Nazira T. Rikhsieva1, Rakhmatilla Sh. Rikhsiev2
1Assistant at the Department of Endocrinology with Pediatric Endocrinology, Tashkent Pediatric Medical Institute, Uzbekistan
2Head of the Radiology Department of the Tashkent Clinical Hospital, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Primary hyperparathyroidism is one of the most common pathologies of the endocrine system, and therefore, our work reflects the results of surgical treatment of this pathology.
Keywords:
Primary hyperparathyroidism, Complications, Analysis, Children
Cite this paper: Nazira T. Rikhsieva, Rakhmatilla Sh. Rikhsiev, Results of Surgical Treatment of Primary Hyperparathyroidism in Children, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 249-258. doi: 10.5923/j.ajmms.20231303.13.
We set ourselves the goal of studying the immediate and long-term results of surgical treatment of primary hyperparathyroidism.
1. Materials and Methods of Research
A retrospective analysis of the case histories of 103 patients with suspected PHPT, who were hospitalized at RSPPMCE, was carried out. Among 90 patients with a confirmed diagnosis included in the study (for the period from 1999 to 2014), 50 children underwent surgical treatment. The average age of the patients was (12.8±1.2 years). Forty of them refused the operation and were under observation. 13 children were diagnosed with various hereditary diseases. The immediate and long-term results after surgical treatment were studied and discussed.
2. Research Results
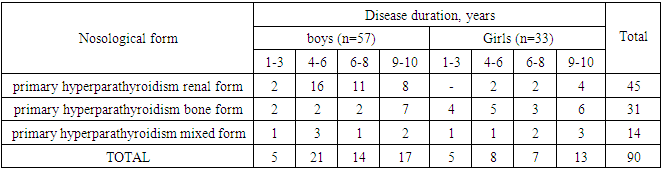
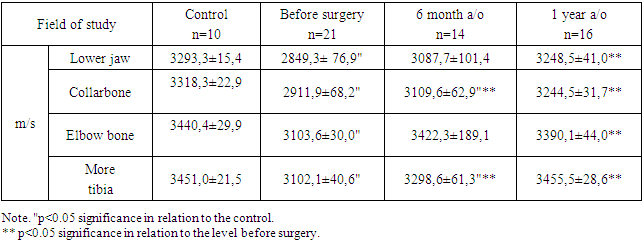
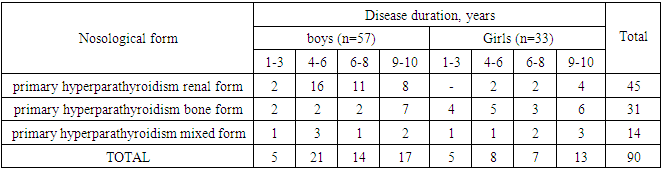
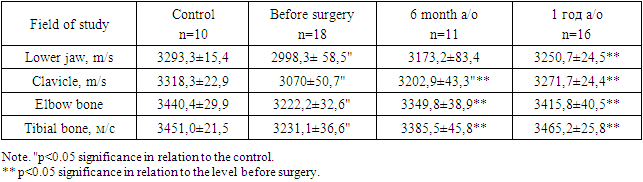
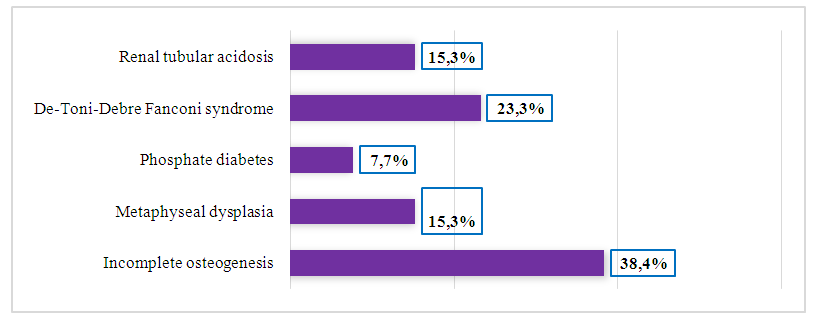
According to the case histories, an analysis of anthropometric (weight, height, body mass index (BMI)), laboratory and radioimmunological parameters (PTH, CT, VitD3, levels of total calcium and phosphorus in the blood, Ca ++, alkaline phosphatase (AP) and indicators of daily calciuria).All patients diagnosed with PHPT (33 girls, 57 boys) were divided into three groups: patients with bone form, patients with renal form, patients with mixed form of PHPT (bone + kidney). The distribution of patients into groups was carried out on the basis of criteria proposed by domestic and foreign associations [2,10,13]. PHPT of the renal form was diagnosed in 45 (43.6%) children (mean age 6.1±3.2 years), including 8 girls and 37 boys. Bone form of PHPT was detected in 31 (30.3%) patients (mean age 12.7±1.2 years), including 18 girls and 13 boys. Mixed form of PHPT was found in 14 (13.5%) children, (mean age 13.2±1.1 years), including 7 girls and 7 boys. The control group consisted of 10 children without parathyroid pathology. The average age is 10.8±0.9 years. Fig. 1.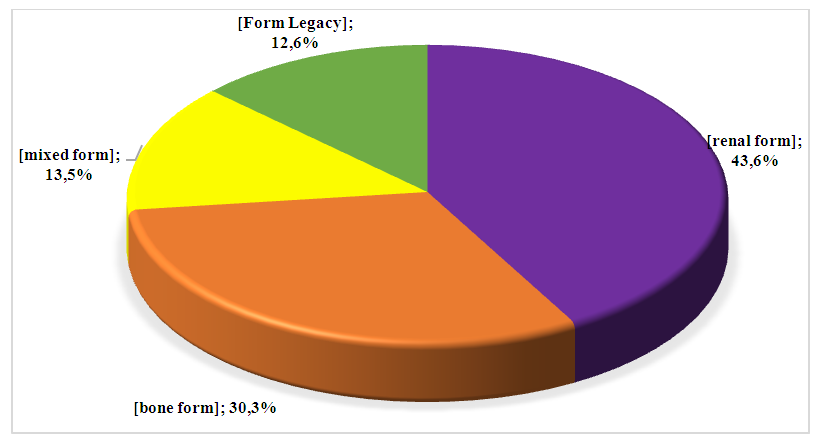 | Figure 1. Distribution of various forms of primary hyperparathyroidism and osteogenesis imperfecta in children |
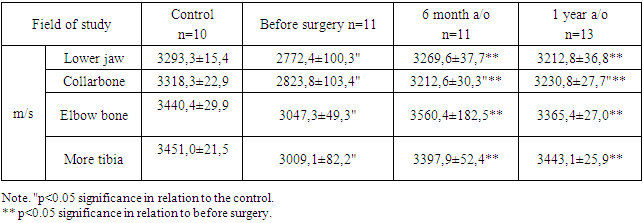
Among those examined with suspected primary hyperparathyroidism, 13 (12.6%) children had various hereditary diseases: osteogenesis imperfecta was detected in 5 (38.4%), craniometaphyseal dysplasia - in 2 (15.3%), rickets-like diseases - renal tubular acidosis - in 2 (15.3%), de Toni - Debre - Fanconi syndrome - in 3 (23.3%), phosphate-diabetes - in 1 (7.7%). Fig. 2.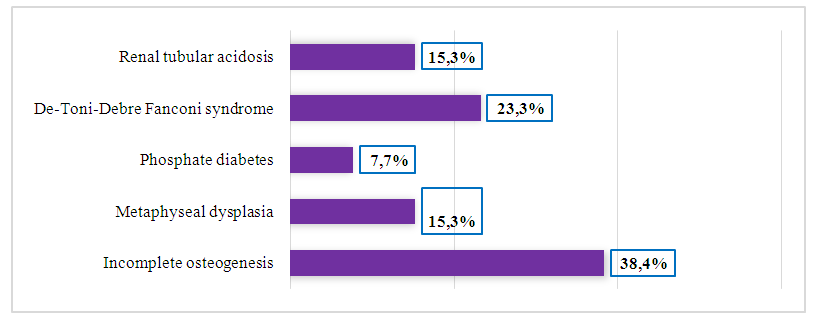 | Figure 2 |
Osteogenesis imperfecta was found without pronounced skeletal deformities. In 2 patients, saber deformities of the legs were noted.Patients from families with closely related marriages suffered from cranio-metaphyseal dysplasia. They have scoliosis, valgus deformities of the lower extremities, enlargement of large joints, chest deformities, and delayed physical and motor development.Two of the patients with renal tubular acidosis were from consanguineous families.Clinical manifestations of the de Toni-Debre-Fanconi syndrome included polyuria, polydipsia, hypoisostenuria, and episodes of fever. There was a sharp deficit in height and weight, signs of intoxication, decreased muscle tone, hyporeflexia. The data show that the main problems in the diagnosis of bone forms of primary hyperparathyroidism were hereditary systemic diseases of the skeleton (imperfect osteogenesis and craniometaphyseal dysplasia), which, like primary hyperparathyroidism, were accompanied by fractures, osteopathy, and osteoporosis.The study of anamnesis in 90 patients with various forms of primary hyperparathyroidism showed that the duration of clinical manifestations of the disease reached 8-10 years and averaged 6.8 ± 3.2 years. Severe course of primary hyperparathyroidism and complicated forms accounted for 72.6% of cases. Table 1.Table 1. Distribution of sick children with primary hyperparathyroidism according to the duration of the disease
 |
| |
|
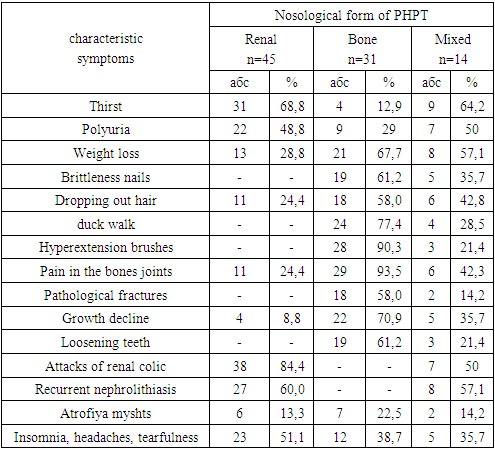
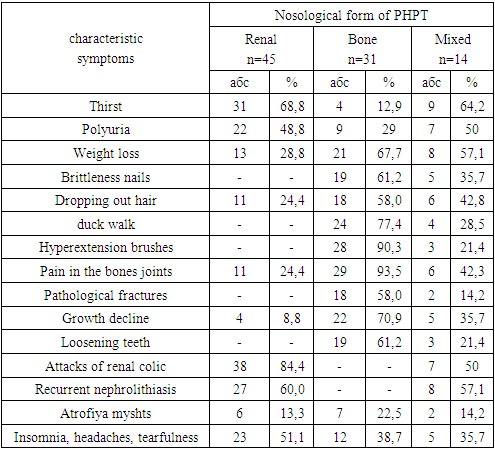
Among the erroneous diagnoses made to patients at the stages of preliminary examination, there were diseases of the spine and joints (14 patients), diabetes insipidus (3 patients), urolithiasis (16 patients), chronic calculous cholecystitis (2 patients), biliary pancreatitis (2 patients) and goiter (3 patients) [6,4,14,18].The analysis of the material shows that one of the reasons for erroneous diagnosis at the stages of preliminary examination is the incorrect interpretation of clinical, echographic and radiological symptoms by doctors, which, as a rule, were assessed in isolation, without taking into account the whole complex of manifestations of PHPT observed in most patients.According to some authors, [3,5,7,9] there is still a large group of patients who have been observed for years for osteoporosis, undergo repeated surgical interventions for nephrolithiasis, bone pathology, suffer from constant exacerbations of peptic ulcers, chronic calculous cholecystitis, pancreatitis and fall into the scope of attention of endocrine surgeons with deep disabilities. An analysis of the clinical data of patients with a confirmed diagnosis of primary hyperparathyroidism made it possible to identify a group of symptoms, the combination of which makes it possible to suspect the pathology of the parathyroid gland. Severe damage to the skeletal system was observed in 20 (22.2%) patients who were treated for a long time for osteoporosis and had numerous fractures. As a result of osteoporosis of the bones and, first of all, of the vertebral bodies, as well as deformities of the limbs, 31 (34.4%) patients showed a decrease in height by 4-8 cm. Pain in the bones and joints was detected in 46 (51.1%) patients, hair - in 35 (38.8%), fragility of nails - in 24 (26.6%). Attacks of renal colic were noted in 45 (50%) patients, bilateral, multiple, recurrent nephrolithiasis was detected in 35 (38.8%). The neuropsychic status in primary hyperparathyroidism in 40 (44.4%) patients was characterized by insomnia, headaches and tearfulness. Table 2.Table 2. The frequency of clinical symptoms of primary hyperparathyroidism in children in a comparative aspect
 |
| |
|
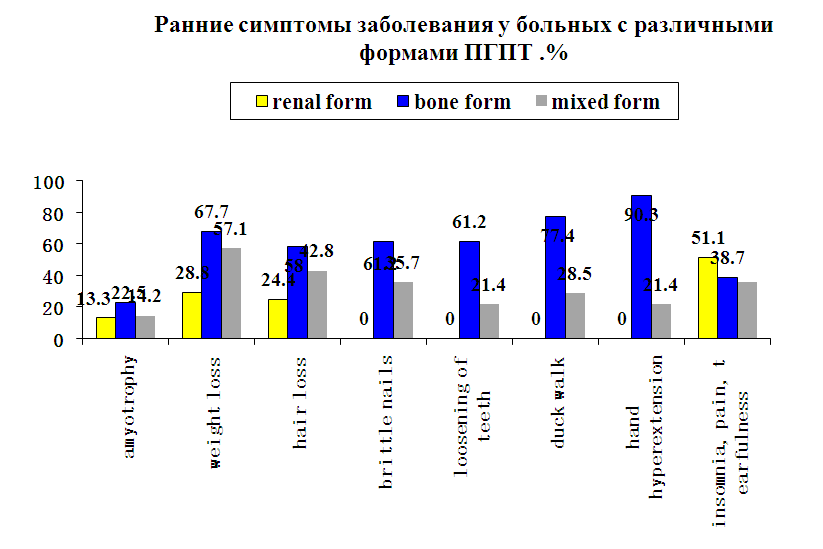
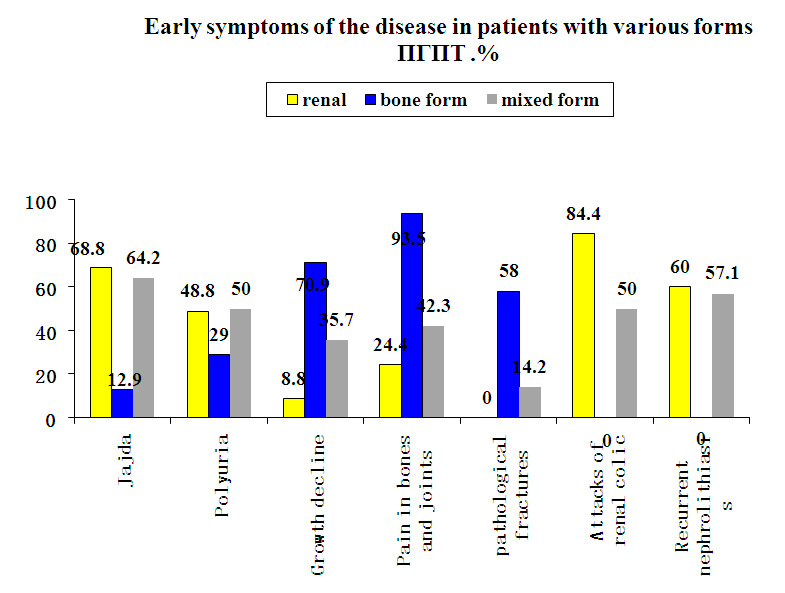
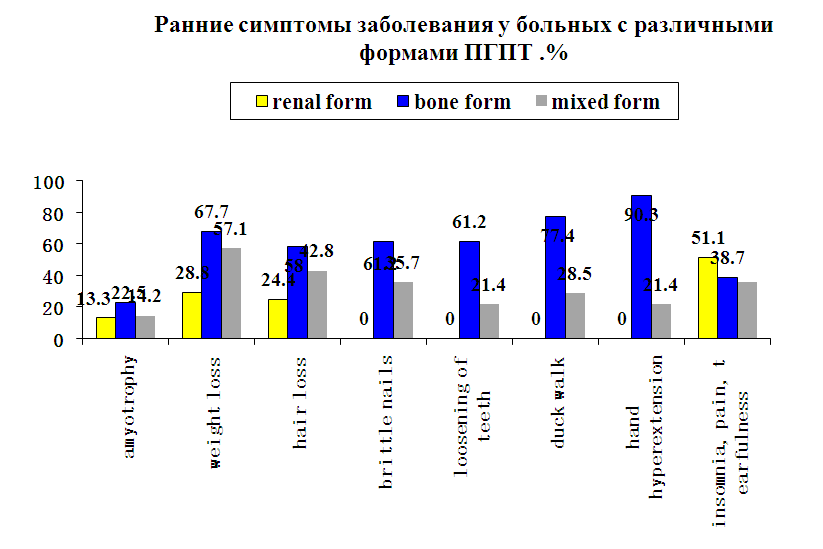
Our analysis showed that hyperparathyroidism in children is characterized by multiple symptoms. In children with the renal form of primary hyperparathyroidism, thirst and polyuria were recorded more often than bone and mixed forms. Pain in the bones and joints, as well as brittle nails, respectively, were more common in children with the bone form of primary hyperparathyroidism. Recurrent nephrolithiasis was observed more often in patients with renal form than in the comparison group (Fig. 3., Fig. 4.).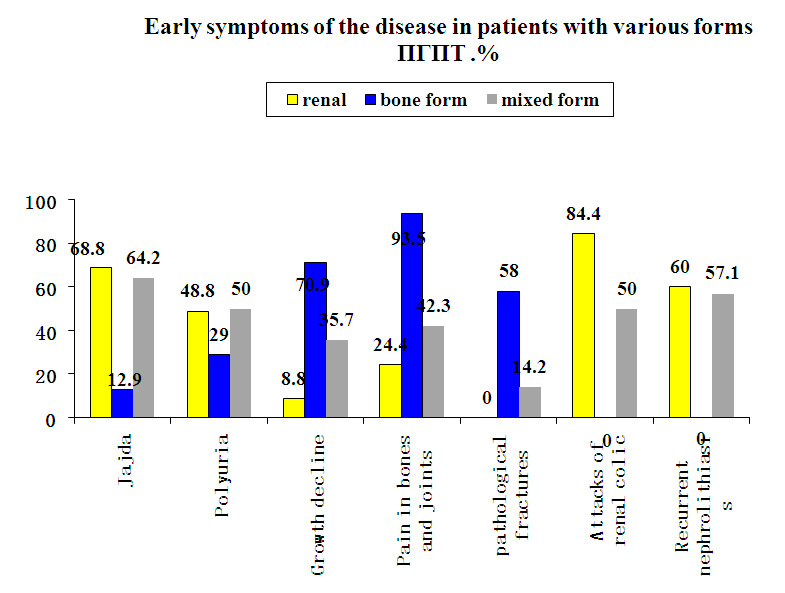 | Figure 3 |
 | Figure 4 |
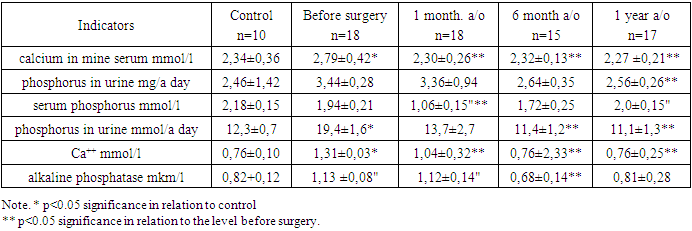
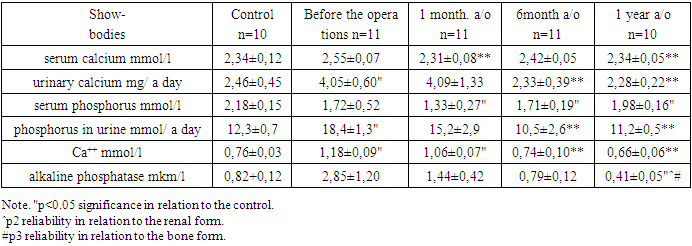
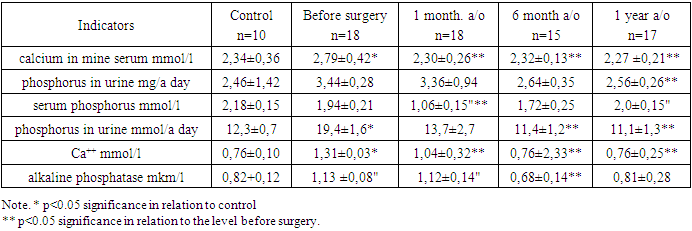
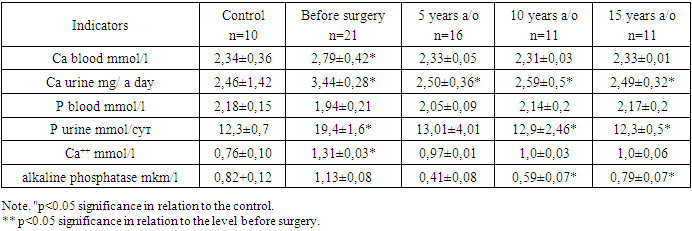
Thus, a retrospective analysis established the predominance of the manifest form of primary hyperparathyroidism in children in the Uzbek population. It was found that the renal form (43.6%) of the disease is observed more often than the bone form (30.3%), in 16.7% of cases hyperparathyroidism of the mixed form was detected. The analysis showed that hyperparathyroidism in children is characterized by multiple symptoms, the clinical course is characterized by a large number of complicated forms (78.6%), while the diagnosis of the disease is delayed by 9–10 years.It is known that hyperparathyroidism in children is characterized by a change in the indicators of calcium-phosphorus metabolism (hypercalcemia, hypophosphatemia, increased activity of blood alkaline phosphatase, hyperphosphaturia, hypercalciuria) [1,15,17,16]. The analysis of these diagnostically significant data in children observed for hyperparathyroidism was carried out.Prior to surgical treatment, hypercalcemia was determined in 90% of patients with renal form of hyperparathyroidism. The average level of total Ca was significantly (2.79±0.42 mmol/l; p<0.05) higher than the control values (2.34±0.36 mmol/l). After parathyroidectomy, the calcium content significantly decreased compared to the level before surgery and remained close to the control throughout the study period. Table 3.Table 3. Dynamics of biochemical parameters in sick children with primary hyperparathyroidism of the renal form in the short term after surgery
 |
| |
|
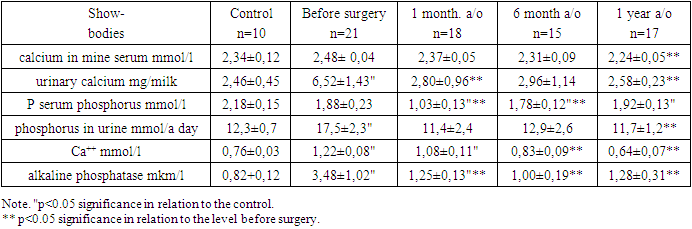
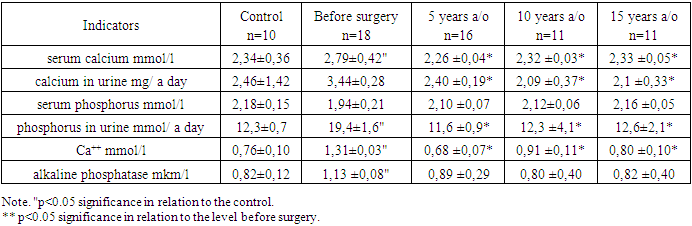
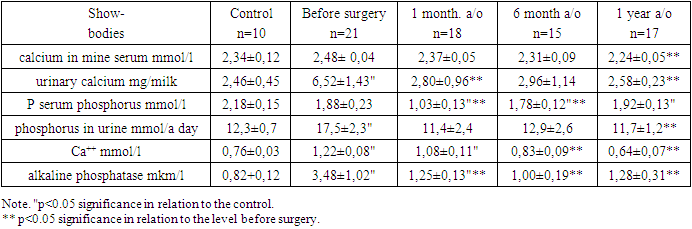
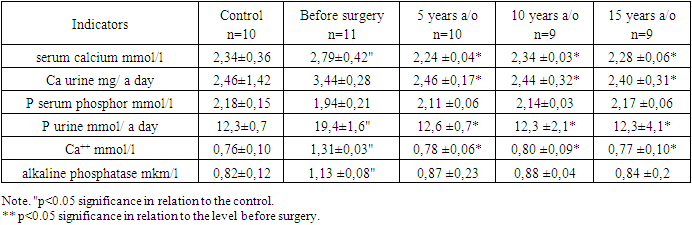
It is known from the literature that the determining factor in clinical practice is the concentration of Ca++ in plasma, since this is the only biologically active constant in various target organs [6,20].Before surgery, in all patients of this group, the level of ionized Ca (1.31±0.03 mmol/l) was statically significantly (p<0.05) higher than the control values (0.76±0.10 mmol/l). Later (1 month, 6 and 12 months after the operation) there was a tendency to a significant decrease in Ca++ (1.04±0.32 mmol/l; 0.76±0.33 mmol/l and 0.76±0. 25 mmol/l; p<0.05).Hypercalciuria was typical for 72% of children with renal form of hyperparathyroidism. Hypocalciuria was observed in 22.2% of cases. A significant decrease was revealed only a year after the operation (2.56±0.26 mg/day; p<0.05).There is a close inverse relationship between plasma phosphate concentration and renal reabsorption. Suppression of reabsorption of inorganic phosphate is accompanied by the development of phosphaturia, which leads to hypophosphatemia [11,12].Hypophosphatemia was found in 77.7% of patients. Before the operation, the average value of phosphorus (1.94±0.21 mmol/l) in the blood of children in this group did not differ significantly from the control (2.18±0.15 mmol/l). However, after 1 month this indicator (0.92±0.15 mmol/l) was significantly lower than both the control and the level before surgery.The majority (72.2%) of children in this group had hyperphosphaturia before surgery. The content of phosphorus (19.4±1.6 mmol/day; p<0.05) in the urine before surgery significantly exceeded the control values (12.3±0.7 mmol/day). Only 12 months after the operation, a significant decrease in phosphorus in the urine was observed (11.1±1.3 mmol/day; p<0.05).According to the literature, an increase in the activity of alkaline phosphatase is considered a sign of osteodystrophy, and its level reflects the severity of the processes of bone formation, bone resorption and demineralization [16,19,20].In 61.1% of children with renal form of hyperparathyroidism, high activity of alkaline phosphatase was found, and in 30% - low activity. The level of alkaline phosphatase (1.13±0.08 µm/l; p<0.05) before surgery was significantly higher than that in the control (0.82±0.12 µm/l). A slight decrease in the activity of alkaline phosphatase (1.12±0.14 µm/l) was registered 1 month after the operation. A significant decrease in the level of alkaline phosphatase (0.68±0.14 μm/l) was detected only 6 months after the operation.In 66.6% of patients with the bone form of hyperparathyroidism, hypercalcemia and hypercalciuria were recorded, the level of ionized calcium was high in 85.7% of cases. Decreased levels of Ca in the blood, urine and Ca++ were found in 24.1%, 33.4% and 14.3% of children, respectively.Hypophosphatemia and hyperphosphaturia were typical for 78.1% and 76.8% of patients with CF. High activity of alkaline phosphatase was detected in 77.6% (Table 4).Table 4. Dynamics of biochemical parameters in sick children with primary hyperparathyroidism of the bone form in the short term after surgery
 |
| |
|
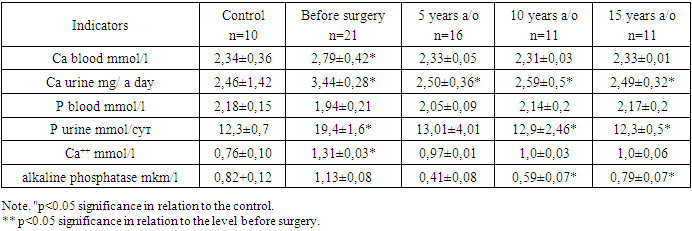
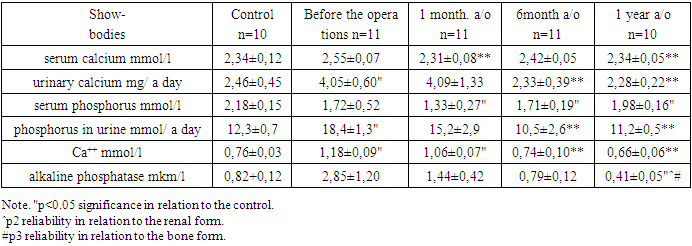
After the operation, the content of total and ionized Ca returned to normal after 6-12 months. The concentration of phosphorus remained significantly low compared with the norm for the entire period of observation of the patient. The level of Ca and P in the urine after surgery changed in waves with a slight increase after 6 months.Parathyroidectomy led to a significant decrease in the activity of alkaline phosphatase, but it remained elevated relative to the norm.Analysis of the biochemical parameters of children with a mixed form of hyperparathyroidism in most of them showed: hypercalcemia (85.7%), hypercalciuria (69.2%), hypophosphatemia (92.9%), hyperphosphaturia (92.9%), increased Ca++ (92.9%) and high ALP activity (78.6%) (Table 5).Table 5. Dynamics of biochemical parameters in sick children with primary hyperparathyroidism of a mixed form in the short term after surgery
 |
| |
|
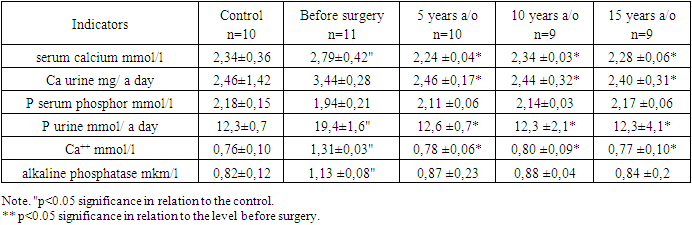
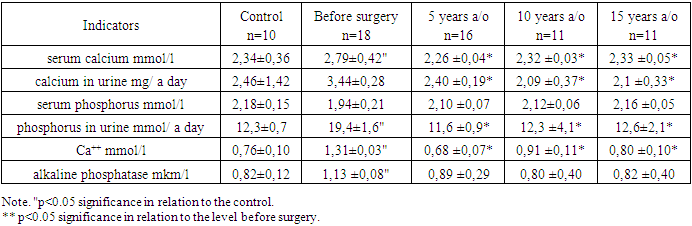
1 month after the operation, the level of Ca in the blood returned to normal, and after 6 months the concentration of ionized calcium and alkaline phosphatase. The content of phosphorus in the blood remained stably low. A significant decrease in Ca and P in the urine was observed 6 months after the operation.Dynamic observation of patients with hyperparathyroidism (for 15 years) showed that after surgery, the level of Ca and P in the blood in all forms of the disease corresponds to the control values. (Table 6).Table 6. Dynamics of biochemical parameters in sick children with primary hyperparathyroidism of the renal form in the long-term after surgery
 |
| |
|
Table 7. Dynamics of biochemical parameters in sick children with primary hyperparathyroidism of the bone form in the long-term after surgery
 |
| |
|
Table 8. Dynamics of biochemical parameters in sick children with mixed primary hyperparathyroidism in the long-term after surgery
 |
| |
|
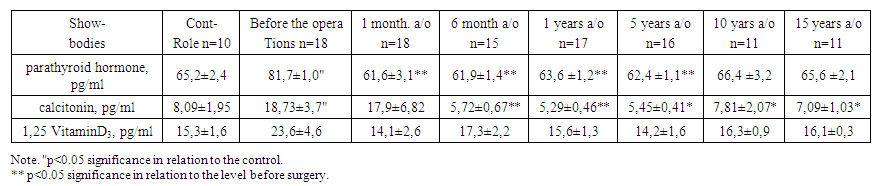
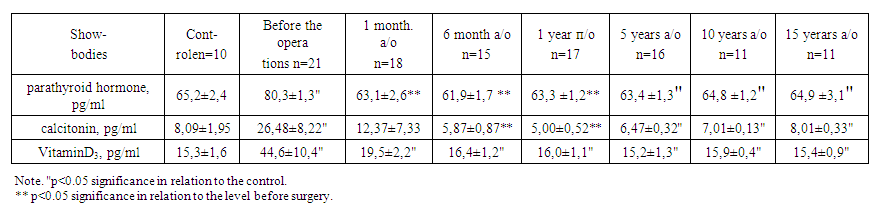
Thus, pronounced changes in the balance of calcium, phosphorus and alkaline phosphatase in children with mixed (in 85.7% of cases), renal (78.0%) and bone (72.7%) forms of primary hyperparathyroidism indicate deep disturbances in the regulation system. phosphorus-calcium homeostasis. The analysis performed showed a positive effect of parathyroidectomy on calcium-phosphorus metabolism.Parathyroid hormone and calcitonin regulate phosphorus-calcium metabolism in the body. Parathyroid hormone affects the level of calcium in the blood, contributing to its increase. Stimulates the activation of vitamin D, which is necessary for the normal functioning of the skeletal system. Calcitonin affects the level of phosphorus in the blood, and is also able to retain calcium ions in the bones, preventing their destruction when exposed to a number of adverse factors [7,14,19].It has been repeatedly confirmed that primary hyperparathyroidism is often associated with a lack or deficiency of vitamin D. Concomitant vitamin D deficiency can lead to a more pronounced increase in parathyroid hormone and aggravate the clinical picture of the disease, primarily due to a decrease in bone mineral density [1,3,5].There are also cases when, with primary hyperparathyroidism, vitamin D in the blood is within the normal range, or elevated. The mechanism for the development of this condition is explained as follows: an increased content of parathyroid hormone leads to an increase in the activation of vitamin D in the kidneys with the formation of an active metabolite - calcitriol, which has such a powerful activity that it is considered a hormone. In turn, an increase in the level of the active form of vitamin D significantly enhances the absorption of calcium in the intestine, leading to a pronounced increase in calcium in the blood [8,17,10].Before surgery, patients with renal form of hyperparathyroidism had elevated levels of parathyroid hormone (92.9%), calcitonin (72.2%), and VitD3 (66.7%).Only the average values of parathyroid hormone (81.7±1.0 pg/ml, at a rate of 65.2±2.4 pg/ml) and calcitonin (18.7±3.7 pg/ml) differed statistically significantly from the control upwards, at a rate of 8.09±1.95 pg/ml). Parathyroid hormone normalized 1 month after the operation, and calcitonin normalized 6 months later (Table 9).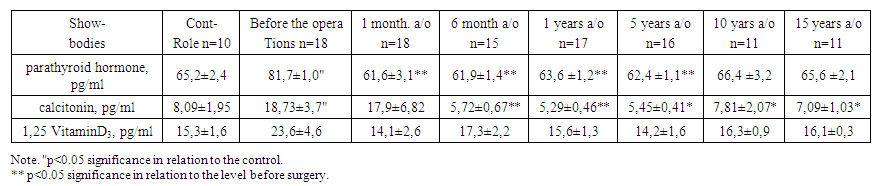 | Table 9. Radioimmunological parameters of blood serum in sick children with primary hyperparathyroidism of the renal form at various times after surgery |
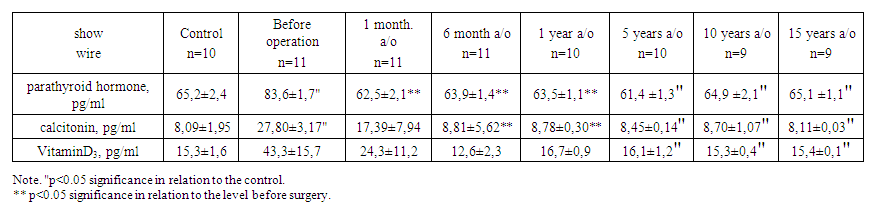
It should be noted that after 5 years, the concentration of calcitonin (3.4 times) and VitD3 (1.7 times) decreased relative to the level before surgery.In the long term (5-10-15 years), the average level of parahormone was significantly lower than before surgery.In 75.0% and 87.5% of children with the bone form of primary hyperparathyroidism, an increased concentration of parathyroid hormone and calcitonin in the blood was found. A high level of Vitamin D3 was detected in 88.9% of patients, respectively.Radioimmunological parameters before surgery were significantly higher compared with the control. 1 month after the operation, there was a trend towards a decrease in the level of parathyroid hormone, calcitonin, and after 6 months their normalization was noted (Table 10). After 12 months, the concentration of calcitonin and parathyroid hormone decreased relative to the level before surgery by 5.3 and 1.3 times, and in the long term (5-10-15 years) it was closer to the control group.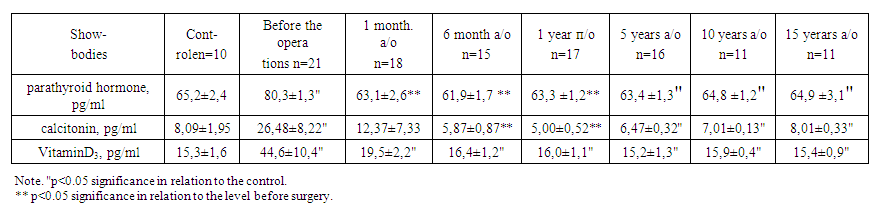 | Table 10. Radioimmunological parameters of blood serum in sick children with primary hyperparathyroidism of the bone form at various times after surgery |
All patients with a mixed form of hyperparathyroidism were found to have high levels of parathyroid hormone, calcitonin, and Vitamin D3. (Table 11.). The concentration of parathyroid hormone decreased to normal values 1 month after the operation, and calcitonin - after 6 months. In the long-term results (5-10-15 years), parathyroid hormone, calcitonin, Vitamin D3 did not significantly differ from the control group and varied within the normal range.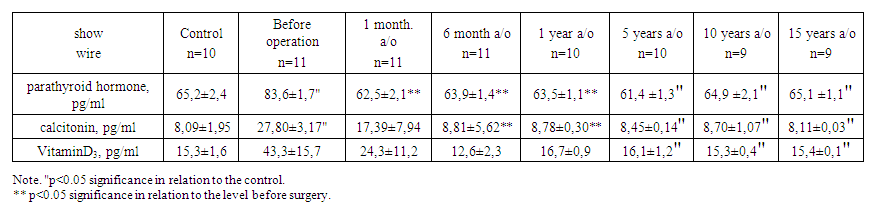 | Table 11. Radioimmunological parameters of blood serum in sick children with mixed primary hyperparathyroidism at various times after surgery |
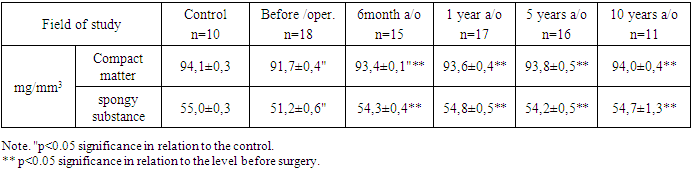
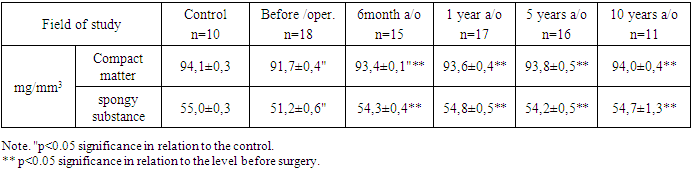
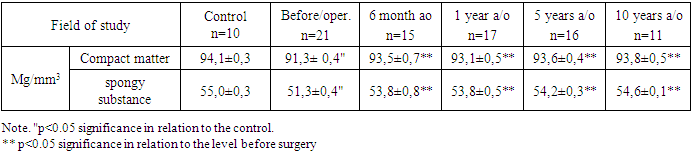
Thus, an increased content of calcium-regulating hormones (in the mixed form in 100% of cases, in the bone form in 86.4% of cases, in the renal form in 78.0% of cases) indicates a violation of the functional activity of the parathyroid gland. Dynamic observation of patients after surgery showed the presence of positive changes in the level of calcium-regulating hormones.Changes in the skeleton in hyperparathyroidism are an important and fairly common symptom of this disease. The X-ray picture of skeletal changes in primary hyperparathyroidism is, to a certain extent, a reflection of pathological changes. Even with pronounced radiological manifestations, the recognition of this disease causes certain difficulties [17]. X-ray examination of children with primary hyperparathyroidism revealed systemic osteoporosis in 30% of cases, subperiosteal resorption of the nail phalanges of the hands in 46.7%, thinning of the cortical layer was found in 100% of cases.Subperiosteal resorption is a characteristic and rather early sign of hyperparathyroidism, and its diagnostic value is equated to a symptom of hypercalcemia [12].Cysts and brown bone tumors (a specific symptom for primary hyperparathyroidism) were not detected in any case of the disease in children. The bone age deficit was 3-4 years.For the purpose of early diagnosis of changes, it was quantified by two methods: a) densitometry and b) echoosteometry. The densitometry method makes it possible to detect bone lesions only when at least 3-5% of the bone substance is lost. According to X-ray densitometry in sick children, osteoporosis was diagnosed in 80% of cases. In the control group, the indicators of the mineral density of the spongy substance (HS) were 55.0 ± 0.3 mg/mm, and the compact (CV) 94.1 ± 0.3 mg/mm3.The mineral density of the compact and spongy substance was reduced in 72.0% and 82.0% of children with renal form of primary hyperparathyroidism, respectively. Before the operation, the mineral density of the compact substance was 91.7±0.4 mg/mm3, that of the spongy substance was 51.2±0.6 mg/mm3. Dynamic observation 6 months after the operation showed the restoration of bone mineral density to control values. A positive result was maintained in the long term (5-10 years) after parthyroidectomy. Table 12.Table 12. Indicators of bone mineral density in sick children with primary hyperparathyroidism of the renal form before and after surgery in dynamics
 |
| |
|
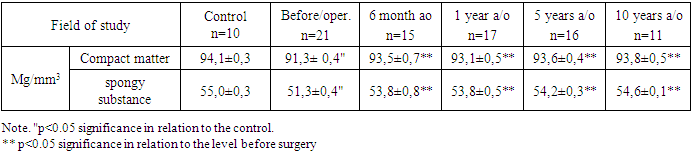
In the group of children with the bone form of PHPT, the mineral density of the compact substance was reduced in 90.9% of cases, and that of the spongy substance, in 95.5% (Table 13).Table 13. Indicators of bone mineral density in sick children with primary hyperparathyroidism of the bone form before and after surgery in dynamics
 |
| |
|
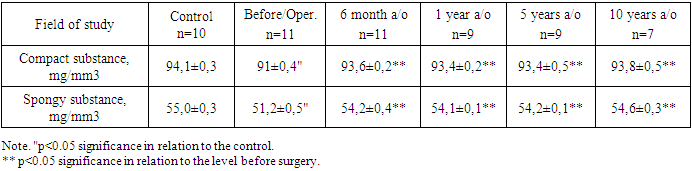
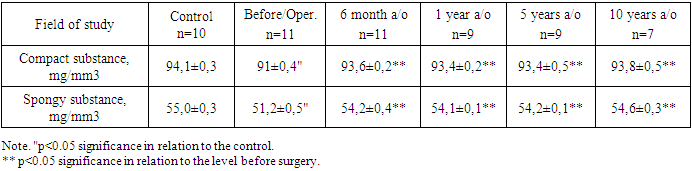
In 85.7% and 100% of children with a mixed form of the disease, respectively, a decrease in the mineral density of the compact and spongy substance was found. (Table 14).Table 14. Indicators of bone mineral density in children with mixed PHPT before and after surgery in dynamics
 |
| |
|
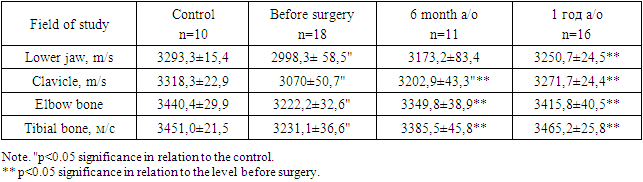
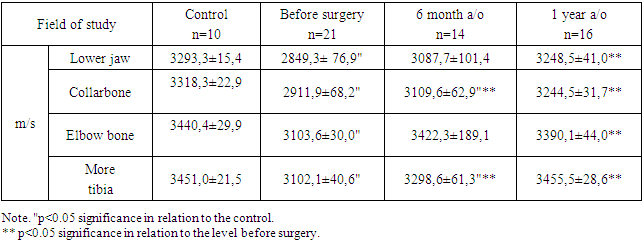
6 months after the operation, the mineral density of the compact and spongy substance increased and remained, in the future, within the control values.The data obtained indicate the restoration of bone tissue in the majority of operated children with primary hyperparathyroidism in the long term after parathyroidectomy.According to echoosteometry, the vast majority of patients with the renal form showed a decrease in the passage of an ultrasound wave in the tibia (64.7%) and ulna (58.8%), clavicle (52.9%) and mandible (94.1%). Restoration of the bone tissue structure was found one year after the operation. (Table 15).Table 15. Velocity of ultrasound propagation in sick children with primary hyperparathyroidism of the renal form before and after surgery in different periods of observation
 |
| |
|
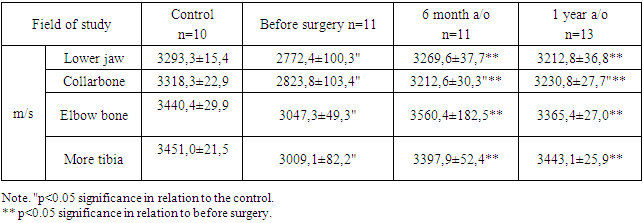
Echoosteometry showed a decrease in the speed of passage of ultrasound in all examined bones in patients with a bone form. After 6 months, restoration of the structure of the tibia and clavicle was noted, and after a year of the ulna and lower jaw. (Table 16).Table 16. Indicators of ultrasound propagation velocity in sick children with primary hyperparathyroidism of the bone form in different periods of observation
 |
| |
|
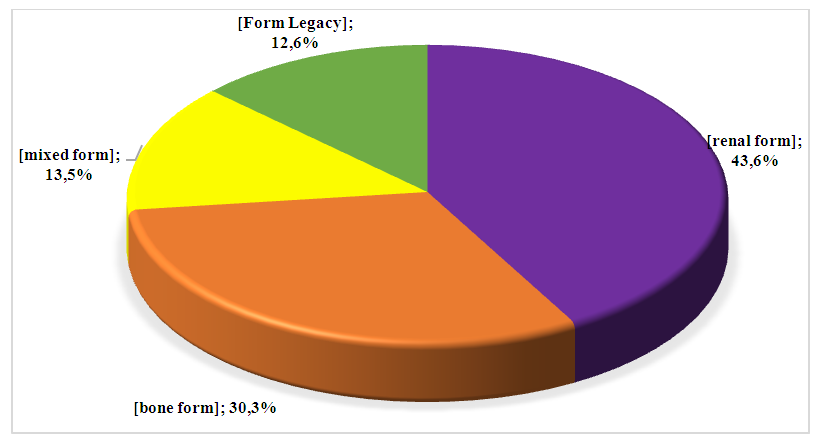
A decrease in the speed of passage of ultrasound was noted in all the examined bones. After the operation, restoration of the bone structure was found in 80-90% of cases. (Table 17).Table 17. Indicators of ultrasound propagation velocity in sick children with mixed primary hyperparathyroidism before and after surgery in dynamics
 |
| |
|
Before surgery, all children in this group showed a decrease in the speed of ultrasound transmission in the bones. After 6 months, restoration of the structure of the examined bones was found.Conclusions: Based on a thorough study of the immediate and long-term results of parathyroidectomy, it was found that the vast majority of patients have a positive dynamics of clinical manifestations and normalization of biochemical parameters.Dynamic monitoring of sick children after surgical removal of the PTG tumor showed stabilization of resorptive, destructive and reparative processes in bone structures.Parathyroidectomy is undoubtedly the most effective treatment for PHPT in children today.
References
| [1] | Alaev, D. S. Nephrolithiasis in primary hyperparathyroidism / D. S. Alaev, I. V. Kotova // Almanac of Clinical Medicine. - Moscow, 2013. - No. 28. - P. 58-60. |
| [2] | Use of preoperative parathyroid fine-needle aspiration and parahormone assay in primary hyperparathyroidism with concomitant thyroid nodules / Y. Erbil [et al.] // Am. J. Surg. — 2007. — Vol. 193, № 6. — Р. 665–671. |
| [3] | Utility of ultrasound-guided fine-needle aspiration of parathyroid adenomas for localization before minimally invasive parathyroidectomy / D. Abraham [et al.] // Endocr. Pract. — 2007. — Vol. 13, № 4. — Р. 333–337. |
| [4] | Diagnostic Perfomance of 4D CT and Sestamibi SPECT/CT in localizing Parathyroid Adenomas in Primary Hyperparathyroidism? Radiology 2019; 291: 496-476. |
| [5] | Bilezikian JP, Silverberg SJ. Normocalcemic primary hyperparathyroidism. Arquivos Brasileiros De Endocrinologia & Metabologia. 2010; 54(2): 106-109. doi: 10.1590/s0004-27302010000200004. |
| [6] | Bilezikian JP, Brandi ML, Eastell R, Silverberg S, Udelsman R, Marcocci C and Potts Jr JT. Guidelines for the Management of Asymptomatic Primary Hyperparathyroidism: Summary Statement from the Fourth International Workshop. J Clin Endocrinol Metab. Oct; 99(10): 3561-9. doi: 10.1210/jc.2014-1413. |
| [7] | Rozhinskaya L, Pigarova E, Sabanova E, et al. Diagnosis and treatment challenges of parathyroid carcinoma in a 27-year-old woman with multiple lung metastases. Endocrinol Diabetes Metab Case Rep. 2017; 2017. pii: 16-0113. https://doi.org/10.1530/EDM-16-0113. |
| [8] | Maruani G, Hertig A, Paillard M, Houillier P. Normocalcemic primary hyperparathyroidism: evidence for a generalized targettissue resistance to parathyroid hormone. J Clin Endocrinol Metab. 2003; 88(10): 4641-4648. doi: 10.1210/jc.2002-021404. |
| [9] | Clarke B.L. Epidemiology of primary hyperparathyroidism. J ClinDensitom. 2013; 16(1): 8-13. |
| [10] | Tordjman KM, Greenman Y, Osher E, et al. Characterization of normocalcemic primary hyperparathyroidism. The American Journal of Medicine. 2004; 117(11): 861-863. doi: 10.1016/j.amjmed.2004.06.037 32. Amaral LM, Queiroz DC, Marques T. |
| [11] | Pasieka J.L. and Moosa Khalil. Parathyroid carcinoma (Book Chapter 26). Springer – Verlag Berlin Heidelberg. 2012; 311–2. |
| [12] | N.T. Rikhsieva, S.I. Ismailov АNALYSIS OF THE QUALITY OF LIFE OF CHILDREN WITH PRIMARY HYPERPARATHYROIDOSIS IN LONG PERIODS AFTER PARATYREOIDECTOMY Journal of Biomedicine and Practice. 2021, vol. 6, issue 3, pp. 522-527. |
| [13] | Lowe H, Mcmahon DJ, Rubin MR, et al. Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J Clin Endocrinol Metab. 2007; 92(8): 3001- 3005. doi: 10.1210/jc.2006-2802. |
| [14] | Pashtan I., Grogan R.H., Kaplan S.P. et al. Primary hyperparathyroidism in adolescents: the same but diff erent. Pediatr Surg Int. 2013; 29 (3): 275-279. doi: 10.1007/s00383-012-3222-3. |
| [15] | Zedek D., Fritchie K., Grenache D. The clinical utility of parathyroid hormone-related peptide in the assessment of hypercalcemia. Clin Chim Acta. 2009; 402 (2): 146-149. |
| [16] | Kollars J., Zarroug A.E., van Heerden J. et al. Primary hyperparathyroidism in pediatric patients. Pediatrics. 2005; 115(4): 1073. |
| [17] | Dowthwaite S.A., Young J.E., Pasternak J.D., Yoo J. Surgical Management of Primary Hyperparathyroidism. J. Clin. Densitom. 2013; 16(1): 48-53. |
| [18] | Mather HG. Hyperparathyroidism with normal serum calcium. BMJ. 1953; 2(4833): 424-425. doi: 10.1136/bmj.2.4833.424. |
| [19] | Kontogeorgos G, Trimpou P, Laine Cm, et al. Normocalcaemic, vitamin D-sufficient hyperparathyroidism — high prevalence and low morbidity in tht general population: a long-term follow-up study. The WHO Monica Project. Gothenburg, Sweden. Clin Endocrinol (Oxf). 2015; 83(2): 277-284. doi: 10.1111/cen.12819. |
| [20] | Ellika, S Preoperative localization of parathyroid adenomas using 4- dimensional computed tomography: a pictorial essay / S Ellika, S Patel, T Aho et al // Can Assoc Radiol J, 2013. – Aug. – № 64(3). – P 258-68. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML