-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(3): 338-343
doi:10.5923/j.ajmms.20231303.29
Received: Mar. 15, 2023; Accepted: Mar. 25, 2023; Published: Mar. 28, 2023

The Role of Vitamin D in the Course of Heart Failure in Patients with Coronary Artery Disease and Type 2 Diabetes
Alimova D. A.1, Mukhtarova Sh. Sh.2, Trigulova R. Kh.1, Shek. A. B.1, Abdullaeva S. Ya.1
1State State Institution Republican Specialized Scientific and Practical Medical Center of Cardiology of the Ministry of Health of the Republic of Uzbekistan Tashkent, Uzbekistan
2Tashkent Pediatric Medical Institute of the Ministry of Health of the Republic of Uzbekistan Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Aim: to study the relationship between the level of vitamin D, the level of glycated hemoglobin, and the course of heart failure in patients with coronary artery disease and type 2 diabetes. Materials and methods. In this study, 130 patients with coronary heart disease with type 2 diabetes with no signs of large-focal myocardial infarction less than three months ago, patients with severe complications of diabetes, life-threatening cardiac arrhythmias, acute cardiovascular insufficiency, and severe impaired liver and kidney function were examined. Results. A close direct correlation was found between the level of vitamin D in the blood (both deficiency and insufficiency) with higher parameters of brain natriuretic peptide and left ventricle isovolumetric relaxation time), in patients with a persistent HbA1 level> 8.1 during the observation period, which is evidence of ventricular diastolic dysfunction worsening and heart failure progression.
Keywords: Ischemic heart disease, Diabetes mellitus, Vitamin D, Heart failure
Cite this paper: Alimova D. A., Mukhtarova Sh. Sh., Trigulova R. Kh., Shek. A. B., Abdullaeva S. Ya., The Role of Vitamin D in the Course of Heart Failure in Patients with Coronary Artery Disease and Type 2 Diabetes, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 338-343. doi: 10.5923/j.ajmms.20231303.29.
Article Outline
1. Introduction
- Type 2 diabetes mellitus (DM) is an independent risk factor for the development of heart failure and cardiovascular complications. Approximately 80% of diabetic patients die from cardiovascular disease. It is known that heart failure occurs 4 times more often in men and 8 times more often in women with type 2 diabetes at the age of 65 than in the general population [1]. Annually, heart failure develops in 3.3% of patients with type 2 diabetes who had no signs of heart failure initially [2]. In the SOLVD (Studies on Left Ventricular Dysfunction) study, diabetes was identified as an independent risk factor for death [3].Vitamin D, in addition to its main function in calcium phosphate metabolism [4-7], has various effects on the growth, development and differentiation of various cell types, as well as protective, regenerative, anti-inflammatory and immunomodulatory properties [4,5]. Moreover, vitamin D is involved in more than 20 different metabolic processes in the body, being an essential element and regulator of the main types of metabolism [6].In type 2 diabetes mellitus (T2DM), vitamin D can affect both insulin secretion and sensitivity. An inverse relationship between T2DM and vitamin D has been postulated by cross-sectional and prospective studies. [8,9]In this regard, further study of the role of vitamin D and calcium in the prevention and treatment of type 2 diabetes is needed to elucidate the relationship between vitamin D and glucose homeostasis in type 2 diabetes.Aim: to study the relationship between the level of vitamin D, the level of glycated hemoglobin, and the course of heart failure in patients with coronary artery disease and type 2 diabetes.
2. Materials and Methods
- We examined 130 patients with coronary artery disease with type 2 diabetes. The patients were hospitalized at the Republican Specialized Scientific and Practical Medical Center for Cardiology (RSNPMCC).Inclusion criteria: stable angina pectoris, BMI 25 kg/m2 and above; HbA1c from 7.0 to 10.0% (53–86 mmol/mol) against the background of antidiabetic drugs (insulin, metformin) with a stable dosage within 3 months before the start of the study; BP<150/85 mmHg stable for at least 1 month during therapy. Written consent was taken from each patient for the processing of his data for scientific purposes.Exclusion criteria: severe cardiac, renal and hepatic failure; gastric bypass; chronic or previous acute pancreatitis; pregnant or lactating women, as well as the refusal of the patient to participate in the study.The average duration of IHD in the examined patients was 9.69±0.49 years, the average duration of DM-2 among the identified patients was 7.3±3.89 years. The presence of concomitant pathology was judged on the basis of an analysis of medical records and the results of an inpatient examination of patients.All patients received conventional basic therapy, including acetylsalicylic acid (ASA), beta-blocker bisoprolol 2.5–5 mg/day, an ACE inhibitor, rosuvastatin 20 mg/day, and metformin. Observations were made throughout the year.The patient examination protocol included the following:• questioning (complaints, anamnesis), physical examination, with an assessment of the functional class of angina pectoris according to NYHA• Analysis of electrocardiogram in 12 leads• Evaluation of hemodynamic parameters, function and state of the myocardium using transthoracic echocardiography (EchoCG, with assessment of LVDD)• laboratory research methods (clinical blood test, lipidogram, coagulogram, biochemical blood test, glycated hemoglobin, C-reactive protein, prothrombin index, vitamin D, natriuretic peptide)Statistical data processing was carried out using the programs STATISTICA 10 (TIBCO, USA) and MedCalc 18.6 (MedCalc software, Belgium). The significance level of α was considered to be 5%; to assess statistical significance, the p-value and/or 95% confidence interval were calculated.
3. Results
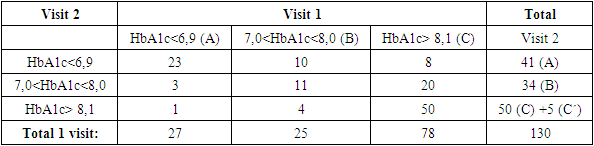
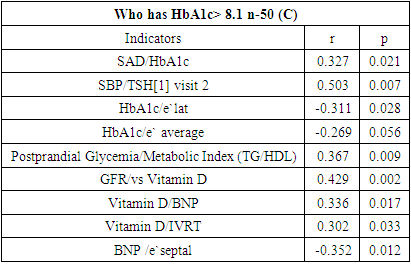
- We analyzed the patient data obtained as a result of HbA1c "turning" with their further distribution depending on the achieved level. In this regard, the distribution of patients into subgroups at 1 visit was: A n-27; In n-25; C n-78, and after 2 years of observation it became the following: A n-41; In n-34; C n-55 (Table 1).
|
|
|
|
|
4. Discussion
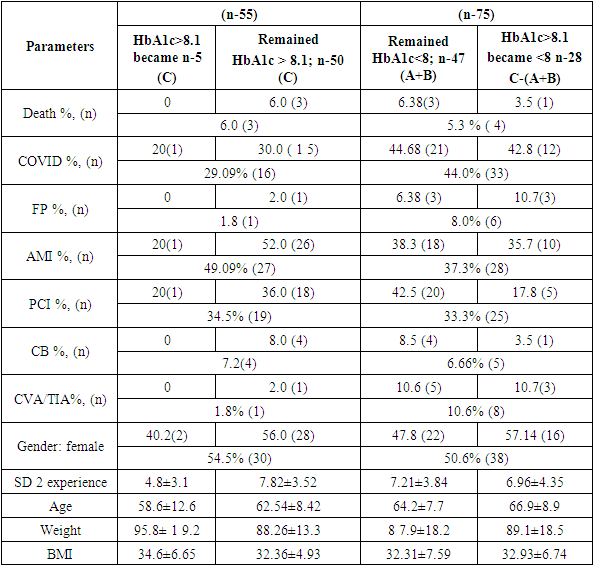
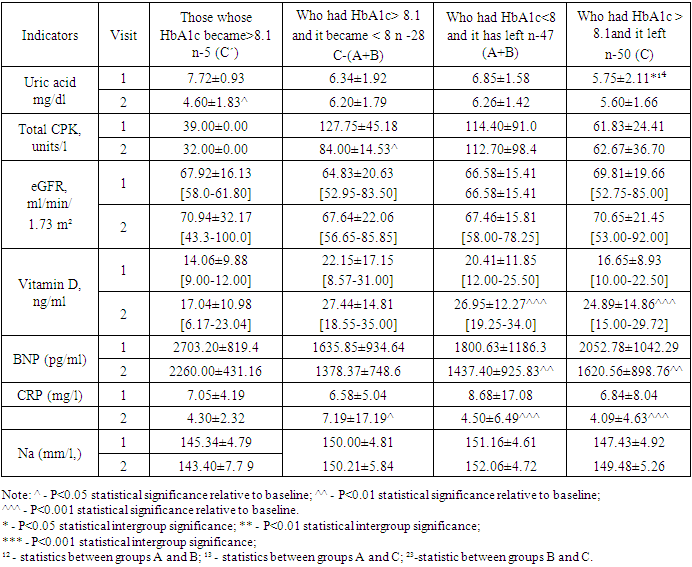
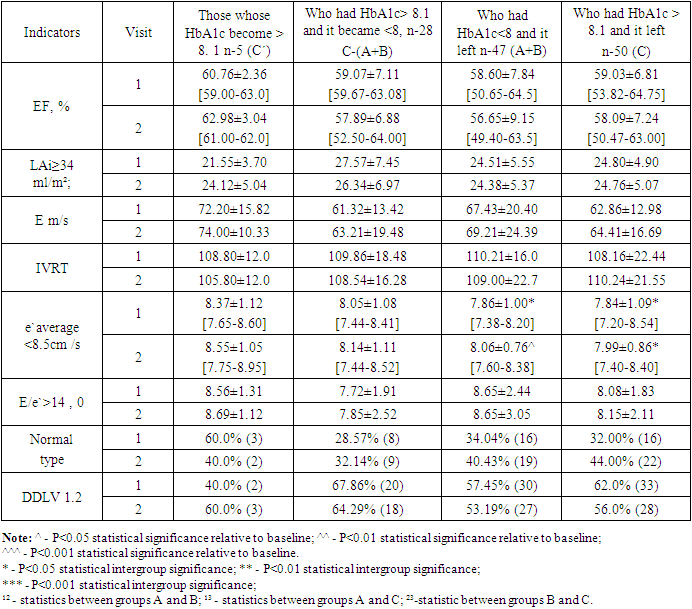
- A two-year evaluation of HbA1c dynamics showed that in patients included in the analysis, variants of alternating its target values are recorded. In 75% of cases, there is a stable maintenance of the HbA1c level with its various target values, in particular, in 38.4% of cases >8.1% and 36.15% -<8%.The number of patients who survived COVID is higher in the group with HbA1c<8 and 2.2 times more often in the "transitions" of patients. The frequency of occurrence of paroxysms of AF and stroke (TIA) increases with a decrease in HbA1c during observation, but in AF it depends on HbA1c transitions, while in stroke there is no such dependence. In our observation, the incidence of AMI, PCI, CABG had no direct relationship with the level of HbA1c and its transitions.The earliest preclinical manifestation of diabetic cardiomyopathy is left ventricular diastolic dysfunction (LVDD), which, when progressing, can lead to the appearance of clinical symptoms of chronic heart failure. According to Boyer J.K. et al, the prevalence of LVDD among patients with type 2 diabetes mellitus (DM) without clinical signs of heart disease reaches 75% [10].A close direct correlation was found between the level of vitamin D in the blood (both deficiency and insufficiency) with higher parameters of BNP and IVRT (LV isovolumetric relaxation time), in patients with a persistent HbA1 level> 8.1 during the observation period, which is evidence of worsening LVDD and progression of heart failure. At the same time, it is worth remembering the cardiorenal syndrome, which describes the negative impact of declining kidney function on the heart and blood circulation [11-13]. According to the research results of Kharlamov et al., as well as Artaza J.N. et al., Ojo A.O and Tishkoff D.X et al, Vitamin D, in particular its activated form 1,25(OH)2D3, being involved in various pathophysiological cascades, including inflammation, fibrosis and reparative mechanisms that ensure the functional and structural preservation of the kidney and myocardium can reduce the progression of the cardiorenal syndrome [14-17]. Confirmation of the influence of renal function on the deterioration of LVDD may be the presence of a direct correlation between vitamin D and eGFR (r=0.429; p=0.002). It was found that in the group of patients with HbA1c> 8.1, there was a decrease in the level of uric acid ∆ 3.12 mg/dl (p=0.02), CPK Δ 30.0 U/l (p=0.0135).Negative dynamics of the e`average index was revealed in the HbA1c<8 (n-47) and HbA1c>8.1 (n-50) groups after 2 years of observation with significant differences between the points of determination, in contrast to the subgroups in which HbA1c transitions were observed. The E/e` ratio in all groups showed a tendency to increase throughout the entire observation period, which indirectly indicates the progression of diastolic dysfunction.
5. Conclusions
- 1. A close direct correlation was found between the level of vitamin D in the blood (both deficiency and insufficiency) and higher BNP and IVRT parameters in patients with a persistent HbA1 level> 8.1 during the observation period.2. There is a direct correlation between vitamin D and eGFR, which confirms the influence of renal function on the deterioration of LVDD.
ACKNOWLEDGEMENTS
- The authors thank all the staff and all medical personnel involved in the creation of this work.
Conflict of Interest
- The Authors declaire no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML