Mavlyanova Zilola Farkhadovna1, Sharipov Rustam Khaitovich2, Shamsiddinova Madinabonu Shuhrat Kizi3
1Head of the Department of Medical Rehabilitation, Sports Medicine and Traditional Medicine, Samarkand State Medical University, Uzbekistan
2Head of Department of Pediatrics and General Practice of the Faculty of Postgraduate Education, Samarkand State Medical University, Uzbekistan
34th Year Student of the Medical and Pedagogical Faculty of Samarkand State Medical University, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Purpose: to assess the individual section of the functioning of children with cerebral palsy with the allocation of domains of social adaptation. Material and methods of research: 214 children diagnosed with cerebral palsy aged 2 to 16 years were examined. Based on an in-depth clinical and neurological examination, patients were divided into 6 subgroups in accordance with the ICD-10 depending on the form of the disease; The proportion of spastic forms among the total number of hospitalized children with cerebral palsy was 57%. In order to systematize and further dynamic monitoring of patients with cerebral palsy, the International Classification of Functioning, Disability and Health, Children and Youth Version, ICF-CY was used. Results of the study: Determining the degree of social and domestic adaptation of children with cerebral palsy by studying the category of environmental factors showed that 166 (77.6%) of the surveyed had an unadapted life with a predominance of profound issues. An analysis of the results by the definition of activity and participation stated that 78 (36.4%) children had a moderate level, and 118 (55.1%) children had a severe level of impairment. According to the components of the “body functions” section, a severe level of problems was most often recorded among children with G 80.0 (55.8%), in every third child with G 80.3 (35.5%) and with G 80.8 (34.3%). Intellectual deficiency in children with cerebral palsy, of a disharmonious and uneven nature, was manifested not only by low cognitive activity, but also by a lack of interest in activities, slowness and a low level of concentration, being recorded most often in the forms G 80.0 (88.4%), G 80.4 (84.6%), G 80.2 (67.5%), G 80.8 (57.1%).
Keywords:
Cerebral palsy, Domains, Social adaptation
Cite this paper: Mavlyanova Zilola Farkhadovna, Sharipov Rustam Khaitovich, Shamsiddinova Madinabonu Shuhrat Kizi, Assessment of Functioning, Limitations of Activity and Health of Children with Cerebral Palsy, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 294-299. doi: 10.5923/j.ajmms.20231303.21.
1. Introduction
Worldwide, cerebral palsy (ICP) is not only the most common [3,9,16] and complex disease among all neuromotor disorders in children [4,7,11], but also the most common cause of physical disability in childhood [12,13,14,15,17,18,20], which is diagnosed in one in 500 children in developed countries and leads to more than 1 million chronic patients at the age of 21 years [21].The range of levels of development and comorbidities in children with cerebral palsy varies, affecting the quality of life of children and their families, as well as functional outcomes [1,2,11].The development of children and adolescents with cerebral palsy has been the subject of numerous studies over the past 50 years [5,10]. Particular attention is paid to the application of the International Classification of Functioning, Disabilities and Health of Children and Adolescents, including those with cerebral palsy, which allows a deep and reliable study of functionality in terms of clinical symptoms, environment and personality, as well as dynamic monitoring of changes, achievement of goals and tasks of rehabilitation at each of its stages [5,6].Since in the group of children with severe neurological disorders, social adaptation is an equally important problem that affects the state of health, this encourages research to assess the functioning and disability in this category of children [19].
2. Purpose of the Study
Evaluate the individual abilities of children with cerebral palsy with the allocation of domains of social adaptation.
3. Material and Methods of Study
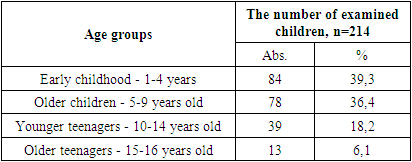
214 children with cerebral palsy aged 2 to 16 years were examined. Based on an in-depth clinical and neurological examination, patients, in accordance with ICD-10, are divided into 6 subgroups depending on the form of the disease:1 subgroup - tetraplegia - G 80.0 - 20.1% (n=43) 2 subgroup - spastic diplegia - G 80.1 - 18.2% (n=39) 3 subgroup - children's hemiplegia - G 80.2 - 18.7% (n=40) 4 subgroup - dyskinetic cerebral palsy - G 80.3 - 14.5% (n=31) 5 subgroup - ataxic cerebral palsy - G 80.4 - 12.1% (n=26) subgroup 6 - mixed form of cerebral palsy - G 80.8 - 16.4% (n=35).From figure 1 it follows that among the examined children, patients with quadriplegia G 80.0 - 20.1% prevailed. Children with ataxic G 80.4 - 12.1% and dyskinetic forms G 80.3 - 14.5% were less common. At the same time, the proportion of spastic forms among the total number of hospitalized children with cerebral palsy was 57%.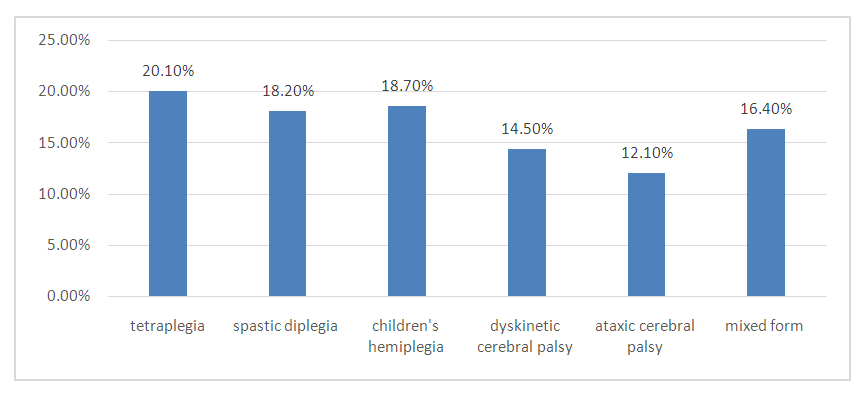 | Figure 1. Distribution of children with cerebral palsy into subgroups |
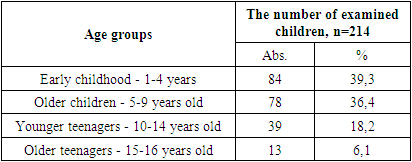
The study group was divided by age and gender. Age gradation of children was carried out according to WHO recommendations (2021) and is presented in Table 1. The average age of children included in the study was 6.7 ± 0.27 years.Table 1. Distribution of examined children with cerebral palsy depending on the age by WHO standards (2021)
 |
| |
|
According to the distribution by gender, an almost 2-fold predominance of boys (62.6%) over girls (37.4%) was established, their ratio was 1.7:1; which coincides with the sciencific data, according to which the frequency of occurrence among boys is 62.9%. This pattern is explained by the greater vulnerability of the premature male child to white matter damage and intraventricular hemorrhage, as well as the neuroprotective effect of the female sex hormone estrogen. In order to systematize and further dynamic monitoring of patients with cerebral palsy, the International Classification of Functioning, Disability and Health, Children and Youth Version, ICF-CY was used, consisting of 25 categories divided into sections - "Functioning" and "Contextual factors". The “Functioning” section includes “body functions”, “body structure”, “activity and participation”, and the “Contextual factors” section includes “environmental factors” and “personal factors”.The component of each section is subdivided into domains containing various categories, which makes it possible to describe and measure the degree of health impairment in children, taking into account a unified individual profile of the child's functioning, including personal and environmental factors [6,8].
4. Results of the Research
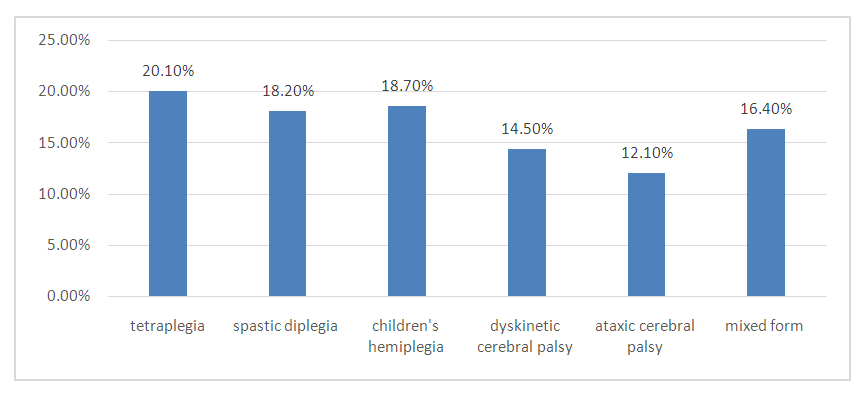
In order to unify the individual profile of a child with cerebral palsy, an analysis of domains according to the ICF was carried out, characterizing not only the assessment of pain, dysfunction of the motor and coordinating abilities, but also taking into account environmental and personal factors. In accordance with the ICF, the following factors were taken into account during rehabilitation: structural and functional disorders, including the diagnosis of existing clinical syndromes (motor, hyperkinetic, muscle hypotension, speech, behavioral ones); activity of the patient (taking into account the age of the child and the severity of motor disorders identified in him, the ability to perform one or another activity); the social status of the family and the motivation of parents, environmental factors, both facilitating and limiting the rehabilitation process; social activity, personal motivation and personal characteristics of a patient with cerebral palsy. Analysis of the results of a study to determine the degree of social adaptation of children with cerebral palsy by studying the category of "environmental factors" using e115 domains - products and technologies for personal everyday use; e120 - products and technologies for personal movement and transportation in and out of premises; e125 - means and technologies of communication, as well as e150 - design, the nature of the design, construction and arrangement of buildings for public use showed that 166 (77.6%) of the examined children revealed an unadapted life with a predominance of absolute disorders (Fig. 2).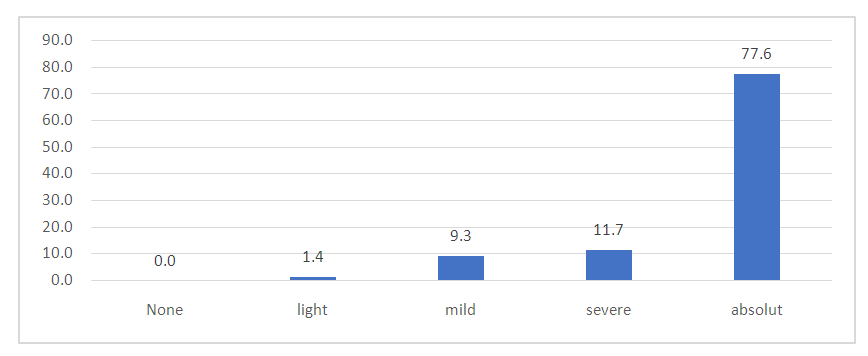 | Figure 2. Distribution of the magnitude and degree of domain damage e 115-150 of children with cerebral palsy |
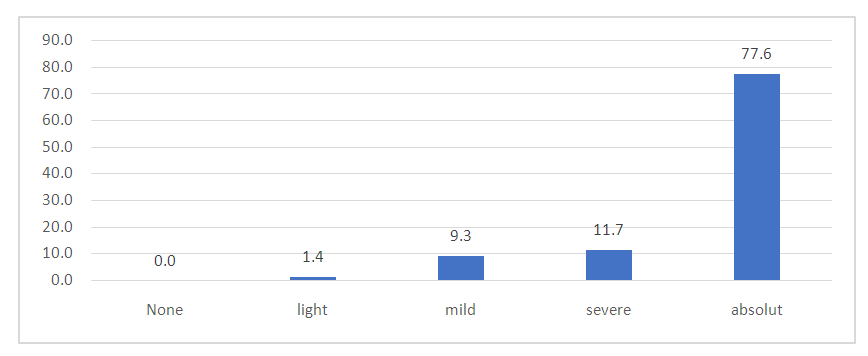
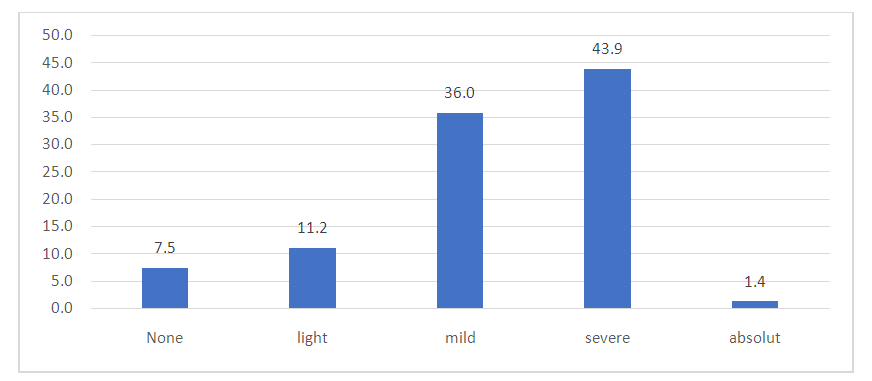
Considering the ethno-cultural characteristics of the population, all 166 patients lived in the private sector, the sick child was placed in one room, deprived of the opportunity to move independently around the house, and living conditions were not available to him. The mode of life was partially adapted for children living in apartments - 48 (22.4%), the thresholds between the rooms were removed in their house, there are handrails, more often in the child's room. All the examined have not adapted bathrooms and toilets; the child, without outside help, could not satisfy the basic physiological needs, carry out personal hygiene, and perform daily household self-service skills.Analysis of the results of the study to determine the degree of "activity and participation" by means of ICF sets using d415 domains - maintaining body position; d440 - the use of precise brush movements; d550 - food intake stated the following: 78 (36.4%) children had a moderate level, and 118 (55.1%) children had a severe level of disorders (Fig. 3).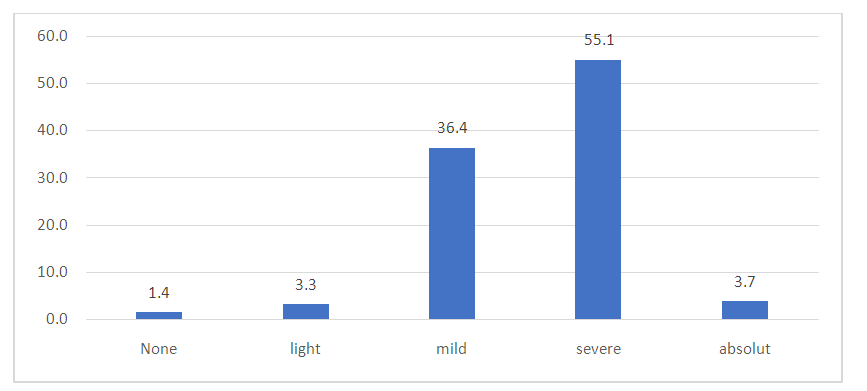 | Figure 3. Distribution of the degree of violations of social adaptation by domains d 415-550 according to the ICF-Disability and Health |
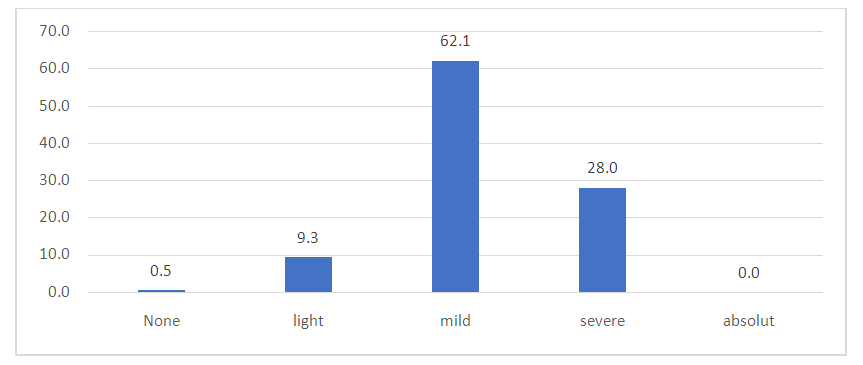
Evaluation of the results of the “body function” according to the ICF for children with cerebral palsy made it possible to establish that 133 (62.1%) children had a moderate level of impairment, and 60 (28.0%) children had a severe level (Fig. 4).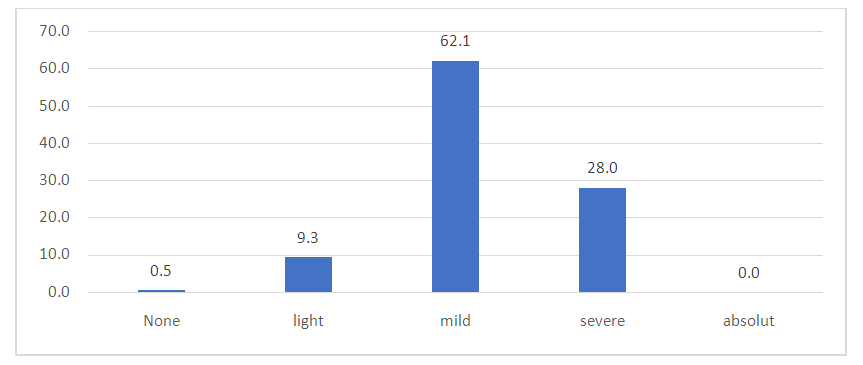 | Figure 4. Distribution of ICF Impairment Degrees by scoring b domains 117-760 |
An analysis of the ICF was also carried out for the s110 domain - the structure of the brain, which showed that 94 (43.9%) children had a severe level, 77 children (36.0%) had a moderate level of impairment (Fig. 5).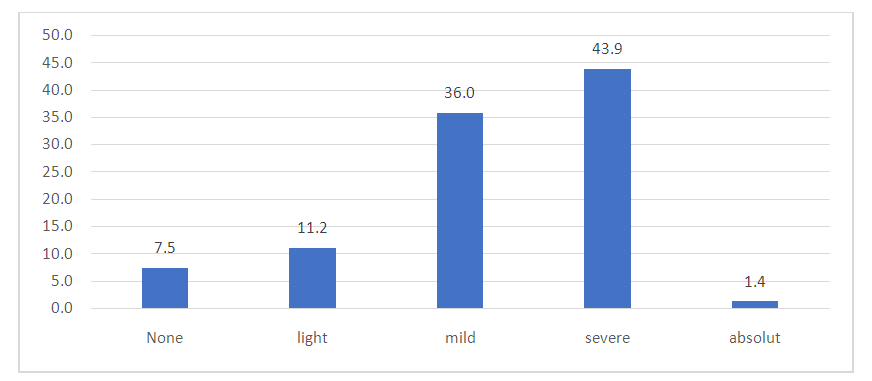 | Figure 5. Distribution of the severity of disorders in children with cerebral palsy by the s110 domain - brain structure |
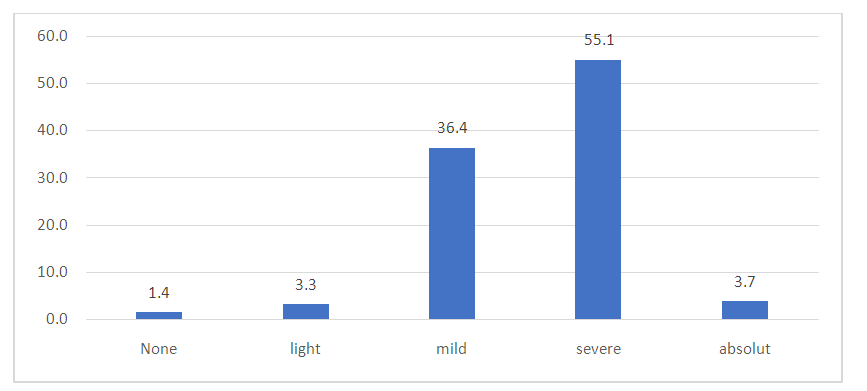
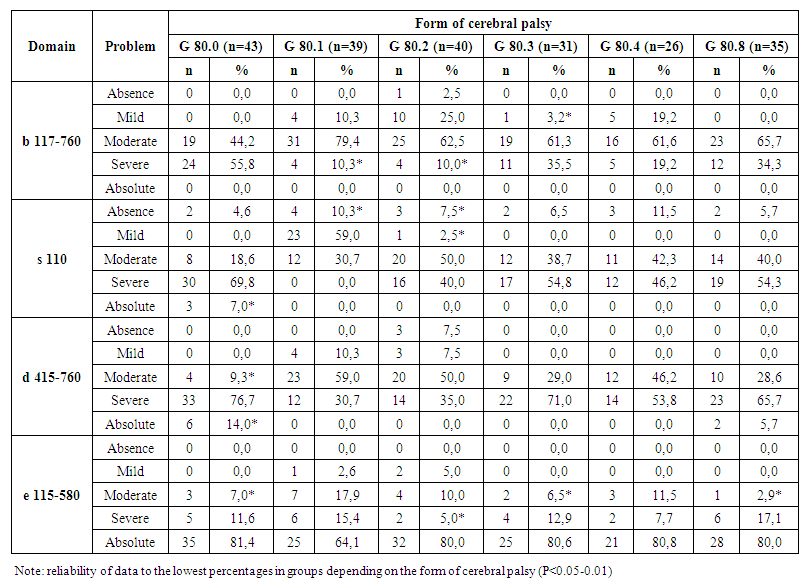
Evaluation of functioning, disability and health of children depending on the topographic form of cerebral palsy is presented in Table 2.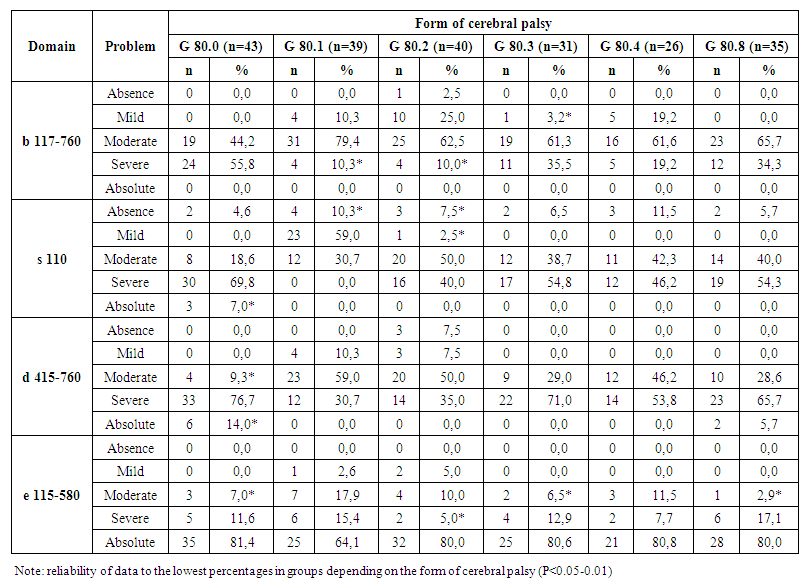 | Table 2. Assessment of the functioning, disability and health of children using sets of ICF domains depending on the form of cerebral palsy |
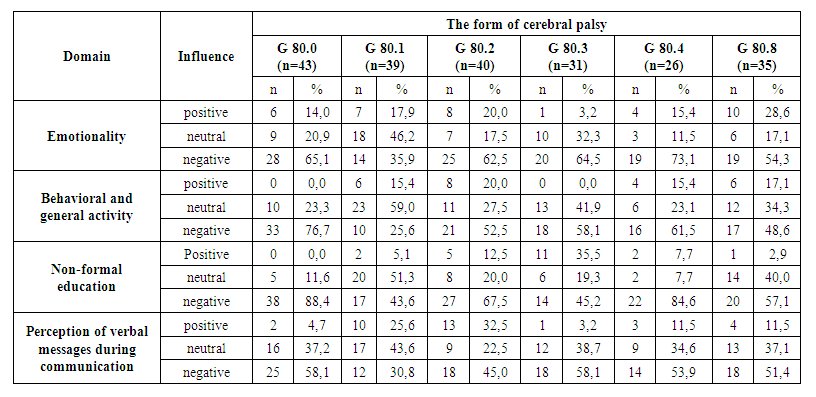
As can be seen from the data presented, a correlation has been established between the forms of cerebral palsy and the severity of problems in the studied domains. So, according to the components of the "body functions" section, we found that a severe level of problems was most often recorded among children with G 80.0 (55.8%), and also occurred in almost every third child with G 80.3 (35.5%) and with G 80.8 (34.3%), while the smallest amount at G 80.1 and G80.2 (10.3% and 10.0%, respectively). It should be noted that in 2.5% of children with G80.2 no problems were identified, while in other forms the level of severity of problems was more manifested. Mild problems in domains b 117-760 occurred in 25.0% of children with G 80.2, in 19.2% with G 80.4, in 10.3% of children with G 80.1 and in 3.2% of those examined with the G 80.3 form. With forms G 80.0 and G 80.8, this degree of problems was not noted. In most cases, moderate and severe problems were encountered in all topographic forms of cerebral palsy. Absolute problems in the study of domains b 117-760 were not registered.The category "activity and participation" is reflected in the domains d 415-760. While interpreting the data, it was found that 7.5% of children with G 80.2 had no problems, in 7.5% of cases with this form of cerebral palsy, mild problems were identified, as well as in 10.3% of patients with the form G 80.1. The occurrence of moderate problems was most often recorded at G 80.1 (59.0%), and the smallest percentage was observed in children with G 80.0, amounting to 9.3%. At G80.2, moderate severity of problems was recorded in every 2 children with cerebral palsy, and at G 80.4 in 46.2% of children. Severe problems were recorded in 76.7% of cases with G 80.0, in 71.0% - with G 80.3, in 65.7% of cases - with G 80.8. Whereas 14.0% of children with quadriplegia (G 80.0) had absolute problems. The highest frequency of registering the absence of problems or a mild degree of severity of problems for the domain "s110 - brain structure" was detected at G 80.1 (10.3% and 59.0%, respectively), while at G 80.0 moderate and severe problems were registered in this domain (18.6% and 69.8%, respectively).Insufficient speech and motor development of patients with cerebral palsy has a significant impact on the formation of a child's personality. Even if the intellect of a child with cerebral palsy corresponds to age standarts, the emotional sphere is not well formed. In this connection, when studying personality factors, we also established characteristic features that depend on the forms of cerebral palsy, presented in Table 3.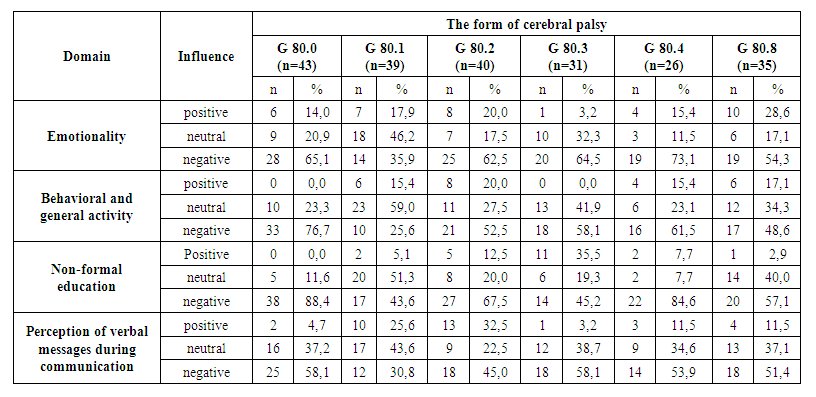 | Table 3. Features of the influence of personality factors depending on the form of cerebral palsy |
When studying the “personal factors” component, it was found that in cerebral palsy, the characteristic features of the influence of the above factor are typical, which manifested themselves depending on the topographic form of the disease. Negative emotional impact was in most cases established at G 80.4 (73.1%), G 80.0 (65.1%), G 80.3 (64.5%), G 80.2 (62.5%) and at G 80.8 (54.3%), the smallest percentage was recorded at G 80.1 (35.9%). The emotionality of children with cerebral palsy was manifested by anxiety and irritability, less often by unmotivated aggression. An identical picture was obtained in the study of activity in behavior and general activity. In the process of carrying out rehabilitation measures, in 53.7% of cases it was necessary to face the fact that activities that require the child to be purposeful led to a negative reaction; it was extremely difficult for the child to make an effort to complete what he had begun.Intellectual deficiency in children with cerebral palsy, of a disharmonious and uneven nature, was manifested not only by low cognitive activity, but also by a lack of interest in activities, slowness and a low level of concentration. Non-formal education, assessed as "negative", was registered in most cases in the forms G 80.0 (88.4%), G 80.4 (84.6%), G 80.2 (67.5%), G 80.8 (57.1%).Whereas the smallest percentage was noted in the forms G 80.1 (43.6%) and G 80.3 (45.2%) (P<0.05).Slow perception of oral messages in the process of communication and insufficient concentration of attention in children with cerebral palsy were characterized as a "negative" influence of the personality factor and in more than half of the cases were recorded in the following forms: G 80.0 (58.1%), G 80.3 (58.1%), G 80.4 (53.9%), G 80.8 (51.4%). Whereas with form G 80.1, a negative effect occurred only in 30.8% of patients.Thus, taking into account the presence of deviations in the results of determining the individual functioning profile in children with cerebral palsy using the ICF, an individual rehabilitation program plan should be developed for all patients, including recommendations for social adaptation. As part of rehabilitation, household adaptations can be used to improve the performance of the necessary self-service activities, in particular, to facilitate eating: dish holders (stationary, removable, tilting and non-tilting); grips-manipulators, drinkers with spouts, a lid and two handles; fencing for plates, plates with a deep and weighted bottom; cutlery with a wrist strap; non-slip dish mats; holders of cutlery and glasses on suction cups; waterproof bibs.The use of the ICF-DP in the rehabilitation activities of children with cerebral palsy will allow a deep study of its functionality in terms of clinical symptoms, environment and personality, as well as dynamic monitoring of changes, achieving the goal of rehabilitation at each of its stages.
References
| [1] | Borzikov V.V., Rukina N.N., Kuznetsov A.N., Belova A.N. Objectification of movement disorders in children with cerebral palsy: state of the art // Orthopedics, Traumatology and Reconstructive Surgery of Children. - 2018. - T. 6. - Issue. 1. - S. 67-66. |
| [2] | Bruikov A.A., Gulin A.V. Functional state of the cardiovascular system in children with cerebral palsy during rehabilitation // Bulletin of TSU. - 2011. - v.16, issue 1. – 374-375. |
| [3] | Idiev O.E., Makhsudov S.N., Ruzieva N.K. Results of electromyographic studies of masticatory muscles in children with cerebral palsy // Innovations in dentistry. - 2014. - No. 1. - P. 47-50. |
| [4] | Kaladze N.N., Ursina E.O., Nuvoli A.V. Characteristics of the regulation of bone metabolism in children with cerebral palsy // In the collection: Problems of medicine in modern conditions. Collection of scientific papers following the results of the international scientific-practical conference. 2015. - S. 97-105. |
| [5] | Clinical guidelines "Infantile cerebral palsy in children". Moscow. - 2016. - 35 p. |
| [6] | International classification of functioning, disability and health. World Health Organization. Geneva. Institute for the Improvement of Doctors-Experts. Saint Petersburg. 2003. - 133 p. |
| [7] | Nurmatova Sh. O., Sherova Z. N., Turabekova Sh. Kh. Inclusion of Cereton in the complex therapy of patients with cerebral palsy. – 2021. |
| [8] | Yastrebtseva I.P., Mishina I.E. The significance of the international classification of functioning, disability and health for assessing the state of human health // Bulletin of the Ivanovo Medical Academy. - 2016. - v. 21, No. 1. – pp. 25-29. |
| [9] | Adamu Sa’idu Adamu, Umar Abba Sabo, Garba Dayyabu Gwarzo, Raymond O. Belonwu. Nutritional status in cerebral palsy: A Cross-sectional comparative survey of children in Kano, Nigeria. Niger Postgrad Med J. 2018 Jul-Sep; 25(3): 156-160. doi: 10.4103/npmj.npmj_67_18. |
| [10] | Chernykh ER, Kafanova MYu, Shevela EYa, Adonina EI, Sakhno LV, Tikhonova MA, Ostanin AA. Autologous M2-like macrophage applications in children with cerebral palsy. Cell Ther Transplant. 2011; 3:e.000092.01. doi: 10.3205/ctt-2011-en-000092.01. |
| [11] | Cosmina Stănoiu. Clinical and functional aspects of evaluation and rehabilitation of spastic upper limb in children with infantile cerebral palsy. - Craiova 2012. – Р. 150. |
| [12] | Erasmus C. E., van Hulst K., Rotteveel J. J. et al. Clinical practice: swallowing problems in cerebral palsy // Eur. J. Pediatr. 2012. Vol. 171 (3): 409-414. |
| [13] | Eun-Young Park Relationship between activity limitation and health-related quality of life in school-aged children with cerebral palsy: a cross-sectional study // Park Health and Quality of Life Outcomes, 2017, 15:87 DOI 10.1186/s12955-017-0650-8. |
| [14] | Egamova M. T. et al. Game Method of Rehabilitation of Children with Infantile Cerebral Paralysis //Indian Journal of Forensic Medicine & Toxicology. – 2020. – Т. 14. – №. 4. – С. 7979-7983. |
| [15] | Ibragimov D. D. et al. Conducting immunomodulatory therapy in the complex treatment of patients with combined injuries of the Facial Bones //Central Asian Journal of Medical and Natural Science. – 2021. – Т. 2. – №. 1. – С. 132-138. |
| [16] | Iskhakova Z. S., Iskhakova F. S., Narzieva D. B. THE USE OF OSTEOGENIC MATERIAL TO REPLACE JAW CAVITY DEFECTS // Applied Information Aspects of Medicine (Prikladnye informacionnye aspekty mediciny). – 2022. – Т. 25. – №. 4. – С. 20-25. |
| [17] | Mavlyanova Z. F. Nutritional status and its condition in patients with cerebral palsy // Problems of biology and medicine. – 2019. – №. 4. – С. 216-222. |
| [18] | Mavlyanova Z., Khusinova S. Diagnostics protein and energy insufficiency cerebral palsi // InterConf. – 2020. |
| [19] | Mavlyanova Z. F. et al. Methodological and theoretical support of integrated computer information technology for monitoring and evaluation of the health status of children and adolescents involved in sports schools //Україна. Здоров’я нації. – 2020. – №. 4. |
| [20] | Shavkatovna I. M. CHARACTERISTICS OF REHABILITATION OF CHILDREN WITH CEREBRAL PALSY AND SPEECH DEFECTS //Conference Zone. – 2022. – С. 410-414. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML