Munisa Sabirova1, Nurkhon Mukhamedova2, Gulchekhra Umarova1
1Head Teacher, 1st Republic Abu Ali Ibn Sina Technical School of Public Health, Uzbekistan
2Associate Professor, Department of Medical and Biological-Chemistry, Tashkent Medical Academy, Uzbekistan
Correspondence to: Munisa Sabirova, Head Teacher, 1st Republic Abu Ali Ibn Sina Technical School of Public Health, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The information about determining the significance of laboratory biomarkers of renal damage in metabolic syndrome in postmenopausal women is given in this article.The study included 48 postmenopausal women with metabolic syndrome (MS), n=48 (44%), and a control group of healthy volunteers - 14 women of comparable age. The age of the patients ranged from 40 to 65 years (the average age of the examined women was 54.4 ± 9.1 years). All patients were treated in multidisciplinary clinics of Tashkent medical academy (TMA). The studies were carried out using automatic analyzers of the company. Mindray, diagnostics set HUMAN analysis.
Keywords:
Metabolic syndrome, Postmenopausal, Hyperinsulinemia, Cholesterol
Cite this paper: Munisa Sabirova, Nurkhon Mukhamedova, Gulchekhra Umarova, Indicators of Carbohydrate Metabolism in Women with Metabolic Syndrome in the Postmenopausal Period, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 304-307. doi: 10.5923/j.ajmms.20231303.23.
1. Introduction
Today, the search for new markers of kidney tissue damage, as well as the identification and refinement of the functional characteristics of known biomarkers with the aim of more objective and early kidney damage in women with metabolic syndrome (MS) in the postmenopausal period, is relevant in modern conditions [1,2,3].During the postmenopausal period, the ovaries secrete about 50% testosterone and 30% androstenedione into the peripheral circulation. Discoordination of the interaction of the central and peripheral parts of the hypothalamic-pituitary-adrenal system develops; androgenic function decreases with increasing or stable adrenocorticotropic function of the pituitary gland; the so-called postmenopausal pituitary gland is formed [3,5].Hyperinsulinemia, insulin resistance, and central obesity characterize postmenopausal insulin metabolism [4].The aim of the study is to determine the significance of laboratory biomarkers of renal damage in metabolic syndrome in postmenopausal women.
2. Material and Methods
The study included 48 postmenopausal women with MS, n=48 (44%), and a control group of healthy volunteers - 14 women of comparable age. The age of the patients ranged from 40 to 65 years (the average age of the examined women was 54.4 ± 9.1 years). All patients were treated in multidisciplinary TMA clinics. The studies were carried out using automatic analyzers of the company. "Mindray", diagnostics set "HUMAN" analysis.According to R. Kraues (2015), postmenopausal insulin resistance can often be the center of a "confusing scientific" risk factor for CVD. The frequency of manifestations of MS in the postmenopausal period increases to 50%.
3. Results and Discussion
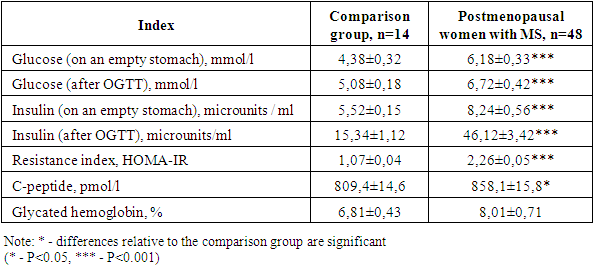
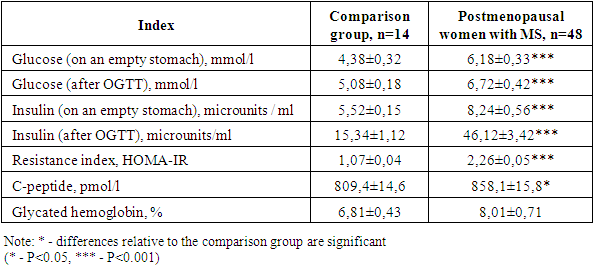
Based on the above, it is of interest to study the dynamics of carbohydrate metabolism in women with MS in the postmenopausal period. The study showed (Table 1) that fasting glucose levels in postmenopausal women with MS are 41% higher. During the stress test, the concentration of insulin in the blood of women with MS in the postmenopausal period exceeded 1.5 times (P<0.05). The content of insulin in the blood in the comparison group is 3 times higher (P<0.05). The insulin resistance index exceeded the initial values by 2 times. Therefore, postmenopausal women with MS have hyperinsulinemia.Table 1. Indicators of carbohydrate metabolism in women with MS in the postmenopausal period, М±m
 |
| |
|
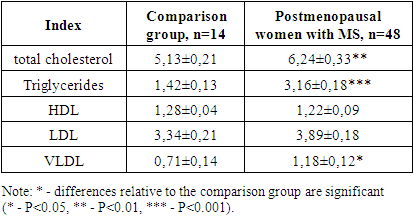
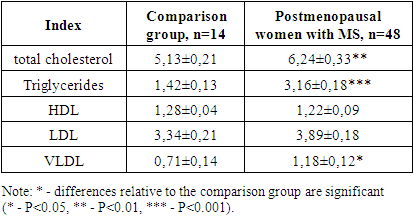
Hyperinsulinemia is compensatory and at the same time pathological, as it contributes to the emergence and development of metabolic hemodynamic organ disorders. Of the external factors that adversely affect tissue sensitivity to insulin, the most important is excessive consumption of animal fat containing saturated fatty acids, which lead to structural changes in cell membrane phospholipids and disruption of the expression of genes that control the conduction of the insulin signal into the cell.Hyperinsulinemia in women with MS in the postmenopausal period is accompanied by an increase in the content of proinsulin C-peptide, which is higher in the blood of women with MS in the postmenopausal period (P<0.05).Insulin, together with potassium ions, promotes the penetration of glucose from the blood into the cell. This leads to the binding of glycated hemoglobin. This condition is a marker of a hyperglycemic state.The level of glycated hemoglobin in erythrocytes in postmenopausal women with MS is higher than 2.8% (P>0.05).The decrease in postmenopausal estrogen levels gradually leads to the accumulation of lipids, especially free fatty acids. They activate the secretion of insulin by the pancreas, reduce its hepatic clearance, promote the progression of hyperinsulinemia, reduce the binding of insulin to receptors, and inhibit the uptake and utilization of glucose [6,7,8].Indicators of lipid metabolism in postmenopausal women with metabolic syndrome Obesity in postmenopausal women is one of the most common chronic diseases. According to WHO, 300 million people in the world are obese. The number of overweight people increases by 10% every 10 years. This is associated with an increase in the incidence of coronary heart disease, arterial hypertension and type 2 diabetes mellitus. Approximately half of women over 55 years of age have a clinic of atherosclerosis and coronary artery disease, 35% have signs of type 2 diabetes mellitus. According to the literature, patients with III-IV degree obesity, on average, live 15 years less than people with normal body weight. Therefore, the diagnosis and prevention of obesity among postmenopausal women is an important task of modern health care, and laboratory monitoring of lipid metabolism is of particular relevance [9,10,11].It was found that in women with MS in the postmenopausal period, the indicators of total cholesterol (TC), triglycerides, HDL, LDL, VLDL exceed the reference values (Table 2).Table 2. Lipidogram parameters (mmol/l) in women with MS in the postmenopausal period
 |
| |
|
Thus, the level of total cholesterol in the blood of women with MS in the postmenopausal period exceeded that in the comparison group by 22% and averaged 6.24±0.33 mmol/l (P<0.05). The content of triglycerides was 2.2 times higher than the initial values (P<0.05). The amount of HDL remained within the same range in the comparison group. In our opinion, this is due to the activity of hepatic triglyceride lipase, the level of which rises sharply at a low level of estrogen, increasing the clearance of HDL.The study revealed a slight increase in the concentration of LDL in the blood of women with MS in the postmenopausal period. On average, this figure was 3.89±0.18 mmol/l, which was higher than in the comparison group by 16.5%. The increase in LDL levels is apparently due to the blocking of its receptors in the liver by endotoxication in women with MS in the postmenopausal period.The level of VLDL in the blood of women with MS in the postmenopausal period (Table 2) significantly increased to an average of 1.18±0.12 mmol/l, which was 66.2% higher than the initial value. CVDs contain a large amount of triglycerides and cholesterol esters in relation to the number of apoproteins. An increase in the level of VLDL in women with MS in the postmenopausal period is due to a high level of triglycerides in the blood plasma and their enhanced formation in the liver under the action of lipoprotein lipase.Thus, changes in the lipid profile in the postmenopausal period in women with MS are associated not only with changes in hormonal status, but also with functional changes in the liver.When studying the lipid profile, the level of total cholesterol, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol is determined. Lipid metabolism disorders largely determine the likelihood of developing type 2 diabetes mellitus, cardiovascular diseases, and the prognosis of a woman's life in various periods of menopause.Women with MS develop secondary hyperlipoproteinemia. It is characterized by an increase in the level of VLDL, TG in the blood and a decrease in the content of esterified cholesterol in the core of lipoproteins of all classes; a change in the spectrum of HDL, an increase in the concentration of LP.There is a pronounced hypertriglyceridemia associated with an increase in the synthesis of triglycerides in the liver.The subclass of small dense particles of LDL is the most dangerous in terms of the development of CVD. It is they, characterized by high atherogenicity, that predominate in patients with MS.In hyperglycemia, glycated LDL is not recognized by LDL receptors in the liver. Their concentration in blood plasma increases, which leads to an atherogenic form of dyslipidemia. In patients with metabolic syndrome, the concentration of LDL and LDL in blood plasma is increased.Before menopause, women have a significantly lower risk of developing atherosclerosis. This is due to the protective properties of estrogens, which maintain the concentration of lipids within the normal range. However, with estrogen deficiency, the factors for the development of metabolic disorders increase. The protective effect of estrogens on lipid metabolism is as follows: the production of large, rich TG, VLDL particles, the level of total TG in the blood increases; the content of LDL decreases due to an increase in the number of hepatic receptors for LDL. All this leads to increased catabolism. Estrogens can inhibit the activity of hepatic triglyceride lipase, increase HDL levels due to a delay in their clearance. Expression of LDL receptors is negatively regulated by intracellular cholesterol mediated by sterol-binding regulatory protein-2.In 98.3% of women with MS in the postmenopausal period, dyslipoproteinemia is detected, only in 1.7% of patients the lipidogram values correspond to the norm.The content of HDL cholesterol in postmenopausal women is lower than in the comparison group. LDL cholesterol in postmenopausal women exceeded the values of the comparison group by 11.0% and averaged 2.81±0.12 mmol/l. The level of VLDL cholesterol averaged 0.78±0.05 mmol/l, which is 36.8% higher than in the comparison group.Thus, no significant changes were found in the blood lipid transport system in women with MS in the postmenopausal period. After recalculation according to the method of A. N. Klimov, the cholesterol coefficient was 4.52 units, and in the comparison group - 2.89 units. (Table 3).Table 3. Indicators of the lipid transport system (mmol/l) in women with MS in the postmenopausal period
 |
| |
|
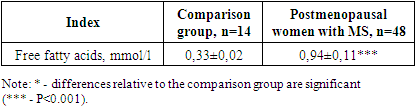
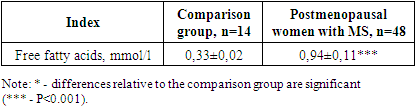
To assess the risk of developing coronary artery disease, you can use the results of determining the content of total cholesterol and HDL cholesterol in blood serum. A low level of α-Cholesterol is associated with a high risk of atherosclerotic lesions of the coronary arteries.The concentration of total cholesterol is of relative importance for assessing the patient's condition. The same level of lipids, depending on other factors, can cause atherosclerotic lesions. Patients with a low concentration of HDL-C are characterized by an increased risk of coronary artery disease even with a low content of total cholesterol in the blood serum. Therefore, determining the concentration of HDL cholesterol is mandatory for assessing the lipoprotein spectrum of blood. Women with low HDL-C and hypertriglyceridemia are at increased risk of MS.Currently, non-esterified fatty acids play an important role in the development of the metabolic syndrome. Insulin resistance enhances lipolysis and results in the release of large amounts of free fatty acids. This condition is combined with hyperglycemia and provides an additional amount of substrate for the synthesis of triglyceride. The relationship between glucose-insulin homeostasis and free fatty acids predetermines the need to study their role in women with MS in the postmenopausal period.In patients with MS in the postmenopausal period, the level of free fatty acids is 2.8 times higher (Table 4) than in healthy women. This is due to hyperinsulinemia and insulin resistance, changes in metabolism in mitochondria, i.e. in conditions of hormonal changes in the body. Free fatty acids are one of the reasons for the accumulation of reactive oxygen species and cell death.Table 4. The content of free fatty acids in the blood of postmenopausal women with MS
 |
| |
|
The degree of risk of coronary heart disease, depending on the ratio of total cholesterol / HDL cholesterol in women with MS in the comparison group - 3.88 in the postmenopausal period, on average, is 5.52; (medium degree).The risk of LDL-C/HDL-C in postmenopausal women with MS was 2.49 versus 1.92 arb. units, which also indicates a high risk of developing coronary artery disease. An HDL-C concentration below 0.9 mmol/L (35 mg/dL) is a risk factor.Thus, in women with MS in the postmenopausal period, against the background of unexpressed hormonal changes, there are unreliable changes in the lipid transport system and atherogenicity in the blood. The combination of hyperinsulinemia with hyperglycemia is accompanied by an increase in lipolysis and an increase in the level of free fatty acids in the blood, which uncouple the electron transport chain in mitochondria and lead to the accumulation of oxygen free radicals in the cell, which adversely affect the cell, accelerating its death.
4. Conclusions
a) We found that 88% of the examined women had hyper- and dyslipidemia;b) Manifested by an increase in the level of fatty acids in the blood serum by 2.4 and 3.5 times;c) Total cholesterol and cholesterol in very low lipoproteins;d) A decrease in cholesterol in high lipoproteins;e) An increase in the atherogenic index.
References
| [1] | Avshalumov A.S., Markovsky V.B., Poleshchuk O.I. Changes in the rheological properties of blood in a patient with metabolic syndrome // Russian Medical Journal. - 2015. - T. 16, No. 4. - S. 200-205. |
| [2] | A. S. Akhmetov and A. A. Belykh, Acoust. Effectiveness of correction of disorders of carbohydrate and lipid metabolism in individuals with high risk factors // Russian Medical Journal. - 2014. - No. 2. - S. 2156-2160. |
| [3] | Akhmetov A.S., Kondratieva L.V. Metformin is the basis of therapy for patients with metabolic syndrome. Russian Medical Journal. - 2006. - T. 14, No. 26. - S. 1905-1911. |
| [4] | V. V. Dolgov, A. S. Akhmetov, K. A. Shchetnikovich, A. P. Roitman, and T. Yu. Laboratory diagnostics of carbohydrate metabolism disorders, diabetes mellitus. - Tver: Triada, 2020. - 112 p. |
| [5] | Dankina, V.V. Violation of lipid metabolism against the background of insulin resistance in perimenopausal women / V.V. Dankina, I.A. Dankina, A.A. Chistyakov, K.V. Dankin // Obstetrics and Gynecology - 2020 - No. 4 (Appendix) - P.68-69. |
| [6] | R. Kraues (2013), Klychnikova E.V. Oxidative stress, lipid metabolism and their relationship in patients with severe hypertension in combination with carotid stenosis/ // Clinical laboratory diagnostics - 2013 - No. 5 - P. 20-22. |
| [7] | Ay C., Tangier T., Vormittag R., Simony R., Dorado W., Vukovich T., Painter I. Venous thromboembolism – a manifestation of the metabolic syndrome // Hematological. – 2018. – Vol. 92, №3. – Р. 374-378. |
| [8] | Barkley L. Meds cape Medical News. New definition of the metabolic syndrome: a newsmaker interview with Sir George Alberta, MA. Available at. http://www.medscape.com/viewarticle/504382 Accessed Juli 8, 2005. |
| [9] | Barrette-Connor E., Wenger N.K., Grady D. et al. Coronary heart disease in women, randomized clinical trials, HERS and RUTH // Maturates. – 2008. – Vol. 31. – P. 1-7. |
| [10] | Basic S.S., Manson J.E. Menopausal hormone therapy and cardiovascular disease risk: utility of biomarkers and clinical factors for risk stratification // Clink. Chem. – 2014. – Vol. 60, №1. – Р. 68-77. |
| [11] | R. Kraues., Plasma metabolic profiles in women are menopause dependent // PLoS One.- 2015 - T.10(11) - P. 141743. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML