-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(3): 330-337
doi:10.5923/j.ajmms.20231303.28
Received: Mar. 8, 2023; Accepted: Mar. 17, 2023; Published: Mar. 28, 2023

Treatment and Prevention of Dorsalgia in Workers Automotive Complex
Mirjuraev E. M., Zuxritdinov U. Yu., Akilov D. X.
Center for the Development of Professional Qualifications of Medical Workers under the Ministry of Health of the Republic of Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

We studied 110 patients with dorsopathies aged 25 to 50 years, the average age was 38.1±1.0 years. Of these, 70 patients (main group) were workers of the automotive industry complex (AIC) and 50 patients (control group) who applied to the clinic and did not work in the AIC. The main inclusion criterion was the presence of chronic pain syndrome (more than 3 months) in the lower back of vertebrogenic origin. All patients were divided into 2 equal groups. The first group (50 patients) was treated traditionally - NSAIDs, vitamins, muscle relaxants, massage. The second group (70 patients) received traditional treatment and diadynamic electrical neurostimulation with the DENAS-Vertebro device, daily for 30 minutes, for a course of 10 procedures. According to the results of treatment in the group of patients who received DDENS in the complex treatment, the outcome of the treatment was much better.
Keywords: Dorsalgia, Dorsopathy, Back pain, Electrical nerve stimulation, Auto industry workers
Cite this paper: Mirjuraev E. M., Zuxritdinov U. Yu., Akilov D. X., Treatment and Prevention of Dorsalgia in Workers Automotive Complex, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 330-337. doi: 10.5923/j.ajmms.20231303.28.
Article Outline
1. Introduction
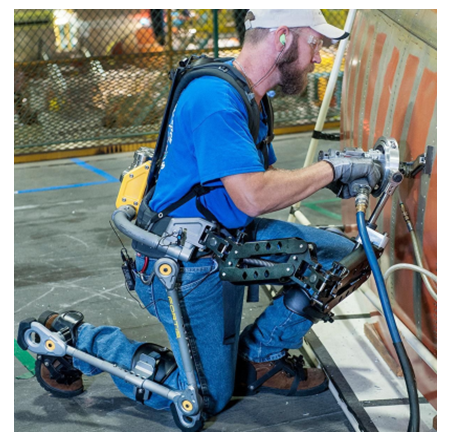
- According to the World Health Organization (WHO), “Low back pain is a common global problem. The point prevalence of low back pain in 2017 was about 7.5% of the global population, or about 577.0 million people” [18]. “In European countries, the cost associated with low back pain is up to 2% of the gross domestic product” [17]. Low back pain is pain in the back from the lower edge of the twelfth rib to the lower gluteal folds, lasting at least one day. Currently, back pain (BP) is the most common cause of temporary disability in people aged 20 to 60 years. “Although less than 28% of people with low back pain have a severe disability, they account for 77% of all disabilities caused by low back pain” [11]. This determines the medical, social and economic significance of the problem.Pain in the lumbar region is one of the main reasons for applying to a specialist and obtaining a disability certificate in people of different ages [2]. In Europe, this reason is the second most frequent visit to a doctor [15].According to statistics, 80% of the world's population suffers from back pain. One third of the population (28.4%) aged 18–70 years experience recurrent back pain, 89% had a relatively long episode of back pain at least once in their lifetime [15,18]. In the United States, back pain ranks first in the structure of rheumatic diseases among the adult population. Pain in the lumbar region is one of the main reasons for consulting a specialist and obtaining a disability certificate in people of different ages. In Europe, this reason is the second most frequent visit to a doctor [15].According to the definition of the International Association for the Study of Pain (IASP): “Pain is an indefinite sensation and emotional experience associated with actual or potential tissue damage, determined by sensory information, affective reactions and cognitive activity” [19,23].Pain is in itself an adaptive reaction of the body, which is presented as an alarm signal. On the one hand, the feeling of pain is conditionally beneficial for the body, since it performs an important physiological function - protecting the human body from excessive damage [8].Physiologists, clinicians, psychologists classify pain in this way:• primary and secondary;• acute and chronic (more than 6 weeks);• stabbing, burning, dull (visceral);• physical and psychogenic (sometimes they can exist simultaneously [19].Psychogenic pain is associated with psychological or social factors. Such pain occurs against the background of various mental disorders - depression, phobias, hysteria, psychosis [8].Physical pain is divided into categories:• pain caused by external influences;• pain caused by internal influences (according to European researchers, such pain is divided into ecto-, meso-, endodermal and pain that occurs from excessive muscle load);• pain associated with damage to the nervous system, especially its afferent apparatus.As a result of numerous studies, it has been established that pain is not only subcortical (thalamic), but also cortical in nature, although definitive evidence regarding the localization of the code ending of the pain analyzer has not yet been obtained [8].There are two systems in the pathogenetic cascade of pain: the pain system itself (nociceptive) and the antipain system (antinociceptive).The structure of the pain system includes:• opiate receptors (found in the posterior horns of the spinal cord, the nuclei of the thalamus, hypothalamus, reticular formation);• serotonergic system;• adrenergic mechanism [8].The basis of the pathogenetic classification of pain, which is very important in the work of a doctor for the selection of adequate therapeutic tactics, is the allocation of the main mechanism of its formation.Types of pain syndrome1. Somatogenic - is formed during trauma, inflammation, ischemia. Options: post-traumatic, postoperative, joint inflammation, vertebrogenic, myofascial pain syndrome, vascular pain, pain in oncological pathology, angina pectoris, gallstone and kidney stone disease.2. Neurogenic - occurs when the peripheral or central structures of the nociceptive system are damaged, which leads to the formation of persistent aggregates of hyperactive neurons. Options: neuralgic pain, thalamic pain, phantom pain syndrome, causalgia.3. Psychogenic - the mechanism of this type of pain syndrome is based on the formation of muscle spasm. Option: tension headache.The main triggers of pain in the lumbar region are muscular-tonic syndrome due to degenerative-dystrophic changes in the spine (osteochondrosis and spondylosis) and myofascial syndrome [8,19].There are such clinical types of back pain.1. Local - occurs when exposed to sensitive nerve endings. The pain in this case is predominantly constant and is localized in the area of the spinal lesion.2. Projection - has options: it is projected from the spine to the lumbosacral region, it is projected from the organs of the abdominal cavity and small pelvis to the spine.3. Radicular (radicular) - pain of a pronounced nature, aggravated by movement, mainly radiates to the lower extremities.4. Pain due to muscle spasm - in 50% of cases, back pain is associated precisely with muscle spasm [19].When analyzing the primary referral to general practitioners for acute pain in the lumbosacral region, its causes (musculoskeletal pain) are detected in the vast majority of patients - in 70% of cases. Discogenic pain and pain associated with dysfunction of the facet joints is observed in 20% of patients with acute back pain [4,22]. In 5–10% of cases, as a result of compression complicating osteochondrosis, the latter is clinically manifested as radiculopathy; in 1% it is manifested by life-threatening diseases that require urgent treatment (oncological, infectious diseases, traumatic injuries) [24].When diagnosing back pain in each case, the doctor must remember that the cause is not always associated with the pathology of the spine. The mechanism of back pain on the basis of these etiological factors is associated with its projection into the dermatome innervated by the same segment that is involved in the pathological process of the affected internal organ [10]. In 8-10% of cases, the so-called referred back pain occurs. Its etiological factors can be:• diseases of the cardiovascular system (ischemic heart disease, myocardial infarction, thromboembolism of the pulmonary artery and its branches);• respiratory diseases (pneumonia, pleurisy);• kidney disease;• gynecological pathology;• diseases of the digestive system (peptic ulcer, cholecystitis, pancreatitis).Among the vertebrogenic causes of back pain, there are: protrusion of the intervertebral disc, osteophytes, instability of the spinal motion segment, subluxations, arthrosis, spinal fracture, osteoporosis, osteoarthritis, metastases to the vertebral bodies, functional vertebrogenic disorders.It should be emphasized once again that the main cause of back pain is the result of age-related degenerative-dystrophic processes in the intervertebral discs and the musculoskeletal apparatus of the spine [4,22].Back pain syndromes are divided into primary and secondary.The primary syndromes include osteochondrosis and spondylarthrosis. Functionally reversible blocking of the intervertebral joints is of great importance.Secondary syndromes include:• tumors and metastases in the vertebrae, spinal cord;• vertebral fractures;• infectious and specific lesions of the vertebrae and intervertebral discs;• non-communicable inflammatory diseases;• metabolic lesions of bones;• acute disorders of spinal circulation;• reflected pain in the pathology of the pelvic organs [26].The peak of back pain complaints occurs between the ages of 30 and 50. Women are predominantly affected. Primary changes and initial clinical manifestations are noted at 20–25 years of age [4,22].In the elderly, the main cause of back pain is spondylarthrosis, when the degenerative process is localized in the intervertebral joints [1].Often, back pain occurs when an intervertebral disc herniates, mainly at the level of L4–L5, L5–S1 [26].Radiculopathy is a complication of osteochondrosis and herniated discs. The occurrence of radiculopathy is associated with microtraumatization of the nerve root by the surrounding tissues, followed by the development of inflammation, ischemia and edema in the nerve root.Radiculopathy develops in the presence of symptoms of prolapse. In its development, it is combined with reflex muscle spasm, which leads to an antalgic posture in the patient [19,26].The cause of back pain is reflex muscular-tonic syndromes of a vertebrogenic nature. Their sources are:• receptors of the fibrous ring;• musculoskeletal apparatus of the spinal motion segment;• capsules of intervertebral joints.Myofascial syndrome involving the muscles of the pelvic girdle and lower extremities occurs due to:• prolonged stay in a non-physiological position;• overload of untrained muscles;• diseases of the digestive system and small pelvis [20].In assessing the neurological deficit in back pain in patients, pain points of the lumbosacral spine should be determined and symptoms of tension in the nerve trunks and roots should be examined. The symptoms of tension of the nerve trunks and roots include: Lasegue's symptom; symptom of Wasserman; Shtryumpel-Matskevich's symptom; Bechterew's symptom 1; Bekhterev-Faerstein's symptom (Lasegue's cross symptom); Sokolyansky test; symptom of Dejerine; Neri's symptom [19].In case of back pain, its objectification, assessment of severity, and intensity control are required [19]. For this purpose, use: visual analog scale (VAS); verbal assessment scale (SVO); the McGill Pain Inventory; Roland-Morris pain questionnaire [19].The VAS scale quantifies pain as a mere sensation and its degree of intensity [19]. To assess the pain syndrome, a short version of the McGill questionnaire with the calculation of the rank index of pain is used. This scale allows you to measure the sensory, emotional, quantitative components of the pain syndrome of a particular patient [19].The Roland-Morris questionnaire is used to assess the patient's quality of life [19].Additional research methods for diagnosing back pain1. X-ray examination:• projections - anteroposterior, lateral;• functional spondylogram in the position of maximum flexion and extension.2. Computed tomography (CT) combined with myelography or magnetic resonance imaging (MRI) [6].X-ray manifestations of degenerative-dystrophic changes in the lumbosacral spine include: reduced disc height, subchondral osteosclerosis, formation of osteophytes, calcification of the nucleus pulposus or annulus fibrosus, arthrosis of the intervertebral joints, displacement of the vertebral bodies.When conducting radiography with functional tests, a functional block and / or hypermobility (instability) of individual segments is detected.Degenerative-dystrophic changes in the lumbosacral spine according to CT scan results include: protrusion, disc calcification, vacuum phenomenon, anterior, posterior, lateral osteophytes, central and lateral stenosis of the spinal canal.According to MRI, protrusion of the intervertebral disc, a decrease in the intensity of the signal from the disc, folding of the fibrous ring, a change in the signal from the end plates, a vacuum phenomenon, calcification, and stenosis of the canal can be determined [6].It should be noted that in the course of ongoing studies, the authors did not note a direct relationship between the severity of back pain and the data of additional research methods. About 40% of patients have asymptomatic disc herniations [19].Back pain or changes in the spinal motion segment, as a structural biomechanical unit of the spine, are coded according to ICD-10 in the category of diseases of the musculoskeletal system and connective tissue [M00-M99], dorsopathy block [M40-M54]. In it, osteochondrosis is considered as a disease terminologically associated with the anatomical structures involved in the pathological process, debuting with degeneration or necrosis with an outcome in the form of regeneration or recalcification. In the case of the spine, this process is referred to as deforming dorsopathies and highlighted in section [M42]. Pathological changes and clinical manifestations are classified in the section "other dorsopathy" [M50-M54] and represent the relationship between functional and diagnostic assessments. However, to this heading in ICD-10 include radiculopathy (M54.1). Root pathology also mentioned under M50.1 and M51.1 ("Disorders of the intervertebral discs with radiculopathy"), G54.2-54.4 ("Nerve root and plexuses not classified elsewhere"), G55* ("Compression nerve roots and plexuses in diseases classified elsewhere headings") [12].Pharmacological therapeutic measures for the relief of back pain are diverse [9]. In the acute period, a sparing regimen is created, it is necessary to sleep on a hard bed, apply superficial dry heat. Bed rest is justified only in the initial period of the disease, for a maximum of 2–4 days [19]. The goal of the treatment of acute lumbar pain caused by degenerative-dystrophic changes in the spine and myofascial syndrome is: to relieve pain and return the patient to an active lifestyle; prevent re-exacerbation and chronicity of the process [19].The basis of modern therapy for back pain includes the use of: non-steroidal anti-inflammatory drugs (NSAIDs); painkillers; dehydration agents; antihistamines; physiotherapeutic methods of treatment; orthopedic treatment [19].NSAIDs are the first-line treatment for acute back pain. Basic requirements for NSAIDs:• when administered orally, rapid adsorption in the stomach and intestines and, consequently, the creation of peak plasma concentrations;• a relatively short period of elimination from blood plasma;• long and adequate action;• minimal range of side effects [19].The therapeutic efficacy of NSAIDs is associated with inhibition of cyclooxygenase (COX) activity. COX is a key enzyme in the metabolism of arachidonic acid. Inhibition of COX leads to inhibition of the synthesis of prostaglandin E2, thromboxane A2, a decrease in the level of leukotrienes, kinins, histamine, serotonin and other inflammatory mediators. NSAIDs stimulate lysosomal membranes, while inhibiting the release of enzymes from them, the formation and release of pro-inflammatory cytokines [21].Classification of NSAIDs by selectivityAll drugs in this group are divided into two groups according to the mechanism of action: selective and non-selective. Selective non-steroidal anti-inflammatory drugs that preserve the activity of COX-1 and suppress COX-2 are considered safer for the human body [21].Nonselective NSAIDs. Drugs in this group inhibit both types of cyclooxygenase, while mostly affecting COX-1. This explains the main side effects, such as ulcerative lesions of the gastrointestinal tract, kidney damage.Selective NSAIDs. Preparations of this group of active substances inhibit COX-2 to a greater extent. This reduces the risk of side effects from the gastrointestinal tract.It should be emphasized that if there are indications for the use of NSAIDs for back pain in the elderly, highly selective COX-2 inhibitors (celecoxib, rofecoxib) or selective COX-2 inhibitors (meloxicam) should be used [21]. Drugs of the NSAID group are used individually, with adequate, timely, differentiated dose selection in order to minimize the risk of complications caused by this group of drugs and return the patient to a normal lifestyle as quickly as possible. In the treatment of NSAIDs, there is a risk of side effects, which can occur in 25% of cases [21]. Among the side effects, it is important to note the toxic effect on the alimentary canal: gastropathy, enteropathy, colopathy; kidney complications: interstitial nephritis, nephropathy, glomerulonephritis; rarely - hepatotoxic manifestations [21]. In the treatment of patients with acute back pain, NSAIDs are used in combination with muscle relaxants [21].The action of muscle relaxants is aimed at reducing pain, reducing reflex muscle tension, improving motor function, their use also facilitates the implementation of physiotherapy exercises. This group of drugs includes tolperizole at a dose of 150 mg 3 times a day, a course of 3 weeks. It has a predominantly central effect on reducing muscle tone. It is characterized by a moderate central analgesic and mild vasodilating effect [9].In order to improve microcirculation and venous outflow, patients are prescribed vascular drugs [9].In case of chronic pain in the back and pain associated with depression, the use of antidepressants is recommended [9].In the complex treatment of pain associated with dorsopathy, B vitamins are traditionally used [14]. It has been established that the analgesic effect of B vitamins is associated with inhibition of nociceptive activity in neurons of the posterior horns of the spinal cord and thalamus, increased noradrenergic and serotonergic antinociceptive activity, as well as with inhibition of the synthesis and (or) blocking of the action of inflammatory mediators [25]. A number of studies have revealed a distinct antinociceptive effect of individual B vitamins and their complexes in neuropathic pain. It has been proven that the administration of vitamins B1 and B12 in combination with anticonvulsants (carbamazepine or gabapentin) has a synergistic effect in reducing tactile allodynia. It has been experimentally proven that the activity of nociceptive neurons decreases in a dose-dependent manner with the introduction of vitamin B6 and a complex of other B vitamins, and vitamins B6 and B12 reduce nociceptive activity to a greater extent than vitamin B1 [19].With pain in the lower back, it is possible to use glucocorticoid therapy, which has an anti-inflammatory effect by inhibiting the synthesis of inflammatory mediators. Possible blockade on paravertebral points with the introduction of a 0.5% solution of novocaine with hydrocortisone [19].Physiotherapy methods for dorsalgiaAfter adequate elimination of pain in the back, physiotherapy is used to improve metabolic and trophic processes: galvanization, phonophoresis and drug electrophoresis, diadynamic therapy, amplipulse therapy, magnetotherapy, laser therapy, laser magnetotherapy, mud applications (ozokerite, paraffin, naftalan, etc.), point, segmental, can massage, reflexology, acupuncture, electropuncture, electroacupuncture. If possible, radon, medicinal, mineral and pearl baths, hydrotherapy are prescribed. Methods of physical therapy are used, when certain muscle groups are strengthened and the range of motion is increased with the help of special exercises, as well as methods of psychotherapy [3,5].Given the above, of great clinical interest is the search and application of new non-invasive, affordable, low-cost and effective technologies that would significantly optimize the results of therapy. Dynamic electrical neuroadaptive stimulation (DENAS) is a new method of transcutaneous electrical neurostimulation, which consists in influencing the direct projection of the pathological focus and certain active reflexogenic zones and acupuncture points with short current pulses [5,10,13].Risk factors for back pain can be divided into modifiable, which can be eliminated, and non-correctable (heredity, age, gender).Adjustable risk factors:• professional (heavy physical work, static load on the spine, monotonous physical labor, including frequent forward bends and body turns; work accompanied by vibration processes);• psychosocial (muscle distress caused by being in conditions of acute and (or) chronic stress);• individual somatic features (for example, stoop due to the weakness of the muscular corset and the lack of regular physical education);• individual physical characteristics (unnatural body position, monotonous stereotyped movements, static posture, etc.);• the influence of meteorological factors (local and general hypothermia, pressure drops);• malnutrition, overweight;• Smoking, alcohol abuse.Thus, the factors described above are quite widespread, but can be eliminated, or at least their effect can be limited to the duration of exposure. Against the background of such predisposing factors, hypothermia, awkward movement, and an acute stressful situation are enough to form a pain syndrome [17,22].Swedish researchers [17] compiled a list of factors that can cause back pain that can be observed in any production process:• heavy physical work;• work that requires a long stay in a motionless position;• work requiring frequent tilts or turns of the head and torso;• work requiring energetic movements and heavy lifting;• work that requires constant repetition of the same movements, for example, work on a conveyor;• work related to vibrations.Therefore, in Russia, the rules on labor protection during loading and unloading operations and the placement of goods, in order to preserve the health of workers, set the maximum allowable norms for a single lifting (without moving) of weights: for men, no more than 50 kg; women - no more than 15 kg. In addition, there are additional regulations “On new norms for maximum permissible loads for women when lifting and moving weights manually”, since the specified resolution establishes the norms for lifting and moving weights: when alternating with other work (up to 2 times per hour): men up to 30 kg; women - up to 10 kg; constantly during the work shift: men up to 15 kg; women - up to 7 kg [16].Prevention of dorsalgia at work are:1. Correctly lift weights: do not lift the load sharply, due to the load of the large muscles of the legs, and not the extension of the back (Fig.1).
 | Figure 1 |
 | Figure 2 |
 | Figure 3 |
2. Materials and Methods
- We studied 110 patients with dorsopathies aged 25 to 50 years, the average age was 38.1±1.0 years. Of these, 70 patients (main group) were workers of the automotive industry complex (AIC) and 50 patients (control group) who applied to the clinic and did not work in the AIC. All patients underwent a thorough neurological examination, as well as X-rays, magnetic resonance imaging, ultrasound of internal organs, general tests, and the patients were consulted by a urologist, a general practitioner to rule out lower back pain of non-vertebrogenic origin.The main inclusion criterion was the presence of chronic pain syndrome (more than 3 months) in the lower back of vertebrogenic origin. All patients were divided into 2 equal groups. The first group (50 patients) was treated traditionally - NSAIDs, vitamins, muscle relaxants, massage. The second group (70 patients) received traditional treatment plus DDENS with the DENAS-Vertebro device, daily for 30 minutes, for a course of 10 procedures.According to the criteria of the MacNab scale (which, although they were first published back in 1971, are widely used to assess the outcomes of surgical treatment of vertebrogenic pathology, we used it to assess the outcome of conservative treatment, in which 4 possible treatment outcomes are distinguished: • excellent - no pain and restrictions mobility, return to previous work and previous level of activity; • good - rare/periodic non-radicular pain, decrease in the severity of existing symptoms, return to work with minor restrictions; • satisfactory - some increase in functional activity, the patient remains disabled / bedridden; • poor - symptoms of root compression persist, repeated treatment or surgery is necessary.
3. Results and Discussion
- When analyzing the demographic indicators of the AIC workers and patients of the control group, the absence of statistically significant differences in age (mean age 37.5±2.5 and 38.4±2.7 years), height, weight (p<0,05), which confirms the comparability of the compared groups of patients. There were also no differences in gender, since we deliberately excluded women from the comparison group, since men predominated among AIC workers.Along with this, a statistically significant difference in the age of onset of the disease with an earlier development of pain syndromes in the back in AIC workers attracts attention. Exacerbations of the disease were also statistically more common among AIC workers (p<0.05),To determine the features of the clinical picture of dorsopathies in the analyzed groups of patients, we identified all the symptoms characteristic of lumbodynia of various origins. The clinical picture of the main neurological manifestations in the two groups of patients did not generally differ. At the same time, attention is drawn to the predominance of the average values of almost each of the neurological signs in AIC workers when compared with the control group, but in most symptoms - without statistical significance. This applies to a large list of symptoms of damage to the sensory and motor-reflex spheres, such as: decreased surface sensitivity L5, the presence of paresthesia L2 - L4, the presence of the Wassermann and Lassegue symptom, weakness in the muscles along the roots of L5, the presence of muscle hypotrophy along the root L2 - L4, S1, decreased Achilles reflex (p<0.05). At the same time, some indicators: the severity of scoliosis, pain on palpation of the spinous processes of the lumbar spine and pain on palpation of the paravertebral points had a statistically significant predominance in AIC workers (p<0.05). In our opinion, the peculiarities in the clinical picture of dorsapathies in AIC workers can be explained by their professional activities associated with physical labor and weight lifting.The analysis of the results of treatment according to the MacNab scale after the treatment showed the following results:In the control group: excellent - in 7 (14%) patients, good - in 20 (40%) patients, satisfactory - in 21 (42%) patients, poor - in 2 (4%) patients.In the main group: excellent - in 20 (28.6%) patients, good - in 38 (54.3%) patients, satisfactory - in 12 (17.1%) patients, poor - no.As can be seen from the above data, in the second group of patients who received DDENS in the complex treatment, the outcome of the treatment was much better. This is due, in our opinion, to the fact that diadynamic electrical nerve stimulation has analgesic, antispasmodic, anti-inflammatory, trophic-stimulating effects.Diadynamic electrical neuroadaptive stimulation (DENAS) is a new method of transcutaneous electrical neurostimulation, which consists in influencing the direct projection of the pathological focus and certain active reflexogenic zones and acupuncture points with short current pulses that constantly react with the transformation of their shape to changes in skin resistance in the subelectrode zone. Due to this, the phenomenon of accommodation (addiction to procedures) does not develop and there are practically no contraindications. The portability of DENAS devices and autonomy of power supply makes it possible to quickly move the electrodes to different areas during a treatment session and use an external therapeutic electrode for the same purpose [2].Explanatory work was carried out among the workers of the automotive industry complex on the prevention of back pain at work.Prevention of back pain at work are:1. Correctly lift weights: do not lift the load abruptly, due to the load of the large muscles of the legs, and not the extension of the back.2. Wearing a support belt (lumbosacral corsets).3. Maintain a healthy weight. Overweight people are at greater risk of back pain, joint pain and muscle tension than those who are not overweight.4. Rest and sleep in a position that maintains the natural alignment of the spine.5. Maintain good posture. Correct posture and body mechanics result in less pressure on the intervertebral discs and less stress on the muscles, ligaments and joints of the back.6. Reducing stress and the prerequisites for its occurrence. Stress increases tension in all muscles, including those in the back.7. Keep the spine and joints flexible. Sports, swimming, yoga.During the year, the medical unit monitored the production of patients who applied with back pain. According to the anamnestic data, the causes of the development of back pain were identified and, on the basis of this, the effectiveness of the preventive measures we carried out among workers was determined.Uzavtomotors Asaka has 8,860 employees. According to the card file of the medical unit for 2018-2020, there were 4280 calls from workers with back pain to the medical unit (an average of 1416 calls per year). After the explanatory work on the prevention of back pain for 9 months of 2019, 320 employees applied to the medical unit with back pain. Of these, there were 195 men and 125 women. The average age was 38.5±1.2 years. According to the anamnesis, it was revealed that among the factors in the development of back pain, work with a significant static and dynamic load on the muscles of the trunk, legs and arms was distinguished - in 77 (24.1), as well as the lifting and moving of gravity, as well as its total mass being lifted. load - in 80 (25%), frequent and deep torso bending, twisting of the torso during work - in 79 (24.7%), forced working posture, including prolonged sitting with an unchanged working posture - in 57 (17, 8%), as well as the impact of general vibration - in 32 (10%). In addition, hypothermia was noted as a provoking risk factor in 75 (23.4%) patients and chronic stressful situations in 50 (15.6%) patients.It turned out that among 320 patients who applied to the medical unit, 301 (94.1%) did not comply with preventive measures. The remaining 19 (5.9%) observed preventive measures, but the exacerbation of back pain did not occur at work.
4. Conclusions
- 1. The clinical picture of dorsopathy in workers of the automotive complex, in comparison with the control group, reveals features in the form of an earlier development of dorsalgia and frequent exacerbation of the disease, as well as more pronounced scoliosis of the spine, soreness of the spinous processes and paravertebral points.2. The use of diadynamic electrical nerve stimulation in the complex treatment of lumbosacral dorsopathies has shown its effectiveness, has made it possible to achieve rapid relief of the pain syndrome, and therefore it can be recommended for wider use in outpatient practice.3. Compliance by employees with a set of preventive measures for back pain at work reduces the occurrence and recurrence of dorsalgia. And during non-working hours, playing sports, swimming, yoga strengthens the muscular frame, strength and endurance of the muscles of the body, increases the flexibility of the spinal column, thereby increasing the endurance of production workers.
ACKNOWLEDGEMENTS
- The authors are grateful to the staff of the department of neurorehabilitation of the Center for the Development of Professional Qualifications of Medical Workers under the Ministry of Health of the Republic of Uzbekistan for their help in selecting patients and conducting differentiated treatment. The authors declare that they have no conflicts of interest when writing this article. The publication is funded from its own funds.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML