-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(3): 259-264
doi:10.5923/j.ajmms.20231303.14
Received: Feb. 19, 2023; Accepted: Mar. 9, 2023; Published: Mar. 15, 2023

The Main Surgical Methods of Colorectal Cancer Treatment: Advantages and Disadvantages
M. N. Tillyashaykhov, O. A. Rakhimov, A. A. Adilkhodjaev, Ya. V. Ten, O. M. Akhmedov, T. Kh. Makhkamov, A. A. Khakimov
Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the study was to compare the clinical efficiency of laparoscopic surgery and open surgery for colorectal cancer by analyzing advantages and disadvantages of both techniques. Background. Colorectal cancer is one of the most common malignant tumors in all economically developed countries of the world and it ranks third in the structure of oncological morbidity and fourth in mortality. Surgical treatment is an efficient method of disease inhibition in patients. Various surgical methods affect oncogenesis and the prognosis of patients in different ways. Material and methods. 92 patients with histologically verified colorectal cancer treated at the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology were included in this study. The patients were divided into a Control group (open surgery, n = 46) and a Main group (laparoscopic surgery, n = 46) by randomization. Open surgery and laparoscopic surgery were used to compare and monitor clinical efficiency, Ki-67 expression obtained after surgery, as well as complications and 5-year survival. Results. The duration of the surgery (122.54 ± 14.85) min and the incision length (4.51 ± 1.065) cm in the Main group were shorter in compare with the Control group. Intraoperative blood loss in the Main group was (161.12 ± 10.694) ml versus the Control group (218.53 ± 15.369) ml (p<0.05). The patients of the Main group had a higher five-year survival rate and a lower frequency of postoperative complications compared with the Control group (for all p< 0.05). Conclusion. Videolaparoscopic interventions for colorectal cancer are not inferior in clinical effectiveness to traditional interventions: they are characterized by a reduction in the duration of surgery, a decrease in intraoperative blood loss and significantly reduce the frequency of postoperative complications, as well as the duration of hospital stay. At the same time, laparoscopic surgery can contribute to the speedy recovery of patients with colorectal cancer. Regarding the indicators of 5-year survival of patients with prognosis and the rate of proliferation of cancer cells, this method deserves clinical promotion.
Keywords: Laparoscopic surgery, Open surgery, Colorectal cancer
Cite this paper: M. N. Tillyashaykhov, O. A. Rakhimov, A. A. Adilkhodjaev, Ya. V. Ten, O. M. Akhmedov, T. Kh. Makhkamov, A. A. Khakimov, The Main Surgical Methods of Colorectal Cancer Treatment: Advantages and Disadvantages, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 259-264. doi: 10.5923/j.ajmms.20231303.14.
1. Introduction
- Colorectal cancer is one of the most common malignant tumors in all economically developed countries of the world and it ranks third in the structure of oncological morbidity and fourth in mortality [1-5]. It can affect the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and other parts of the gastrointestinal tract [6]. The positive Ki-67 index and its positive value are an expression of oncogene expression, as well as the basis of malignant biological behavior and histopathological changes of colorectal cancer. Surgical treatment is an efficient method of disease inhibition in patients. Various surgical methods affect oncogenesis and the prognosis of patients in different ways. Colorectal cancer is a malignant tumor that is often found in clinical practice. In patients with early colorectal cancer only clinical symptoms, such as bloating and dyspepsia, are observed, which rarely cause patients to pay attention to them. As a result, most patients seek hospital treatment, and their condition progresses to an advanced stage, which poses a serious threat to the patient's life. Despite the success of drug and radiation therapy, surgical treatment remains the most efficient way to treat colorectal cancer. Laparotomy has mainly been used to treat colorectal cancer for the recent years, but this method of treatment is more traumatic for the patient [7-9].Patients in the postoperative period have multiple complications, and the prognosis is not always satisfactory [10-12]. Therefore, the active study of alternative methods of colorectal cancer treatment has become the focus of clinical research [13-15]. With the continuous development of minimally invasive methods, laparoscopic surgery has become widely used in clinical treatment due to its lesser surgical injury, minor bleeding and rapid recovery of postoperative patients [8,16-17].The use of modern minimally invasive technologies in surgery allowed to increase the efficiency of surgical treatment of patients with colo-rectal cancer on the one hand by minimizing surgical injury, and on the other hand, by early rehabilitation of patients, which led to the creation of a multimodal program of early recovery or the so-called "accelerated rehabilitation of patients" after surgeries. The ideologist of this method was the Danish anesthesiologist-resuscitator Professor Henrik Kehlet. He was the first to propose the use of an accelerated rehabilitation protocol in patients and conducted a systematic analysis of the pathophysiological mechanisms of complications after elective surgical interventions [19]. It was a comprehensive program that included both preoperative preparation, surgery, and postoperative management of the patient. However, the clinical effect of laparoscopic surgery in the treatment of colorectal cancer is still controversial [21-22]. In our study, we analyzed the clinical efficiency of open surgery and laparoscopic surgery for colorectal cancer, and also conducted a comparative analysis of the long-term results of both methods of surgical treatment of colorectal cancer.The aim of the study was to compare the clinical efficiency of laparoscopic surgery and open surgery for colorectal cancer by analyzing advantages and disadvantages of both techniques.
2. Material and Methods
- This study included the treatment results of 92 patients with histologically verified colorectal cancer admitted to the Department of Coloproctology of the Republican Specialized Scientific and Practical Medical Center of Oncology and Radiology for the period from 2015 to 2021. The patients were divided into a Control group (open surgery, n = 46) and a Main group (laparoscopic surgery, n = 46) by randomization. The study was approved by the ethics committee of the center.Inclusion criteria were as follows:• Age: 18 - 75 years;• Histologically verified adenocarcinoma of the rectum and colon T1-T3, T4a N0-2, M0;• No distant metastases;• Absence of primary multiple malignant tumors;• ECOG status: 2 or below;• ASA I, II, IIIExclusion criteria were as follows:• Age under 18 and over 75 years;• Non-epithelial forms of tumors, neuroendocrine cancer of the colon and rectum;• The presence of synchronous tumors of the colon;• Complicated course of the disease;• Distant metastases;• Pregnancy and lactation;• ASA status IV and above;• HIV-infection;• Having a mental illness;• Established diagnosis of diffuse familial polyposis or Lynch syndrome.Patients of the Control group were performed open surgical interventions. Patients of the Main group underwent laparoscopic treatment. The specific procedure was as follows. First, an artificial pneumoperitoneum was applied, and the pressure in the pneumoperitoneum was maintained at about 12 mm Hg. (1 mm Hg = 0.133 kPa). Laparoscopy and instruments were performed using the 5-hole method; tumors were observed using laparoscopy to determine the localization of the tumor. Then, using an operating instrument, the blood vessels around the tumor were clamped and cut, the tumor was removed (when removing the tumor, attention was paid to the integrity of the colon and mesentery of the rectum), and the surrounding regional lymph nodes were cleaned. The area of the abdominal cavity was washed and a drainage tube was placed for drainage; in the absence of bleeding, the abdominal cavity was closed in layers. Open surgery and laparoscopic surgery were used to compare and monitor clinical efficiency, Ki-67 expression obtained after surgery, as well as complications and 5-year survival. The comparative analysis was carried out using various methods of statistical test: Student's t-test, Mann-Whitney U-test, χ2 criterion. The level of statistically significant result was considered p <0.05. Statistical data processing was carried out using programs StatPlus and IBM SPSS.
3. Results
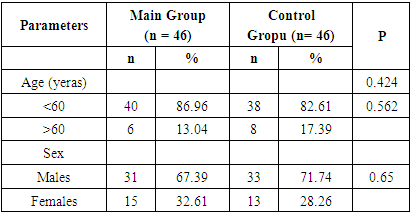
- The mean age of patients in the Main group was (56.71 ± 4.33) years and in the Control group it was (56.04 ± 3.59) years. There was no statistically significant difference between two groups (t = 0.803, p = 0.424). There were 40 (86.96%) patients under the age of 60 In the Main group. there were 38 (82.61%) patients whose age was under 60 years in the Control group. There were 31 (67.39%) men in the Main group, and 33 (71.74%) men in the Control group. There were no significant differences in age, gender between the Main and Control groups (p>0.05) (Tab.1).
|
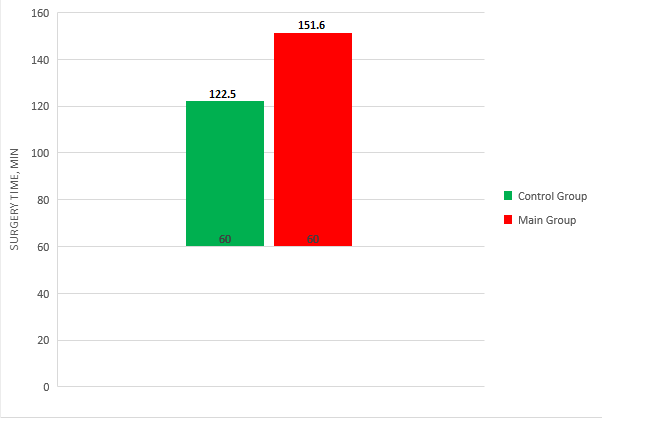 | Figure 1. Duration of surgery time |
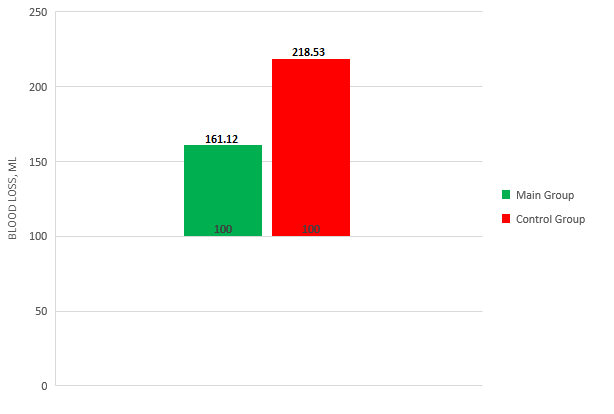 | Figure 2. Intraoperative blood loss |
|
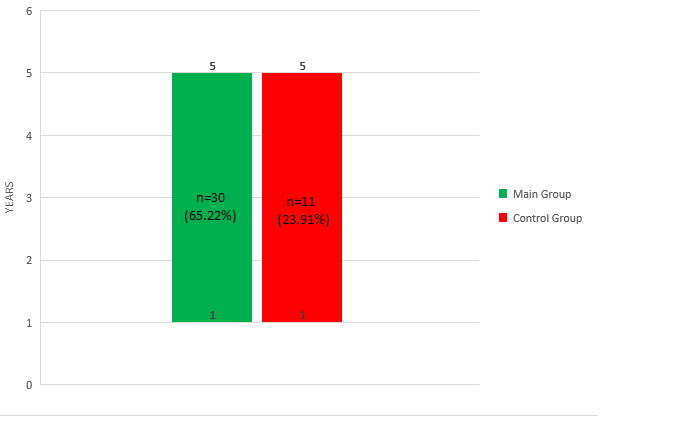 | Figure 3. 5-year survival rate |
4. Discussion
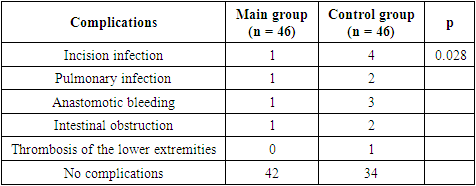
- As it is known, the pathogenesis of colorectal cancer is mainly associated with chronic inflammation of the colon, colorectal adenoma, genetic factors. technologies of minimally invasive approaches using endoscopic techniques have become increasingly interesting for recent years, which allows to increase the efficiency of surgical treatment due to better visualization and more precise work of the surgeon [23].However, it is necessary to take into account the specifics of the affected part in radical surgery to improve the prognosis. The elimination of postoperative complications and the frequency of relapses negatively affects the quality of patients life. The use of laparoscopic video-assisted surgical intervention not only allows detecting small formations that cannot be detected during open surgery, but also has a comparative advantage in reducing the frequency of local relapses and surgical operation of the tumor [2,24-27].The results of our study showed that the duration of the surgery and the length of the incision in the Main group were shorter than in the Control group, and the difference was statistically significant. The amount of intraoperative blood loss in the Main group was lower than in the Control group, and the difference was also statistically significant. The results obtained indicate that, in comparison with open surgery, the duration of the operation and the length of the incision during laparoscopic surgery are shorter, and the volume of intraoperative blood loss is less.The results of this study also showed that the incidence of complications in the Main group was lower than in the Control group, and the difference was statistically significant. The results obtained indicate that laparoscopic surgery is a safe method in compare with traditional open surgery.The 5-year survival rate in the Main group was 65.22% (30/46) versus the same indicators of the Control group (23.91% (11/46)). The difference was statistically significant (p<0.05).
5. Conclusions
- Videolaparoscopic interventions for colorectal cancer are not inferior in clinical effectiveness to traditional interventions: they are characterized by a reduction in the duration of surgery, a decrease in intraoperative blood loss and significantly reduce the frequency of postoperative complications, as well as the duration of hospital stay. At the same time, laparoscopic surgery can contribute to the speedy recovery of patients with colorectal cancer.Regarding the indicators of 5-year survival of patients with prognosis and the rate of proliferation of cancer cells, this method deserves clinical promotion.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML