Mukhamedova Malika Murtazayevna1, Ganieva Shakhzoda Shavkatovna2
1Basic Doctoral Student of the Bukhara State Medical Institute, Republic of Uzbekistan
2Associate Professor of the Department of Pediatrics of Bukhara State Medical Institute, Republic of Uzbekistan
Correspondence to: Mukhamedova Malika Murtazayevna, Basic Doctoral Student of the Bukhara State Medical Institute, Republic of Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The original article is devoted to the study of clinical features, the level of cytokines in acute coronary syndrome in people who have had a coronavirus infection and the development of a program for stratification of the risk of acute coronary syndrome and diagnostic immunological precursors of dangerous cardiovascular complications. Prevention of cardiovascular complications of postcovid syndrome is of great importance for health authorities when organizing rehabilitation measures in a pandemic. The proposed diagnostic method and program serve for the early diagnosis of acute coronary syndrome, which is of great practical importance.
Keywords:
Acute coronary syndrome, Cytokines, Immunity, Postcovid syndrome, Cardiovascular diseases
Cite this paper: Mukhamedova Malika Murtazayevna, Ganieva Shakhzoda Shavkatovna, Diagnostic Value of Immuno-Inflammatory Markers in Acute Coronary Syndrome, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 236-241. doi: 10.5923/j.ajmms.20231303.10.
1. Introduction
Coronavirus infection of 2019 (COVID-19) has a high risk of severe course in patients with concomitant pathology, including cardiovascular diseases (CVD), obesity, diabetes mellitus (DM), etc. An increased risk of acute coronary syndrome (ACS) was also previously noted after acute respiratory viral infections (ARVI) in patients with concomitant cardiovascular pathology [13]. Patients with ACS on the background of COVID-19 are more likely to have a more severe course in the acute period, after discharge from the hospital — the development of circulatory insufficiency and stent thrombosis. In the postcovid period, there is an increased risk of developing ACS [6-8]. Due to the prevalence and clinical significance, "postcovid syndrome" received the official status of the disease and was included in the new edition of the International Classification of Diseases of the 10th revision as "post-COVID-19 condition" with the code U09.9. [1]. Cytokines, which are mediators of immune inflammation, are locally produced by cells in atherosclerotic plaques. They coordinate intercellular interactions and modulate the functions of vascular wall cells. Evidence has been obtained that cytokines are markers of atherosclerotic risk and endothelial dysfunction. Therefore, the attention of researchers in recent years has been attracted by the study of cytokine status in cardiovascular diseases [3]. The pro-inflammatory properties of the CD40/CD40L system are due to the ability to increase the synthesis of cell adhesion molecules and various chemokines, enhance the expression of tissue factor, as well as matrix metalloproteases leading to instability of atherosclerotic plaque (AB). These results, together with the data on the high content of CD40L in the atherosclerotic plaque, confirm the concept that the interaction of CD40L with its receptor can contribute to the development of AB instability, causing acute thrombotic complications of atherosclerosis [11]. It is assumed that sCD40L is a potential indicator of the risk of developing CVD. Its level is increased in MI, heart failure, stroke [10]. The direct damaging effect of COVID-19 on the endothelium of the coronary arteries is established, leading to its dysfunction. Also, against the background of infection with SARS-CoV-2, the metabolic rate increases, therefore, the load on the CVD increases [2]. Today, the proteolysis system is searching for new fast and accurate diagnostic markers of ACS and its main forms — myocardial infarction and unstable angina [4].
2. The Purpose of the Research
To study the factors of cardiac remodeling and cytokine profile in patients with acute coronary syndrome who have had a coronavirus infection.
3. Materials and Methods
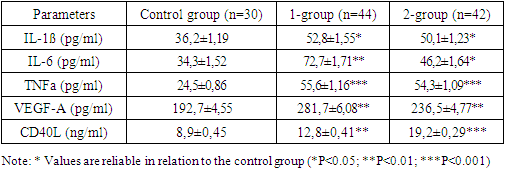
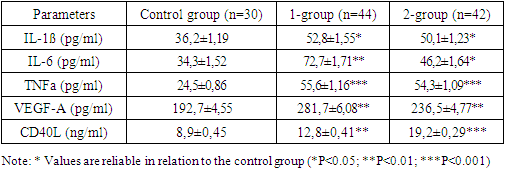
The study included 86 patients with ACS (ACS with transformation into acute myocardial infarction without ST segment elevation). Inclusion criteria were patients aged 46 to 65 years with a diagnosis of coronary artery disease, confirmed by coronary angiography, changes in the electrocardiogram and/or dynamics of cardiospecific enzymes, hospitalized for ACS. The distribution of groups of patients was carried out as follows: Control group, which included 30 people without cardiovascular pathology, practically healthy, group 1 - 44 patients with ACS who had previously suffered COVID-19 (with postcovid syndrome), group 2 - 42 patients with ACS without COVID-19 in the anamnesis. The patients of the study groups were comparable in age, gender, and the presence of CVD risk factors, such as hypertension, smoking, physical inactivity, dyslipidemia, and a history of myocardial infarction. Clinical manifestations of ACS were considered to be the presence of at least one of the following signs: the development of an anginal attack at rest and /or the duration of an anginal attack > 20 minutes and /or first-time angina pectoris of functional class II-III (FC) or progressive angina pectoris (the appearance of anginal attacks under loads within III-IV FC).The exclusion criteria from the study were patients with acute coronavirus infection (with a positive PCR test, and with the presence of IgM antibodies for ELISA), viral myocarditis, systemic diseases, oncological and hematological diseases. All patients were analyzed for the level of serum cytokines (IL-1β, IL-6, TNF-α) CD-40, VEGF-A – vascular endothelial growth factor in the hospital period of ACS, lipid profile (total cholesterol, low-density lipoproteins (LDL), high-density lipoproteins (HDL), triglycerides)), blood glucose level, coagulogram. PCR and ELISA (IgM and IgG) were performed for the presence of COVID-19, ECG, EchoCG, coronary angiography (CAG). The research was carried out in accordance with the Helsinki Declaration. Statistical processing of the results was carried out using Excel programs from the Microsoft Office XP application package (Microsoft, USA). The following results were obtained: the patients included in the study underwent COVID-19 on average 2-6 months before the development of ACS. The analysis of CVD risk factors among the admitted patients did not reveal gender differences in the two groups of patients. Comparison of anamnesis data revealed that in patients with ACS with postcovid syndrome, the development of the disease occurred at a younger age of 58.4 ±1.3 years in comparison with patients without postcovid syndrome 64.2±1.6 years, Three months after the diagnosis of COVID-19, changes in the cardiovascular system are present in 64% of patients with mild, 91% - moderate severity and 96% of patients with severe course of the infectious process (Fig.1).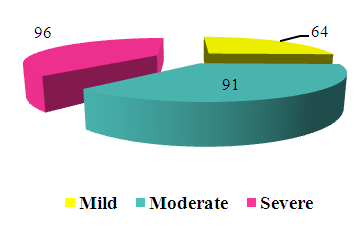 | Figure 1. The presence of symptoms of CCC pathology in patients who have had a coronavirus infection |
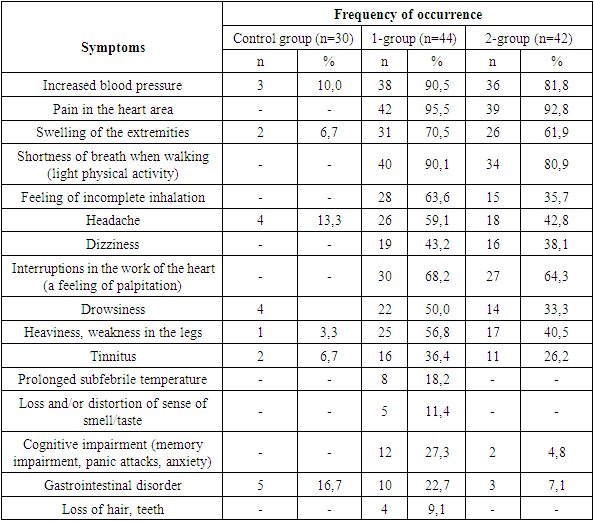
The symptoms presented by patients with acute coronary syndrome had a different frequency of occurrence depending on the presence of postcovid syndrome. In the group of patients with postcovid syndrome, symptoms such as swelling of the extremities, feeling of incomplete inhalation, headaches, heaviness and weakness in the legs, drowsiness and cognitive impairment significantly prevailed.When collecting anamnesis of patients with ACS who had a coronavirus infection, symptoms such as hair and teeth loss in 4 (9.1%), loss and/or distortion of taste were revealed/olfaction in 5 (11.4%) and prolonged subfebrile temperature in 8 (18.2%), which did not occur in the 2nd group of subjects without postcovid syndrome.It was found that the most common complication of coronavirus infection was the transformation of the form of coronary heart disease in 18 (40.9%), i.e. the transition of stable angina into unstable angina, an increase in the degree and stage of hypertension, the detection of chronic heart failure (CHF), as well as the progression of the stage of CHF. An increase in the degree of hypertension was diagnosed in 15 patients (34.1%). In 20 patients (45.5%), there was an excessive increase in blood pressure with the development of a hypertensive crisis. The increase in blood pressure ranged from 150/80 mmHg to 200/100 mmHg. In 8 patients (18.2%) in the long-term period (within 2-6 months after coronavirus infection), 2 or more hypertensive crises were recorded, which was regarded as their increase (Table 1). Table 1. Clinical characteristics of patients
 |
| |
|
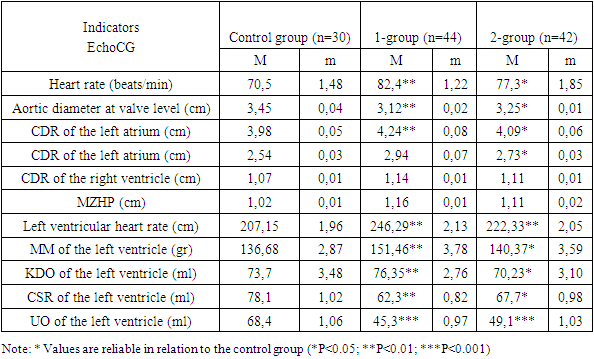
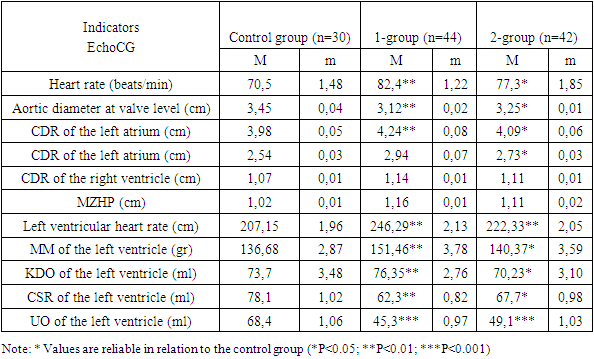
On the echocardiogram of ACS patients with postcovid syndrome, a slight aortic stenosis was observed at the valve level of 3.12±0.02 compared to healthy 3.45± 0.04 cm, in all ACS patients the muscle mass of the left ventricle was greater than in healthy patients and a significant decrease in the left ventricular ejection fraction was also observed regardless of the presence of postcovid syndrome 45.3± 0.97% and 49.1±1.03% versus 68.4±1.06% in the control group (Table 2).Table 2. Hemodynamic parameters of patients with ACS
 |
| |
|
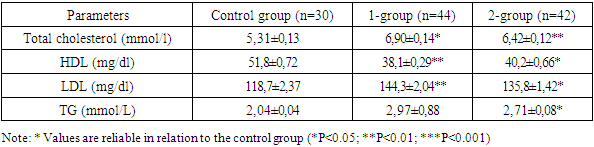
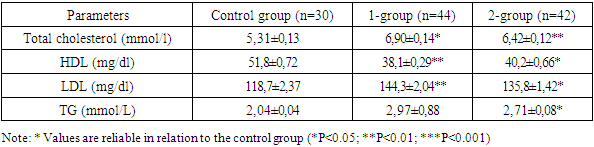
The study of the blood lipidogram in patients with ACS indicated an increase in total cholesterol to 6.90±0.14 mmol/l in ACS with postcovid syndrome and to 6.42±0.12 mmol/l in ACS without postcovid syndrome compared with the control group - 5.31±0.13 mmol/l. A significant decrease in the level of high-density lipoproteins (HDL) against the background of an increase in the concentration of low-density lipoproteins (LDL) in patients with ACS in both groups, they indicate a high coefficient of atherogenicity (Table 3).Table 3. Parameters of the lipid spectrum in acute coronary syndrome (M ±m)
 |
| |
|
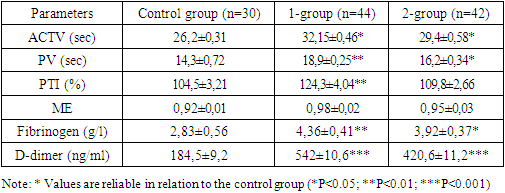
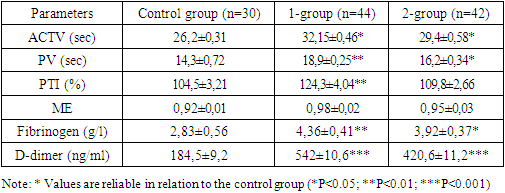
Coagulogram indicators of patients who had undergone coronavirus infection indicated the presence of hypercoagulation with a significant difference from the reference values. When comparing the parameters of ACS patients with postcovid syndrome, the concentration of D-dimer was 1.3 times higher than in group 2 and 3 times higher than in the control group. In patients with COVID 19, its significant increase is the result of hyperactive fibrinolysis associated with plasmin. In addition, an increased concentration of D-dimer may also indicate an excessive amount of intravascular polymerized fibrin. The proof of this pattern was a twofold increase in fibrinogen levels in the ACS group with postcovid syndrome 4.36±0.41 g/l (P<0.01), compared to healthy 2.83±0.56 g/l (Table 4).Table 4. Indicators of the blood coagulation system in acute coronary syndrome (M ± m)
 |
| |
|
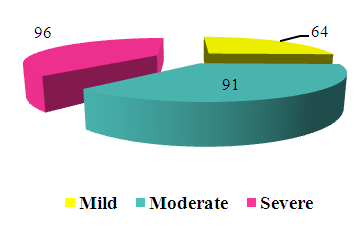
In patients with ACS, the risk of hospital mortality was calculated according to the GRACE scale (Global Registry of Acute Coronary Events) [9]. Low risk was determined with a score of <108, average — 109- 139 points, high — with ≥140 points.When calculating the risk of hospital mortality in ACS, the scores scored by patients varied depending on the presence of postcovid syndrome. A high risk in group 1 was observed in 17 (38.5%) patients compared with 11 (26.9%) in group 2, which was associated with high systolic blood pressure and increased heart rate in patients with coronavirus infection (Fig.2).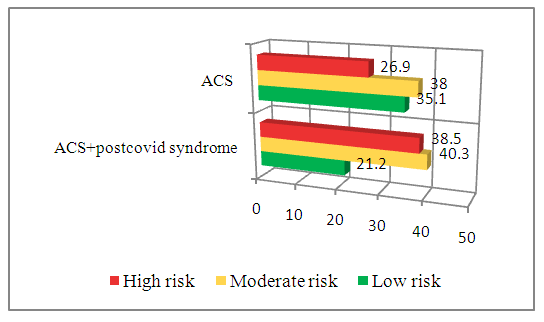 | Figure 2. Assessment of the risk of hospital mortality from myocardial infarction on the GRACE scale |
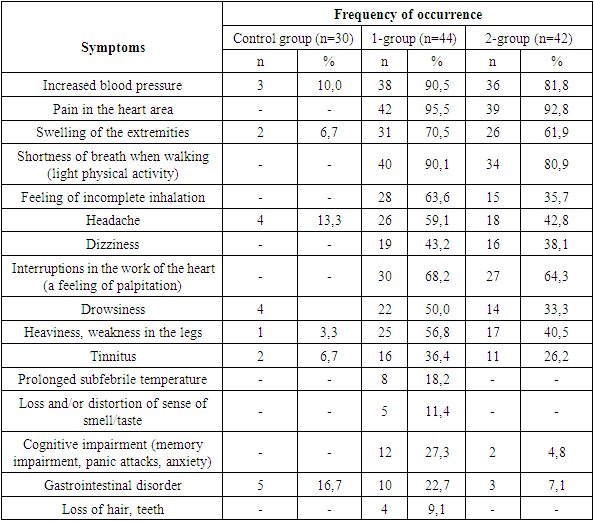
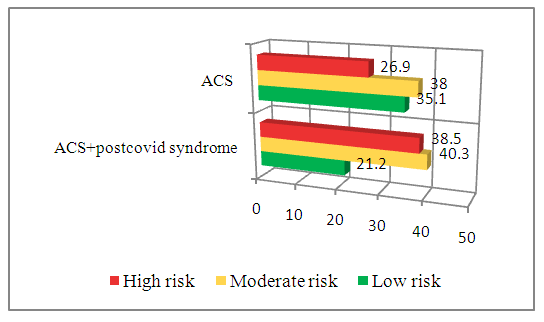
In order to assess the activity of the inflammatory process in ACS, cytokines (IL-1ß, IL-6, TNF-α) CD-40, VEGF, CRP, IgG to SARS COV2, as well as the correlation relationship of immunological parameters, lipodgrams and coagulograms were studied.Thus, high levels of serum IL-1ß and TNFa reflect a more pronounced systemic inflammatory response in the group of patients with ACS, however, the values of these cytokines were almost the same regardless of the presence of postcovid syndrome. In our study, the indicators of IL-1ß in group 1 (52.8±1.55 pg/ml) and in group 2 (50.1±1.23 pg/ml) were significantly 1.4 times higher than the control values (36.2±1.19 pg/ml), and TNFa in group 1 (55.6±1.16 pg/ml) and in group 2 (54.3±1.09 pg/ml), were 2.2 times higher than in healthy (24.5±0.86 pg/ml). This indicates the induction of an endogenous reaction aimed at the production of proinflammatory cytokines in response to ischemic myocardial damage in ACS. IL-6 and VEGF-A indicators were the most informative, as markers of ACS in patients who had undergone coronavirus infection, with significantly high values in the 1st main group. IL-6 in ACS with postcovid syndrome was (72.7±1.71pg/ml) 2 times higher than in the control group (34.3±1.52 pg/ml) and 1.6 times higher than in the ACS group without postcovid syndrome (46.2±1.64 pg/ml). The level of VEGF-A repeated trends similar to IL-6 and was significantly high in group 1 (281.7±6.08 pg/ml), which is 1.5 times higher than in the control group (192.7±4.55 pg/ml) (Table 5). Table 5. Indicators of serum cytokines in acute coronary syndrome (M ± m)
 |
| |
|
The increased concentration of this cytokine in the blood of ACS patients who have had a coronavirus infection indicates the process of post-ischemic neoangiogenesis and inflammatory infiltration of the endothelium of coronary vessels.Very ambiguous results were obtained with respect to the CD40L protein, which acts as a marker of atherosclerotic plaque instability. Antoniades C. It was proved with co-authors that CD40L level significantly increases with the development of unstable angina and myocardial infarction [5]. In our study, in the ACS group without postcovid syndrome, CD40L levels were 2 times higher (19.2±0.29 ng/ml) than in healthy individuals (8.9±0.45 ng/ml), however, in the group of those who had a coronavirus infection, they were increased only 1.4 times (12.8±0.41 ng/ml), compared with the control group, which indicates the need for a correlation analysis of immuno-inflammatory, thrombotic and biochemical factors in ACS (Table 5).During the correlation analysis of immunological and clinical laboratory parameters in patients with ACS and postcovid syndrome, the following informative results were obtained: CD40L protein had strong positive correlations with the GRACE scale (r=0.66), D-dimer (r=0.64) and fibrinogen (r=0.48) of blood serum, the average direct relationship it was observed with total cholesterol (r=0.34). The VEGF-A cytokine had strong positive correlations with the age of patients (r=0.42) and with the severity of coronavirus infection (r=0.41), an average negative association was observed with BMI (r=-0.32), and an average positive association with the GRACE scale (r=0.38), D-dimer (r=0.32) and fibrinogen (r=0.36).There was a strong negative relationship between the age of patients and IL-6 (r=-0.40), and strong positive correlations with the GRACE scale (r=0.44), total cholesterol (r=0.58) and triglycerides (r=0.54) of blood. IL-1ß was on average strongly positively correlated with the D-dimer (r=0.36), and TNFa had an average direct relationship only with the severity of coronavirus infection in patients (r=0.36).For comparison, in the group of patients with ACS without postcovid syndrome, CD40L protein strongly correlated with the GRACE scale (r=0.54), D-dimer (r=0.52), and total blood cholesterol (r=0.42). IL-6 had a strong positive relationship with the GRACE scale (r=0.44) and negative – with the age of patients (r=-0.38). The VEGF-A cytokine also strongly correlated directly with the age (r=0.51) of patients and negatively with BMI (r=-0.32), average positive associations were observed with fibrinogen (r=0.36), with the GRACE scale (r=0.38) and D-dimer (r=0.32). No reliable informative results were obtained for the remaining cytokines.Thus, in both groups of ACS, informative and diagnostically significant results of correlation analysis were obtained with respect to cytokines IL-6, CD40L and VEGF-A. The presence of strong direct links of CD40L with thrombosis factors D-dimer and fibrinogen in all patients with ACS indicates the prognostic value of this protein at the stages of IHD risk stratification. Our results are reflected in the studies of foreign authors (O. Pryshchep, W. MaKrupa, B.R. Younge et al. 2018), who proved that the interaction of CD40L with its receptor promotes the formation of platelet-neutrophil aggregates, which are one of the connecting links between the processes of inflammation and thrombosis [12]. Strong positive associations of the results of the GRACE scale with IL-6 and the severity of the coronavirus infection indicate the high informative value of this cytokine in patients with postcovid syndrome as a predictor of ACS. Significantly high concentrations of IL-6 in patients with postcovid syndrome indicate a high informative value of this cytokine in relation to coronavirus infection, rather than ACS, which requires the need for a comprehensive study of IL-6 with CD40L and VEGF-A for the diagnosis of coronary thrombosis, endothelial dysfunction and instability of atherosclerotic plaque. VEGF-A being a cytokine of neoangiogenesis processes directly correlated with the age of patients and the severity of the coronavirus infection.In patients with high BMI, IL-6 and IL-1ß cytokines were significantly elevated, the same cytokines positively correlated with total cholesterol and blood triglycerides. Taking into account the fact that BMI is an indirect manifestation of insulin resistance syndrome, we can think that hypercholesterolemia, insulin resistance and activation of nonspecific inflammation are links of the same process.
4. Conclusions
1. It was found that the most common complication of coronavirus infection was the transformation of the form of coronary artery disease in 40.9% of patients, i.e. the transition of stable angina into unstable angina, an increase in the degree and stage of hypertension, the detection of chronic heart failure with the progression of its stage. 2. A significant two-fold increase in the concentration of cytokines IL-6 and VEGF-A was found in patients who had a coronavirus infection, which indicates a higher process of post-ischemic neoangiogenesis and inflammatory infiltration of the endothelium of coronary vessels.3. Positive correlation of cytokines IL-6 and IL-1ß with BMI, total cholesterol and blood triglycerides was found in all patients with ACS. 4. The presence of strong positive correlations of CD40L protein with thrombosis factors D-dimer and serum fibrinogen in all patients with ACS has been proven, which justifies the prognostic value of this protein at the stages of IHD risk stratification before the development of ACS.
References
| [1] | Vaxnenko Yu.V., Dorovskix I.E., & Domke A.P. (2022). KARDIOVASKULYaRNAYa SOSTAVLYaYuShAYa POSTKOVIDNOGO SINDROMA. Tixookeanskiy medisinskiy jurnal, (1 (87)), 56-64. |
| [2] | Kravsiva Anastasiya Vladimirovna, Gulyaeva Alina Aleksandrovna, Golovanova Yelena Dmitrievna, & Ayrapetov Karen Viktorovich (2021). PORAJENIE SERDEChNO-SOSUDISTOY SISTEMI PRI COVID-19. Vestnik Smolenskoy gosudarstvennoy medisinskoy akademii, 20 (4), 59-65. |
| [3] | Prasolov A. V., Knyazeva L. A., Knyazeva L. I., Jukova L. A. Izmenenie pokazateley sitokinovogo statusa u bol'nix IBS: stabil'noy stenokardiey napryajeniya P-Sh funksional'nogo klassa v zavisimosti ot terapii // VNMT. 2009. №2. URL: https://cyberleninka.ru/article/n/izmenenie-pokazateley-tsitokinovogo-statusa-u-bolnyh-ibs-stabilnoy-stenokardiey-napryazheniya-p-sh-funktsionalnogo-klassa-v-zavisimosti. |
| [4] | Turna A.А. Diagnosticheskoe znachenie aktivnosti matriksnoy metalloproteinazi 9 (jelatinazi v) pri ostrom koronarnom sindrome // AG. 2010. №6. URL: https://cyberleninka.ru/article/n/diagnosticheskoe-znachenie-aktivnosti-matriksnoy-metalloproteinazy-9-zhelatinazy-v-pri-ostrom-koronarnom-sindromeAntoniades C., Tousoulis D., Vasiliadou C. et al. // J. Am. Coll. Cardiol. 2006. V. 47. Р. 1959–1966. |
| [5] | Azul Freitas A., Baptista R., Gonçalves V., Ferreira C., Milner J., Lourenço C. et al. Impact of SARS-CoV-2 pandemic on STelevation myocardial infarction admissions and outcomes in a Portuguese primary percutaneous coronary intervention center: Preliminary Data. Rev Port Cardiol (Engl Ed). 2021 Jul; 40(7): 465–471. DOI: 10.1016/j.repc.2020.10.012. |
| [6] | Choudry F.A., Hamshere S.M., Rathod K.S., Akhtar M.M., Archbold R.A., Guttmann O.P. et al. High Thrombus Burden in Patients With COVID-19 Presenting With ST-Segment Elevation Myocardial Infarction. J Am Coll Cardiol. 2020. Sep 8; 76(10): 1168–1176. doi: 10.1016/j.jacc.2020.07.022. |
| [7] | Hamadeh A., Aldujeli A., Briedis K., Tecson K.M., SanzSánchez J., Al Dujeili M. et al. Characteristics and Outcomes in Patients Presenting With COVID-19 and ST-Segment Elevation Myocardial Infarction. Am J Cardiol. 2020. Sep 15; 131: 1–6. DOI: 10.1016/j.amjcard.2020.06.063. |
| [8] | Hamm CW, Bassand JP, Agewall S, et al. Guidelines of the European Society of Cardiology for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal 2011; 32: 2999- 3054. |
| [9] | Plaikner M., Peer A., Falkensammer G. et al. // Clin. Chem. 2009. V. 55. Р. 175–178. |
| [10] | Velazquez E., Pfeffer M. // Circulation. 2004. V. 109. P. 440–442. |
| [11] | Vesselspecific tolllike receptor profiles in human medium and large arteries /O. Pryshchep, W. MaKrupa, B.R. Younge et al. // Circulation. – 2018. – V. 118. – P. 12761284. |
| [12] | Wadhera R.K., Shen C., Gondi S., Chen S., Kazi D.S., Yeh R.W. Cardiovascular Deaths During the COVID-19 Pandemic in the United States. J Am Coll Cardiol. 2021 Jan 19; 77(2): 159–169. DOI: 10.1016/j.jacc.2020.10.055. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML