results. The study found that in elderly patients who underwent coronary artery stenting, there was a significant increase in left ventricular ejection fraction, NT-proBNP level in patients with PICS, subacute MI, compared with patients with unstable angina pectoris. Conclusion. The issue of coronary artery stenting in elderly patients should be carefully discussed, especially when there is a comorbid pathology. It is necessary to conduct studies aimed at long-term observation of patients after percutaneous coronary intervention, as well as to confirm or exclude chronic heart failure in all patients to study the level of natriuretic peptide.
Keywords: Chronic heart failure, Percutaneous coronary intervention, Coronary artery stenting, Echocardiography, Natriuretic peptide
Cite this paper: Yarasheva Zarrina Hikmatillaevna, Ismoilova Yulduz Abduvohidovna, Yusupov Tokhir Shomirza Ugli, Results of Coronary Artery Stenting in Elderly People with Chronic Heart Failure, American Journal of Medicine and Medical Sciences, Vol. 13 No. 4, 2023, pp. 347-350. doi: 10.5923/j.ajmms.20231304.01.
1. Introduction
- Coronary artery disease (CHD) is widespread among patients with heart failure (HF) and accounts for almost two-thirds of cases. The use of percutaneous coronary intervention (PCI) in patients with CAD has increased markedly, and numerous observational studies have suggested that it is associated with improved patient outcomes [3,5]. There are no randomized data comparing the impact of PCI on clinical outcomes and myocardial deremodeling in patients with coronary artery disease with coronary artery stenting or modern drug therapy aimed at compliance [1,4,8]. There is evidence of the effect of PCI in acute MI (with and without acute coronary syndrome), chronic CAD with reduced ejection fraction, and MI with preserved ejection fraction. Randomized clinical trials with sufficient confirmation are needed to study the outcomes of PCI in these various populations of patients with coronary artery disease [2,6,7,9].RelevanceIschemic heart disease (CHD) remains the most common cause of heart failure (HF) in Uzbekistan, accounting for 60% to 70% of cases [1,3]. Coronary artery bypass surgery (CABG) is and remains in recent years the main method of treatment of multivessel coronary artery disease with concomitant left ventricular systolic dysfunction (LVSD) for several decades [4,5]. However, at present, advanced and complex multivessel percutaneous coronary interventions (PCI) using the latest antiplatelet therapy and percutaneous mechanical circulatory support, the impact of PCI on patients with acute and chronic heart failure with reduced ejection fraction (HFEF), as well as heart failure with preserved fraction emissions (HFpEF) has become a subject of increased interest.American studies reported that after revascularization in stable CAD with severe LV EF, an increase in LV EF was observed in 50% of patients [6,7]. Pooled data from the PROTECT II registry (a prospective, multicenter, randomized, controlled trial of the IMPELLA RECOVER LP 2.5 system versus an intra-aortic balloon pump in patients undergoing high-risk elective PCI) and the cVAD (ventricular assisted catheter devices) registry showed that 57% of patients after PCI with hemodynamic support, there was an improvement in LV EF by at least 5% [8]. Mean LVEF improved from 25% to 31% after PCI (6.5% net increase p < 0.001), and greater improvement in LVEF was directly correlated with more vessels treated [8]. One small study of revascularized patients with stable CAD, reduced LV EF and no implantable cardioverter defibrillator (ICD) found that 56% of these patients were no longer candidates for an ICD based on improved LV EF at follow-up [7,11]. In the PROTECT II sub study, 51% demonstrated reverse LV remodeling with an absolute increase in LVEF of 13% (p<0.001) and a decrease in end-systolic volume [6]. Reverse LV remodeling occurred more frequently in patients with more extensive revascularization (RR: 7.52; 95% CI: 1.31–43.25) and was associated with significantly fewer major adverse cardiovascular and cerebrovascular events (9.7% vs 24.2%, p ¼ 0. Pooled data from Protect II and the cVAD registry showed that more treated vessels were independently associated with greater improvement in LVEF (5.5% improvement in LVEF with 1 vessel treatment, 6.6% with 2 vessel treatment, 8.3% for 3-vessel treatment [p for trend ¼ 0.046]) [8]. Data from the CHART-2 study (Chronic Heart Failure Analysis and Registry in the Tohoku District-2) demonstrated that in patients with symptomatic heart failure and a history of PCI, approximately two-thirds of patients had residual stenosis (defined as the presence of residual ≥70% neovascular stenosis) [9]. Patients with residual stenosis had a higher all-cause mortality than those without, even after density matching (21.9% vs. 11.6%; log-rank p ¼ 0.027). Residual stenosis was independently associated with all-cause mortality in patients with ischemic heart disease (HR: 1.62; 95% CI: 1.07–2.46; p ¼ 0.024) [9,10]. Complete revascularization in patients with HF can sometimes be technically challenging. In patients with HFrEF, failure of a total revascularization attempts due to hemodynamic instability, difficulty in performing chronic total occlusion (CTO), presence of non-dilated lesions, or procedural complications was associated with higher rates of short-term and long-term major adverse cardiac events compared with successful total revascularization and selective incomplete revascularization [10,11]. Complete revascularization in patients with HF can sometimes be technically challenging. In patients with HFrEF, failure of a total revascularization attempts due to hemodynamic instability, difficulty in performing chronic total occlusion (CTO), presence of non-dilated lesions, or procedural complications was associated with higher rates of short-term and long-term major adverse cardiac events compared with successful total revascularization and selective incomplete revascularization [10,11]. Complete revascularization in patients with HF can sometimes be technically challenging. In patients with HFrEF, failure of a total revascularization attempts due to hemodynamic instability, difficulty in performing chronic total occlusion (CTO), presence of non-dilated lesions, or procedural complications was associated with higher rates of short-term and long-term major adverse cardiac events compared with successful total revascularization and selective incomplete revascularization [10,11].Target: To evaluate the benefits of percutaneous coronary intervention (PCI) in reducing NT-proBNP and increasing the left ventricular ejection fraction in elderly patients.
2. Materials and Methods
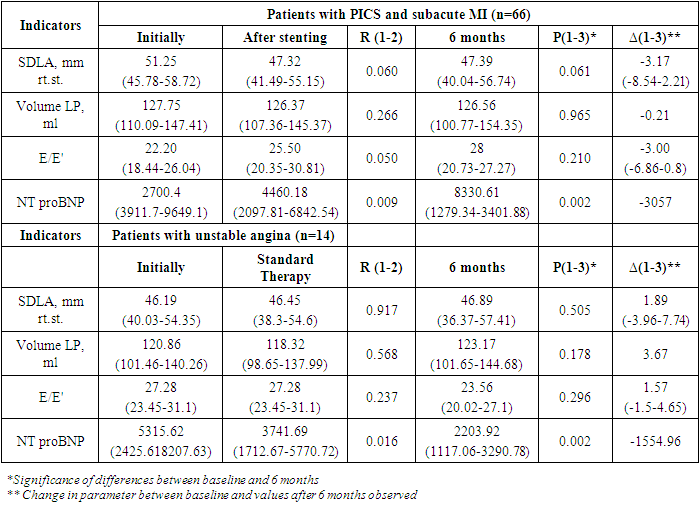
- We analyzed elderly patients who underwent PCI from September 1 to March 1, 2022 according to the data of the Samarkand Regional Branch of the Republican Specialized Scientific and Practical Medical Center for Cardiology. A total of 80 patients were analyzed, who underwent interventional intervention (PCI) with a radial approach 58.75% (n=74) and other approaches 3.68% (n=6). Men accounted for 68.1% (n=43), women 31.9% (n=37). The mean age was 63.46.Before PCI, all patients were examined by a cardiologist and prescribed general and biochemical blood tests, blood NT-proBNP levels, ECG, echocardiography, chest x-ray, and coronary angiography. The main part of the patients was diagnosed with coronary artery disease: postinfarction cardiosclerosis (PICS) - 40% (n=32), with subacute myocardial infarction 42.5% (n=34), unstable angina FC 3-4 17.5% (n= fourteen). The distribution of patients by diagnosis is shown in diagram № 1.
 | Diagram 1. Distribution of patients by diagnosis |
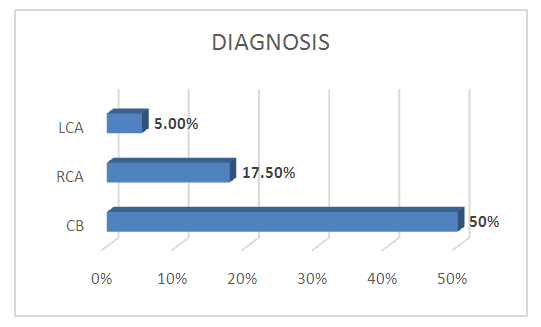
 | Diagram 2. Damage to the branches of the coronary vessels |
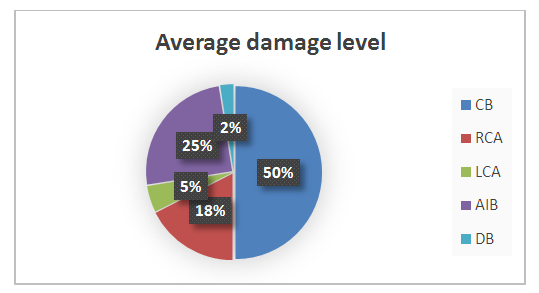
 | Diagram 3. Types of stenting |
|
3. Results
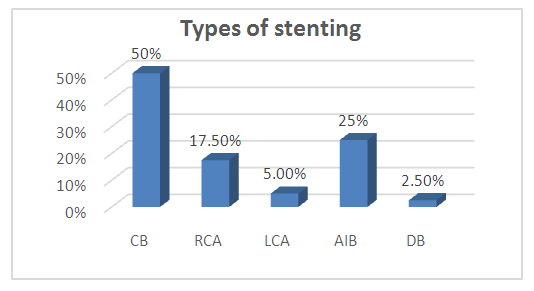
- The study found that in elderly people with a diagnosis of coronary artery disease: postinfarction cardiosclerosis (PICS) - 40% (n=32), with myocardial infarction 42.5% (n=34), angina pectoris FC 3 17.5% (n=14). From diagram No. 2, it can be seen that the circumflex branch is most affected in 40 patients, the average level of damage was 80%, the anterior interventricular branch (LAB) - 20 (25%), in which the average level of damage is 70%, 14 patients are affected by the right coronary artery (RCA), which amounted to 70% of the average level, in 49 patients the obtuse marginal branch (OBB) was affected, which amounted to 69%, the diagonal branch (DV) was affected in 2 patients and amounted to 78%, who underwent stenting of the coronary arteries there is a significant increase in LV EF and the level NT proBNP.It is necessary to study the comparative long-term follow-up of patients diagnosed with postinfarction cardiosclerosis in the elderly - 32 patients (40.0%), patients with acute myocardial infarction underwent stenting in 14 patients, which amounted to 8.6%. Various types of stenting were also involved - recanalization of an occluded coronary artery in 30.67% of patients, balloon angioplasty in 42.33% of patients, in other patients stenting of various sections of the coronary arteries. All patients before and after PCI were prescribed statins, in particular, rosuvastatin - mertenil at a dose of 20 mg/day, double or triple anticoagulant therapy - acetylsalicylic acid and clopidogrel, or enoxaparin (rivaroxaban).After stenting, the patients were in the hospital under observation and no angina pectoris attacks were observed in patients before discharge from the hospital.
4. Discussion
- Comparative long-term follow-up of elderly patients is to be studied. The importance of stenting in elderly patients with CIHD, who have a high level of comorbidity, is likely to be quite high, while the need for stenting in patients who have had myocardial infarction with postinfarction cardiosclerosis raises many questions. It is necessary to study the presence of early chronic heart failure in these patients to address the issue of the need for coronary artery stenting and improve the quality of life.
5. Findings
- Currently, interventional surgery, which includes coronary artery stenting, balloon angioplasty and coronary artery bypass grafting, are at the peak of treatment for patients with coronary heart disease. However, a more careful selection of comorbid patients should be carried out taking into account age, patients with complicated chronic heart failure, for whom it is important to study the level of brain natriuretic peptide, as well as long-term monitoring of the outcomes of surgical intervention.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML