Irgasheva S. U., Shermatova S. E.
Republican Specialized Scientific-Practical Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan
Correspondence to: Shermatova S. E., Republican Specialized Scientific-Practical Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The article presents the results of surveys of 104 adolescent girls with normogonadotropic oligomenorrhea, the control group consisted of 50 healthy girls with timely menarche and regular menstrual cycle. Depending on causative factor, the patients were divided into 6 groups: PCOS and group of risk for the developing PCOS, group of functional oligomenorrhea, group of patients with hyperprolactinemia, thyroid diseases, non-classical form of Congenital adrenal hyperplasia and idiopathic oligomenorrhea. Distinctive features of the main forms of oligomenorrhea in adolescents are presented, an improved algorithm for diagnosing oligomenorrhea with the marking out the main diagnostic markers is proposed. An immunological study and determination of the follicular reserve in adolescents with oligomenorrhea were carried out. The tactics of management of patients depending on the pathogenesis of the occurrence of oligomenorrhea are described.
Keywords:
Oligomenorrhea, Adolescents, Menstrual disorders, PCOS, Idiopathic oligomenorrhea
Cite this paper: Irgasheva S. U., Shermatova S. E., Features of Diagnosis and Therapeutic Tactics in Various Forms of Oligomenorrhea in Adolescents, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 325-329. doi: 10.5923/j.ajmms.20231303.27.
1. Relevance
Menstrual disorders took a leading place in gynaecological morbidity structure in adolescence. Complaints of infrequent menstruation are common reason for visiting an adolescent gynaecologist. Oligomenorrhea (OM) is a violation of the menstrual cycle, manifested by scanty and rare menstruation. OM diagnosis established based on clinical data - the duration of menstrual cycle is more than 42 days and less than 6 months. Also, according to foreign authors, the criterion for establishing the OM diagnosis is the presence of 4 to 9 monthly menstrual episodes annually [1,2,3,4].Oligomenorrhea in result of hyper- and hypogonadotropic ovarian insufficiency is not particularly difficult to diagnose and has precise recommendations for the management of these patients. Adolescents with oligomenorrhea with normal levels of gonadotropins in a blood serum present the particular interest, because normogonadotropic decrease of ovarian function is the most common cause of menstrual disorders in adolescence. This form of ovarian failure has wide range of ovarian and extragonadal etiological factors: obesity, underweight, polycystic ovary syndrome (PCOS), adrenal hyperandrogenism, functional and organic hyperprolactinemia, primary hypothyroidism, etc. [5,6]. Such a variety of causative factors often provide difficulties in diagnosis and choice of therapeutic tactics for practicing adolescent gynaecologists.
2. The Aim of This Study
The aim of this study was developing diagnostic algorithm for various forms of oligomenorrhea and substantiate the choice of therapeutic tactics.
3. Research Material and Methods
The study involved 104 adolescent girls with oligomenorrhea who referred to the Republican specialized science-practical medical center of obstetrics and gynecology in the period from 2021-2022. The criteria for inclusion to the main group were the following features:1. The patients Age is 15-19 years.2. The time interval between menstruations is from 42 days to 6 months, in case of timely menarche age.3. Gynecological age at least 2 years.4. Patient and her parent’s agreement to participate in the study.The exclusion criteria were:1. Hypo- and hypergonadotropic oligomenorrhea.2. Oligomenorrhea after ovarian surgery.3. The presence of sub and decompensated extragenital pathology.4. Sexually active and pregnant patients.5. Taking combined oral contraceptives and/or other hormonal drugs during last 3 months.The control group consisted of 50 adolescents with timely menarche and regular menstrual cycle. To clarify the oligomenorrhea genesis, the following studies were performed: history taking, general examination with clinical anthropometry, assessment of sexual development, assessment of hirsutism severity according to the Ferryman-Galway score scale, ultrasound of the pelvic organs, according to indications - MRI of the brain and MSCT of the adrenal glands. Hormonal studies were carried out by ELISA and included the determination of serum concentrations of follicle-stimulating (FSH), luteinizing (LH) hormones, prolactin (Prl), estradiol (E2), TSH, testosterone, according to indications - adrenocorticotropic hormone (ACTH), cortisol, 17-OH progesterone. Blood sampling is done in the morning from the cubital vein. [7,8]Comparative assessment of anamnestic, clinical, hormonal parameters was carried out between the following groups: general oligomenorrhea (n=87), this group included girls with established oligomenorrhea causative factors; idiopathic oligomenorrhea-included girls with oligomenorrhea of unclear etiology (n=17) and the control group consisted of patients with normal menstrual cycles.
4. Research Results and Discussion
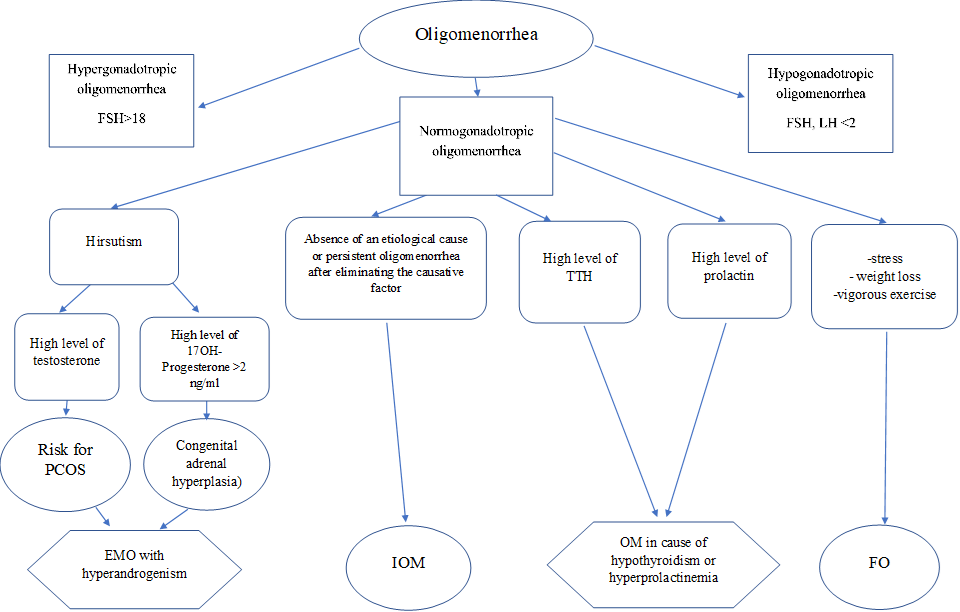
A comprehensive assessment of the obtained data allowed to identify 6 main causative factors of normogonadotropic OM in the cohort of examined patients (Figure 1).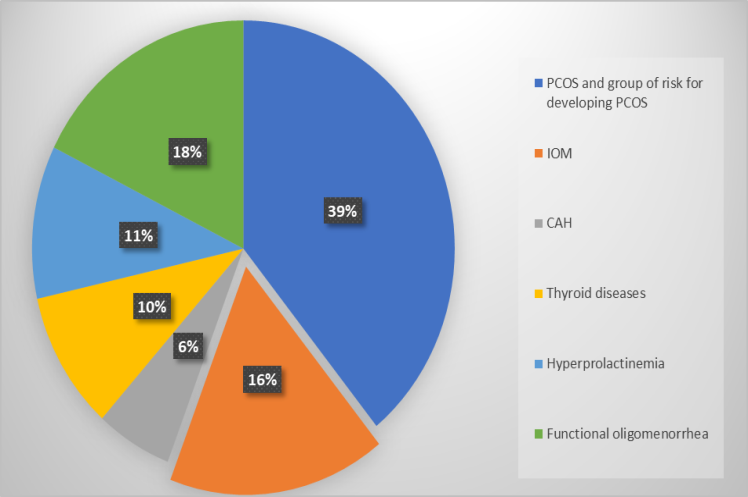 | Figure 1. The structure of normogonadotropic oligomenorrhea in adolescents |
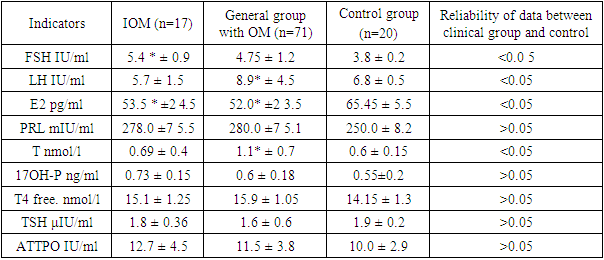
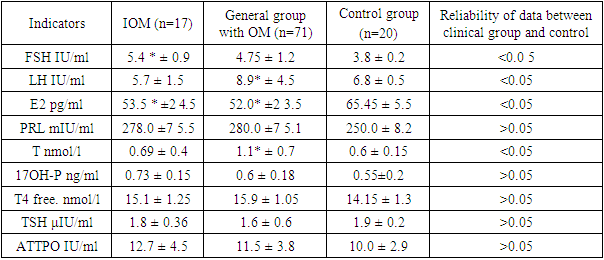
The most common cause of OM was PCOS (polycystic ovary syndrome) (39%). According to the subjects age and last criteria for diagnosing the hyperandrogenic conditions in adolescent girls, this group also included adolescents identified as group of risk for the developing PCOS [9]. The group of functional oligomenorrhea, which accounted for 18% of the examined patients, was the next most frequent group. According to foreign researchers [10], functional oligomenorrhea has the same etiology as functional hypothalamic amenorrhea (FHA), but in this case there is an incomplete suppression of the hypothalamic-pituitary- ovarian axis, manifested by rare menstruation. The main causes of FHA are weight loss, intense exercises and stress.Hyperprolactinemia and thyroid diseases with impaired function, as a causative factor of oligomenorrhea, were detected in 11 and 10% of cases, respectively. Non-classical form of Congenital adrenal hyperplasia (CAH) was detected in 6% of cases.The big interest in the structure of causal oligomenorrhea factors in adolescent girls was the sample of patients with oligomenorrhea that did not have obvious etiological factors caused it, or oligomenorrhea that persisted after the elimination of alleged causes (for example, functional hyperprolactinemia or underweight). This disease form accounted for 16% and we identified it as idiopathic oligomenorrhea (IOM).The results of a comparative assessment of hormonal IOM parameters compared with the general group of patients with oligomenorrhea and their peers with a normal menstrual cycle are shown in Table 1. Analysis of obtained data in the comparison groups revealed a statistically significant decrease in the serum level of estradiol in both clinical groups compared to the control data. This indicates the presence of ovarian insufficiency, which develops regardless of the oligomenorrhea form. At the same time, a statistically significant increase of FSH level compared with the control group was detected only in IOM group. A significant increase in the level of LH, testosterone in the general group of OM compared with the group of healthy adolescents is explained by a significant proportion in the overall structure of oligomenorrhea in adolescents with PCOS.Table 1. Comparative assessment of hormonal parameters in IOM compared with general oligomenorrhea and control
 |
| |
|
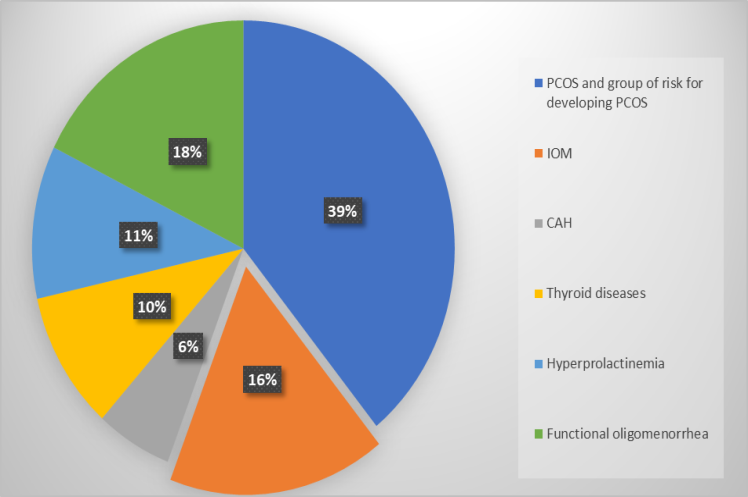
The most significant decrease was in the level of AMH in IOM group with almost identical indicators of serum estradiol concentration in various forms of oligomenorrhea (Figure 2). Thus, the average values of AMH in the group of patients with IOM were almost twice as low as the control data, while in the group with PCOS, this indicator exceeded the control values by 1.6 times. A decrease in the AMH blood concentration of patients with idiopathic oligomenorrhea indicates an increased risk of a decrease in ovarian reserve in this category patients. [11]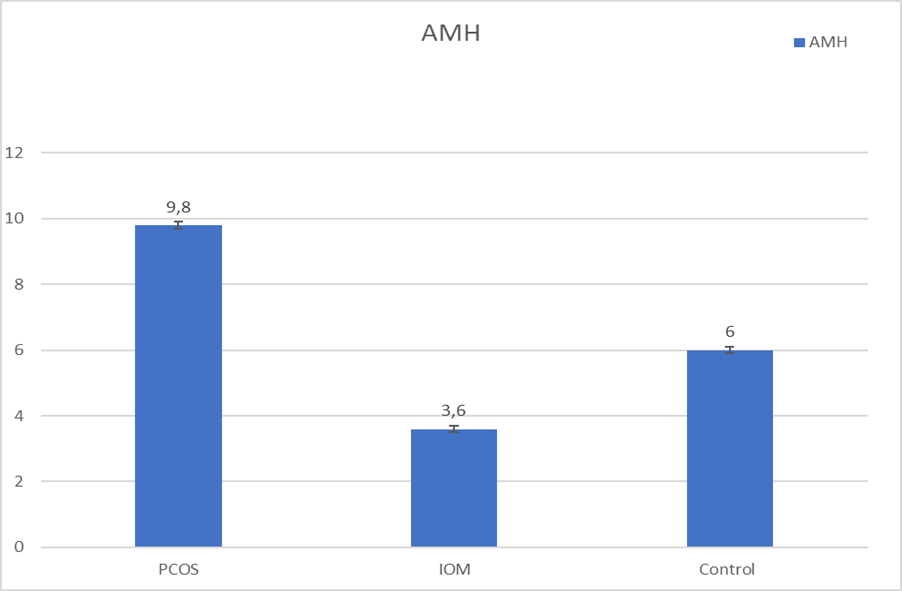 | Figure 2. Serum AMH level in various forms of oligomenorrhea |
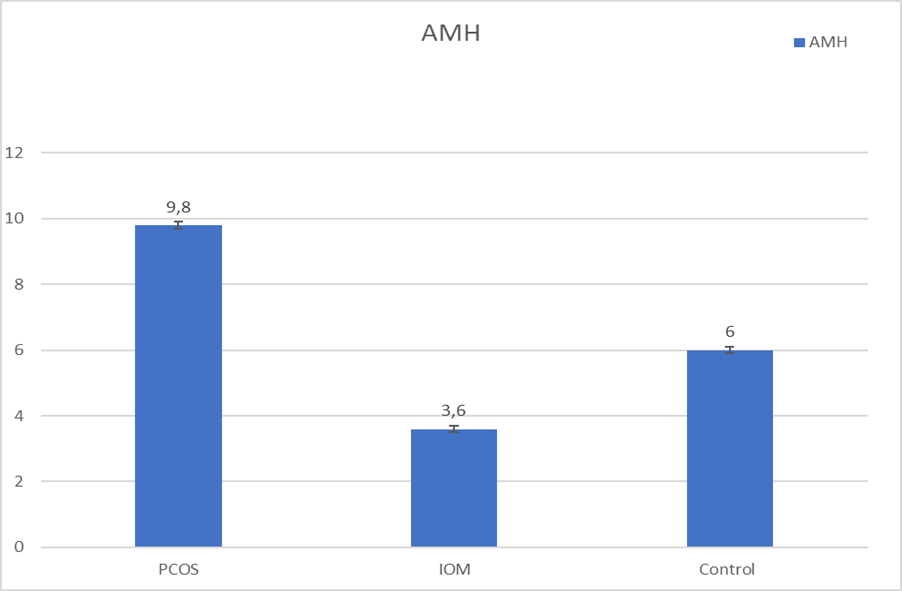
Currently, there is no generally accepted classification of oligomenorrhea that fully reflects the causes of its occurrence. Accordingly, different approaches to classification determine the differences in the diagnostic algorithm and the choice of therapeutic tactics.In our opinion, the classification of the following forms of OM proposed in 2019 by Silvia Baggio et al. [10] deserves attention: endocrine-metabolic oligomenorrhea (EMO) against the background of hyperandrogenism and functional oligomenorrhea (FO). According to the authors, patients with hyperandrogenism, namely, with an increased testosterone or 17-OH progesterone level in the blood serum, should be included in the EMO group. Thus, PCOS risk group and CAH are proposed to be combined into one group - endocrine-metabolic oligomenorrhea group. The main markers for this category are:- clinical or biochemical hyperandrogenism (hirsutism and / or increased serum testosterone),- oligomenorrhea,- polycystic ovaries on ultrasound- 17OH-Progesterone above 2ng / ml.Functional oligomenorrhea is a form of oligomenorrhea resulting from hypothalamic dysfunction. Pathogenetically identified three main markers for the diagnosis of functional oligomenorrhea:- sudden weight loss;- excessive physical activity, accompanied energy deficit;- chronic stress [10].This form of oligomenorrhea is transient, the menstrual cycle normalization is associated with the elimination of these causal factors. [10]Oligomenorrhea on the background of hyperprolactinemia and hypothyroidism, we have combined in a common group, since these conditions can be pathogenetically interrelated, as well as medicine correction methods.We had proposed the idiopathic oligomenorrhea group as the 4th group of OM, in which there is no obvious cause of the menstrual cycle disorder, or when the alleged causal factors were eliminated, the cycle was not normalized.Examination of patients with oligomenorrhea includes a large amount of examinations. The algorithm of laboratory and clinical markers use, that we proposed allows rational use of diagnostic methods, identifying the form of oligomenorrhea and determining the treatment direction (Figure 3).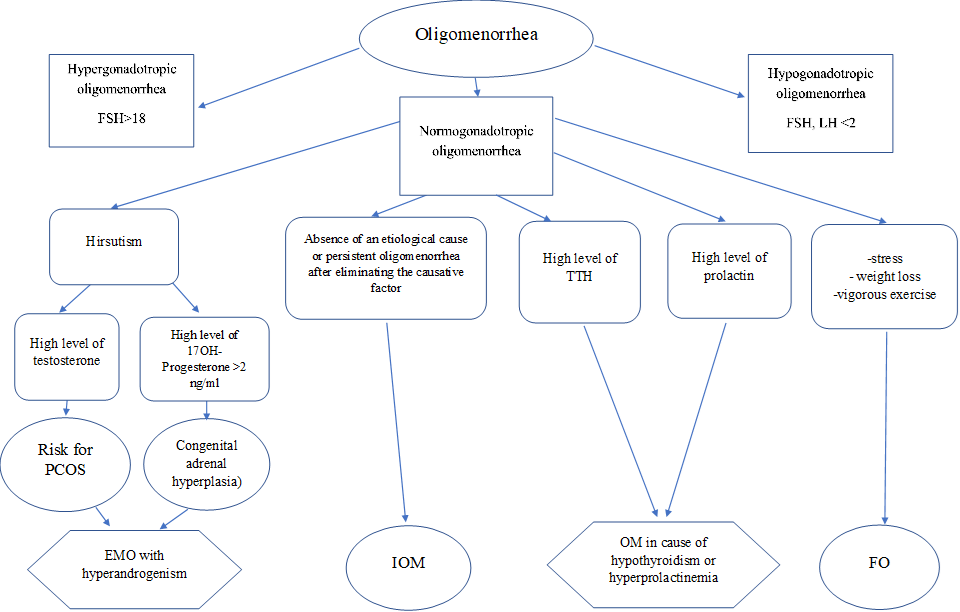 | Figure 3. The Algorithm for the diagnosis of various forms of oligomenorrhea |
Based on the proposed forms of oligomenorrhea and the above algorithm, we consider it rational to adhere to the following directions in therapeutic tactics:Endocrine-metabolic oligomenorrhea on the background of hyperandrogenism.In young overweight patients firstly recommended a lifestyle modification, including physical activity and reduced caloric intake. Drug therapy should be aimed to restoring the menstrual cycle and eliminating androgen-dependent dermatopathy. For this purpose, the use of ultra- and microdosed COCs containing 15 and 20 micrograms of ethinylestradiol is recommended. Metformin is recommended in case of insulin resistance and no effect of diet therapy. In case of suspected CAH in adolescence, the use of glucocorticoids is recommended if the serum level of 17OH-Progesterone exceeds 2.0 ng/ mL [12]. When diagnosis of CAH is established, the diagnosis confirmation and the dose of glucocorticoids selection is carried out with endocrinologist.If the patient is not satisfied with the antiandrogenic response to COC monotherapy, after six months, 50 mg of spironolactone can be added 1-2 times a day. [13]Oligomenorrhea associated with hyperprolactinemia and / or hypothyroidismHypothyroidism. Levothyroxine sodium dose selection for adolescents is carried out in conjunction with an endocrinologist. The drug is recommended to be prescribed for 2-3 months, followed by monitoring of TSH levels. Hyperprolactinemia. Since hyperprolactinemia often occurs due to a decrease in thyroid function, a parallel decrease in prolactin in the blood serum is noted against the background of replenishing the deficiency of thyroid hormones. If there is a persistent increase in prolactin, an additional examination is recommended to clarify the cause of hyperprolactinemia. In case of establishing the diagnosis of functional hyperprolactinemia, dopamine agonists are prescribed - cabergoline, bromergon. If a micro-(macro) adenoma is detected, the patient should be consulted by a neuroendocrinologist (neurosurgeon).Functional oligomenorrhea. Pathogenetic therapy consists in eliminating the causative factor: this cohort of patients is recommended to normalize the regime of work and rest, replenish body weight deficit, and eliminate the influence of stressful situations. If necessary, patients are consulted by specialists of a related profile - a neuropsychiatrist, therapist, psychotherapist.Idiopathic oligomenorrhea. Hormone therapy courses, such as microdosed COCs, are recommended as therapy and for the normalization of menstrual cycle. Since these patients are at risk for the development of premature ovarian failure, active monitoring and earlier implementation of reproductive function should be recommended.
5. Conclusions
Thus, oligomenorrhea in adolescence is a multifactorial pathology. The selection of the proposed groups, in our opinion, allows the rational use of diagnostic methods and the correct choice of pathogenetic therapy. Idiopathic (unspecified) oligomenorrhea may be a predictor of POF and requires more detailed study.
References
| [1] | Riaz Y, Parekh U. Oligomenorrhea. [Updated 2022 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560575/. |
| [2] | Glueck, CJ. Adolescent oligomenorrhea (age 14-19) tracks into the third decade of life (age 20-28) and predicts increased cardiovascular risk factors and metabolic syndrome / CJ Glueck [et al.] // Metabolism. – 2015. –Vol. 64(4). -P. 539–553. |
| [3] | Jacobs, A. M. Oligomenorrhea in the Adolescent // The Female Patient. - 2012. - Vol. 37, No. 1. - P. 19-24. |
| [4] | P. Pinola [et al.] Menstrual disorders in adolescence: a marker for hyperandrogenaemia and increased metabolic risks in later life? // Human Reproduction, Vol.27, No.11 pp. 3279–3286, 2012. |
| [5] | Rigon F, De Sanctis V, Bernasconi S, Bianchin L, Bona G, Bozzola M, Buzi F, Radetti G, Tatò L, Tonini G, De Sanctis C, Perissinotto E. Menstrual pattern and menstrual disorders among adolescents: an update of the Italian data. Ital J Pediatr. 2012 Aug 14; 38: 38. |
| [6] | Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ; International PCOS Network. Recommendations from the international evidencebased guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018 Aug; 110(3): 364-379. |
| [7] | Bauman, D. Diagnostic methods in pediatric and adolescent gynecology // Endocrine development. - 2012. - Vol. 22. – P. 40-55. |
| [8] | Braverman, PK, Breech L. American Academy of Pediatrics. Clinical report--gynecologic examination for adolescents in the pediatric office setting. // Journal Pediatrics. - 2010. - Vol. 126, No. 3. - P. 583-590. |
| [9] | Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, Noroozzadeh M, Farahmand M, et al. The risk of metabolic syndrome in polycystic ovary syndrome: A systematic review and meta-analysis. Clin Endocrinol (Oxf) 2018; 88: 169–84. |
| [10] | Silvia Baggio*, Rossana Di Paola, Stefano Zaffagnini, Stefania Fino, Ricciarda Raffaelli and Massimo Franchi Functional and endocrine-metabolic oligomenorrhea: proposal of a new diagnostic assessment tool for differential diagnosis in adolescence // J Pediatr Endocrinol Metab 2019; aop. |
| [11] | Casper P. Hagen*, Lise Aksglaede, Kaspar Sorensen, Annette Mouritsen, Anna-Maria Andersson, Jorgen Holm Petersen, Katharina M. Main, and Anders Juul. Individual serum levels of anti-Mullerian hormone in healthy girls persist through childhood and adolescence: a longitudinal cohort study // Human Reproduction, Vol.27, No.3 pp. 861–866, 2012. |
| [12] | Honor, John. (2014). 17-Hydroxyprogesterone in children, adolescents and adults. Annals of clinical biochemistry. 51. 10.1177/0004563214529748. |
| [13] | Kim GK, Del Rosso JQ. Oral Spironolactone in Post-teenage Female Patients with Acne Vulgaris: Practical Considerations for the Clinician Based on Current Data and Clinical Experience. J Clin Aesthet Dermatol. 2012 Mar; 5(3): 37-50. PMID: 22468178; PMCID: PMC3315877. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML