Dauletova M. J., Babakhanova A. M., Yusupbaev R. B., Asatova M. M., Nishanova F. P., Rakhimbaev T. S.
Republican Specialized Scientific and Practical Medical Center for Obstetrics and Gynecology, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The disease is characterized by a severe course, a decrease in the quality of life and an increase in perinatal morbidity and mortality. According to the World Health Organization, the problem of reproductive health is in the center of attention of scientists around the world. During the observation of pregnant women with CAH, the following features were identified. Pregnant women with chronic hypertension regularly visited an obstetrician-gynecologist and an ultrasound diagnostics doctor, but the patients of the main group were significantly more frequent - on average, the frequency of visits was 14.2±0.3 times rather than those of the comparison group, 5.1±0.4 times (p<0.001). The purpose of the study. To optimize obstetric management tactics of pregnant women with chronic arterial hypertension, depending on the condition of fetal shunts.
Keywords:
Dopplerometry, Fetoplacental, Cardiotocographic, Obstetrician-gynecologist, Ultrasound diagnostics
Cite this paper: Dauletova M. J., Babakhanova A. M., Yusupbaev R. B., Asatova M. M., Nishanova F. P., Rakhimbaev T. S., Management Tactics of Pregnant Women with Chronic Arterial Hypertension Complicated by Severe Uterine-Fetal-Placental Disorders, American Journal of Medicine and Medical Sciences, Vol. 13 No. 3, 2023, pp. 197-202. doi: 10.5923/j.ajmms.20231303.01.
1. Introduction
Fetoplacental insufficiency in presence of arterial hypertension (AH) is the most common disease complicating the course of pregnancy, as well as one of the most pressing problems of medical science and practice [1,2,5,9,11]. In recentyears, pregnancy-related complications, including hypertensivedisorders, have increased in all economically developed countries, which is reflected in the latest publications [2,4,5,8].Fetoplacental insufficiency and fetal growth restriction syndrome (FGR) in presence of hypertensive disorders is complicated in 20% of cases of pregnancy and ranks 2-3 in the structure of perinatal morbidity and mortality [3,4].According to the report of experts from the World Health Organization, the frequency of hypertension and, accordingly, FGR among pregnant women has increased by more than 40% over the past two decades of observation [6,7,10,11]. Elevated blood pressure (BP) during pregnancy is strongly associated with a high rate of preterm birth, chronic and acute placental insufficiency, various perinatal complications such as FGR, and fetal death [12]. In this regard, it is important to raise the level of quality of medical services provided to a new level, and to develop new approaches to prognosising and prolonging pregnancy in women with chronic arterial hypertension (CAH), complicated by severe blood circulation in the mother-placenta-fetus system.
2. Materials and Methods of the Research
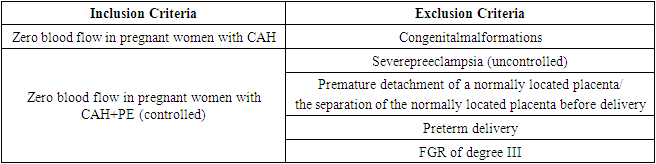
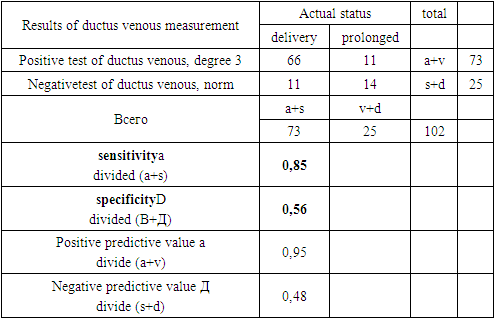
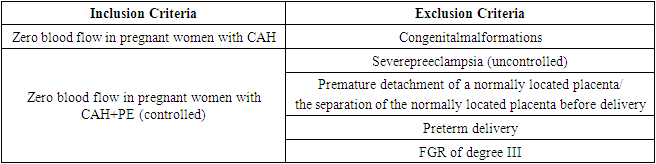
We studied 120 pregnant women with chronic arterial hypertension (CAH) with impaired uteroplacental-fetal blood flow (IUPFBF) of degree 3. 120 pregnant women with CAH were divided into 2 groups:Group I consisted of n=73 pregnant women with zero blood flow in the umbilical artery with CAH (main group) whose pregnancy was prolonged;Group II included n=47 pregnant women with zero blood flow, and CAH who gave childbirth without pregnancy prolongation (comparison group).Pregnant women of the main group regularly visited an obstetrician-gynecologist, who carried out dynamic control of Doppler parameters and, depending on their parameters, prolonged pregnancy.The selection of patients for the study was carried out according to the inclusion/exclusion criteria (Table 1).Table 1. Criteria for selecting patients for the study
 |
| |
|
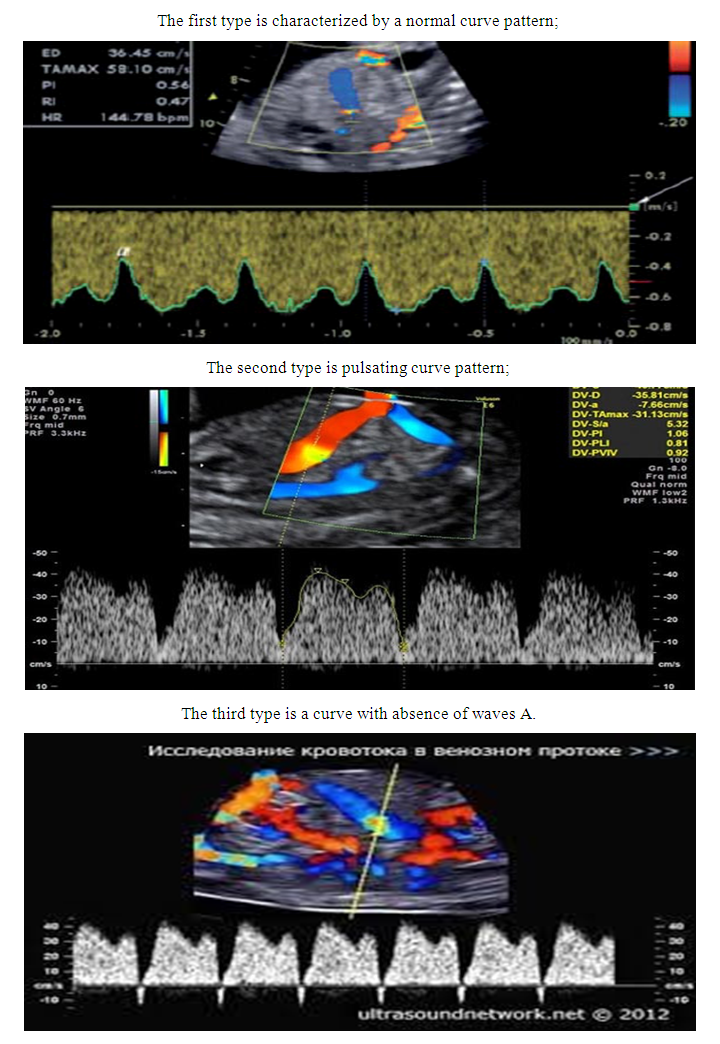
The diagnosis of CAH and CAH + PE was made on the basis of the internal protocol of the Republican Specialized Scientific and Practical Medical Center for Obstetrics and Gynecology.The most significantprognostic indicators for prolongation of pregnancy were determined with the help of Dopplerometry. Also, pregnant women with CAH and after 30 weeksof gestation underwent periodic cardiotocographic monitoring of the fetus. The study of uterine-fetal-placental circulation was carried out by the method of Dopplerography with color mapping and Dopplerometry on the device "Mindray DC-70". The blood flow in the umbilical artery was studied: it is a systemic indicator of fetal hemodynamics and the properties of the vascular bed of the placenta (sclerosis, thrombosis). Reverse or zero blood flow in diastole, a notch on the curve at the end of systole are indications for immediate obstetric intervention, since such changes are often followed by fetal death.The blood flow in the ductus venous was studied. There are 3 types of venous blood flow curves (Figure 1).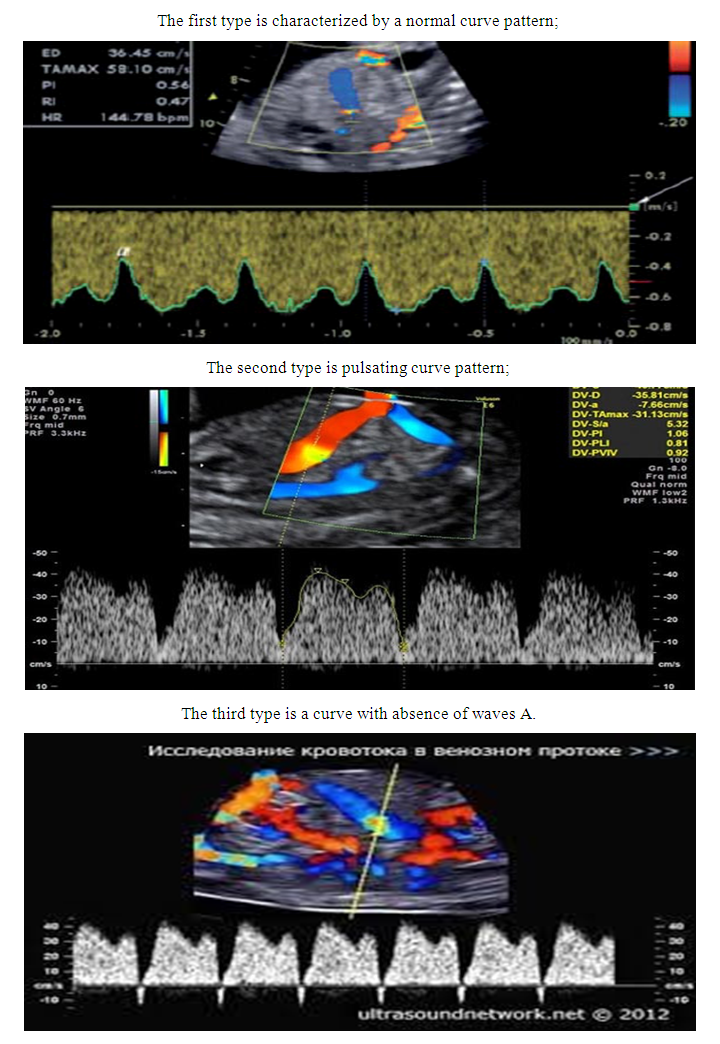 | Figure 1 |
3. Results and Discussions
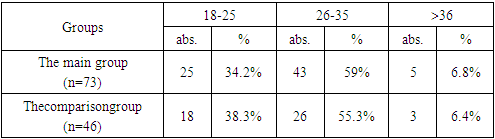
During the observation of pregnant women with CAH, the following features were identified. Pregnant women with chronic hypertension regularly visited an obstetrician-gynecologist and an ultrasound diagnostics doctor, but the patients of the main group were significantly more frequent - on average, the frequency of visits was 14.2±0.3 times rather than those of the comparison group, 5.1±0.4 times (p<0.001). This is due to the fact that, with the connection of the progression of circulatory disorders of UPFBF, the patients more often went to the Doppler ultrasound of the fetus, and the women in the comparison group were immediately hospitalized and delivered prematurely, as soon as IUPFBFof degree 3was detected (zero blood flow). All patients of the main group were taken under observation at 25-28 weeks of gestation and were observed in dynamics until delivery, respectively, pregnant women at 25-28 weeks or more were also included in the comparison group.The age of the examined pregnant women ranged from 21 to 38 years and in the main group averaged 27.4 ± 1.26 years, which did not significantly differ from 26 ± 2.54 years in women of the comparison group (* - hereafter in the text the difference is not significant at p>0.05), (table 2).Table 2. Characteristics of the age groups of pregnant women (in absolute numbers and%)
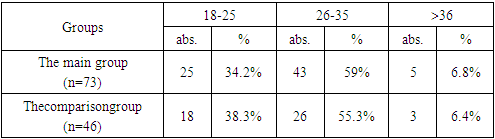 |
| |
|
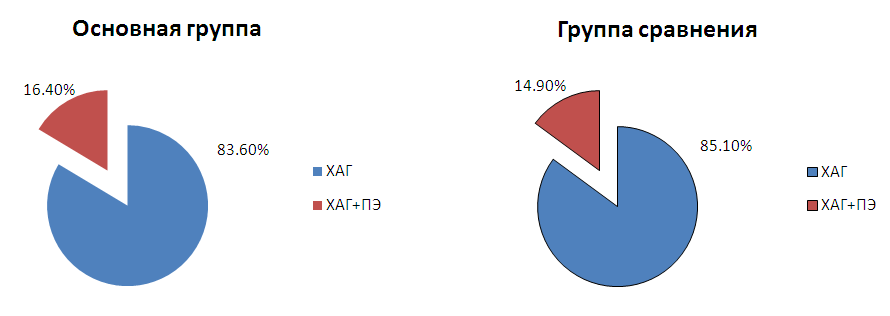
In both groups, in pregnant women with CAH, the addition of PE was detected in the third trimester of pregnancy. These indicators did not differ significantly, in the main group PE joined in 16.4% of cases and in the comparison group in 14.9% of cases, respectively (Figure 2).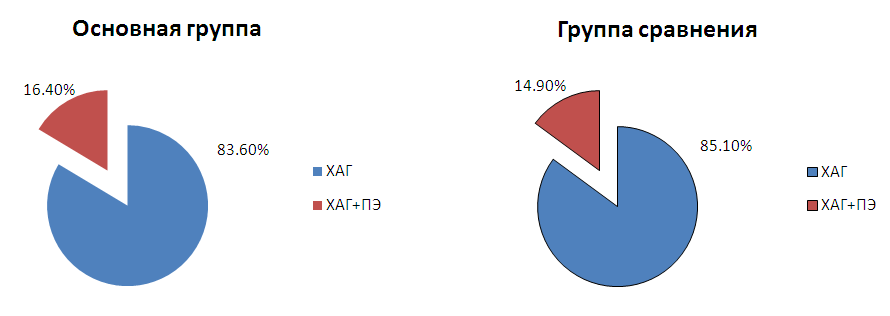 | Figure 2. Frequency of occurrence of PE in pregnant women with CAH in both groups |
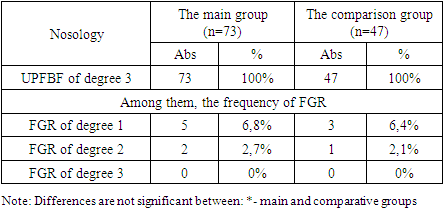
In the analysis of patients in the observation group during predelivery hospitalization, a high frequency of IUPFBF was revealed already at the ambulatory stage. Disorders of UPFBFof degree 3 were recorded in all examined pregnant women, which was an indication for hospitalization.In the prospective study in both groups, pregnancy was complicated by disorders of UPFBF (table 3). Fetal growth restriction syndrome (FGR) is one of the signs of intrauterine fetal distress, which is the main manifestation of IUPFBF in presence of hypertensive disorders.Table 3. Doppler indicators for IUPFBF in the II and III trimester of pregnancy
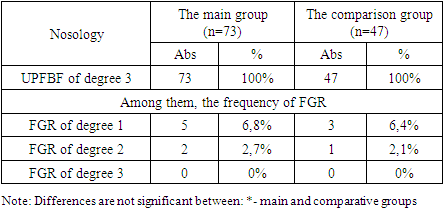 |
| |
|
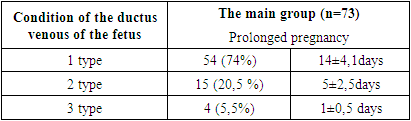
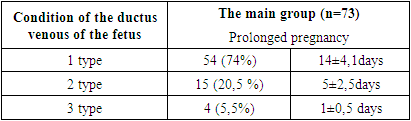
Dopplerometry of the umbilical artery showed the results of zero blood flow. In our observations, FGR of degree 1 and FGR of degree 2were detected in 6.4%, 2.1% of women respectivelyin the comparison group and in the main group, 6.8% and 2.7% of women respectively. (p<0.001).The study of the ductus venouspresented some visualization difficulties, which were an indication for re-examination after a certain time. A typical ductus venous blood flow wave consisted of three phases: the first peak is the pressure gradient between the veins and the right atrium during ventricular systole; the second peak is associated with valve opening and early passive ventricular filling; the decrease in flow velocity coincides with the third phase - atrial contraction at the end of diastole. With the development of fetal congestive heart failure and deterioration of myocardial contractility, resistance in the right atrium increased in 33% of cases. We distinguished 3 types of curves of venous blood flow, which are described in table 4.Table 4. Condition of the ductus venous in the study groups
 |
| |
|
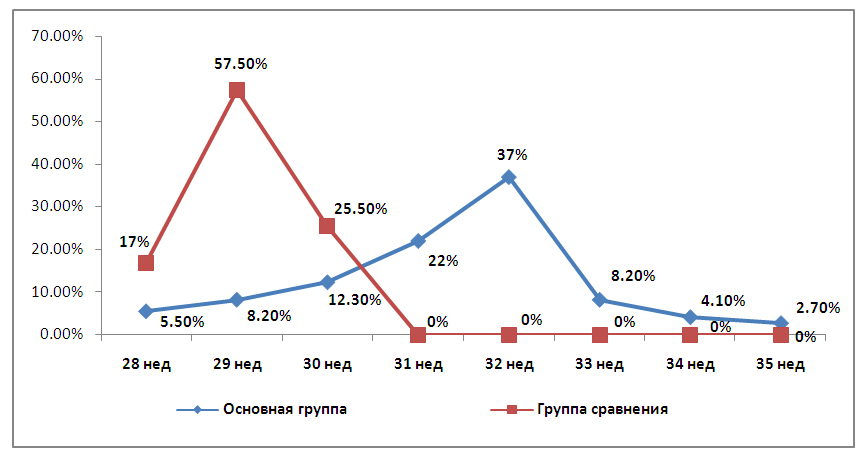
Thus, during the study, 3 types of ductus venous disorders were described in pregnant women with chronic arterial hypertension and preeclampsia:During the initial examination, type 1 of ductus venous curve was detected in 54 (74%) women, this is the norm without changes in the visual graph of the normative indicators of the pulsation index (PI) and resistance index (IR) according to the gestational age within the 95th percentile for this period PI=0.21- 1.35, IR 0.50-0.70., the dynamic Doppler study of UPFBF and ductus venous was performed every 7 days in these women, after changing to type 2 of ductus venous curve, the study was performed every 3 days. In our study, in the patient with type 1 of circulatory disorder, pregnancy was extended from 14±4.1 days.The 2nd type of ductus venous curve was revealed in 15 women (20.5%). This is with a change in the visual graph of the spectrogram with an increase in pulsation and pathological indicators (PI, IR) above the 95th percentile for a given gestational age, these women underwent the Doppler study of the UPFBF every 3 days and assessed the blood flow in the ductus venous. In our study with type 2 of circulatory disorders, pregnancy was extended from 5±2.5 days.During the initial examination in 4 women (5.5%), type 3 of the EP curve was revealed, and therefore all of them gave childbirth within 24 hours. Type 3 of the curve is severe pathological changes in the spectrogram - reverse or zero diastolic blood flow of the pulse wave and pathological pulsation index above 95 percentile for a given gestational age.Changes in ductus venous of type 3 were the basis for early delivery in the main group, in the comparison group these indicators were not measured for various reasons (poor visualization, technical difficulties, lack of personnel who master methods for measuring ductus venous), including women's refusal to offer prolongation of pregnancy. Thus, we took these changes in venous blood flow as a control marker identified by Doppler. Critical indicators of blood flow in the umbilical cord that occur due to the stop in the translational movement of blood in the diastole phase (zero values) or a change in the movement of blood flow to the opposite (retrograde blood flow) were an indication for emergency delivery in the comparison group. In turn, the use of an assessment of blood flow in ductus venousmade it possible to prolong pregnancy up to 35 weeks in 2.7% of women in the main group (Figure 3).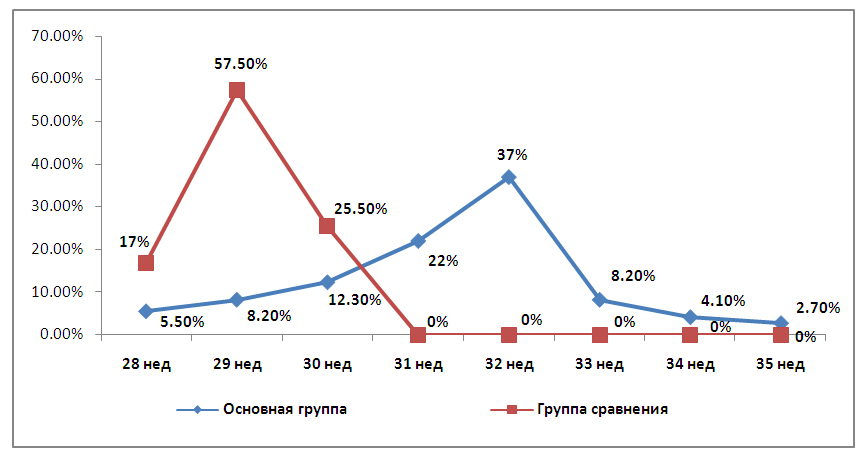 | Figure 3. Terms of delivery in examined women with CAH and PE with zero blood flow |
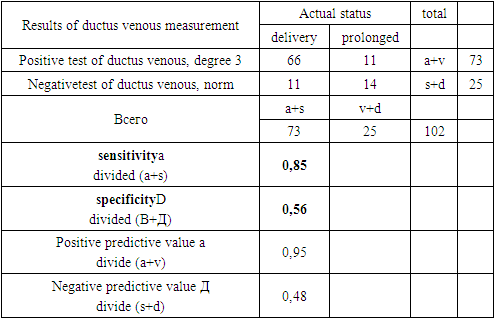
The diagram shows that at 28 weeks of gestation in the main group childbirth was delivered (5.5%), the largest number of deliveries took place at 31, 32 and 33 weeks of gestation, in the comparison group 22%, 37% and 8.2% of casesrespectively. At 34 weeks of gestation, 3 women (4.1%) gave childbirth. According to fetal dopplerometry, it was possible to prolong pregnancy up to 35 weeks only in 2.7% of cases, respectively, this significantly increases the chance of survival of newborns.The condition of the ductus venous had the appearance of types 1 and 2, which served as one of the indicators for the prolongation of pregnancy in the main study group, which is consistent with the literature data. Thus, the sensitivity (85%) and specificity (56%) of the ductus venous test to confirm fetal hypoxia affecting pregnancy outcome was confirmed by our study data (Table 5).Table 5. A four-dimensional contingency table for calculating the specificity and sensitivity parameters for the ductus venous in this method
 |
| |
|
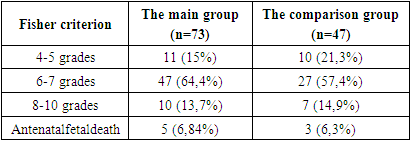
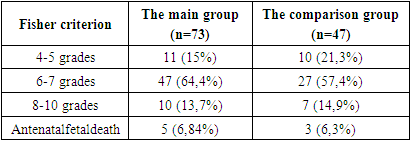
To identify the functional state of the fetus, a study was carried out in both groups by the method of cardiotocography with the determination of the Fisher index and the evaluation of the cardiotocogram graph. The data obtained indicate that in both groups there was a disorder of the state of the fetus requiring CTG monitoring in dynamics (Table 6). The results of CTG were considered strictly individually only in combination with clinical data, as well as with the results of other studies, such as Doppler utero-fetal complex. The above conditions were observed in the first group and in the second group, and this was a marker for daily monitoring and for early delivery due to the lack of improvement in dynamics.Table 6. Estimation of the Fisher criterion
 |
| |
|
As can be seen from Table 6, the indicators of the Fisher criterion are different in both groups. If the Fisher criterion was below 5 points, CTG was performed daily, deterioration in dynamics was detected on average in 89% of patients within 3 days, which suggests that the observation interval can be extended to 3 days without additional research.An analysis of the outcomes of childbirth for the fetus showed that in pregnant women of the main group, 64.4% of children were born with an Apgar score of 6-7 points, 13.3% of cases with a score of 8-10 points and 6.8% of cases with a score of 4-5 points, while in the comparison group, 14.9% of women had an Apgar score of 8-10 points, 57.4% of women had 6-7 points and 21.3% of women had 4-5 points. Also in the groups of women, antenatal fetal death occurred in the main group in 6.84% of cases and in the comparison group in 6.3% of cases, which was statistically unreliable. The results of CTG were considered strictly individually only in combination with clinical data, as well as with the results of other studies, such as Doppler utero-fetal complex.Indications for early delivery in the first group were set in the first 3 days in 28 pregnant women, during the next 2 days in 14 pregnant women, the indications were mainly the progression of hypertensive conditions in (28.5%), the progression of IUPFBF in (21.3%) and the unconvincing state of the fetus in (18.9%) cases, as well as other obstetric indications that did not depend on hypertensive conditions.
4. Conclusions
Thus, 3 types of ductus venous disorders in pregnant women with chronic arterial hypertension are described:Type 1 norm - without changes in the visual graph of the normative indicators of the pulsation index (PI) and resistance index (IR) according to the gestational age within the 95th percentile for this period PI=0.21- 1.35, IR 0.50-0.70. In our study, in the patient with type 1 of circulatory disorder, pregnancy was extended from 14±4.1 days in 54 pregnant women (74%).Type 2. With a change in the visual graph of the spectrogram with an increase in pulsation and pathological indicators (PI, IR) above the 95th percentile for a given gestational age. In our study with type 2 of circulatory disorders, pregnancy was extended from 5±2.5 days in 15 women (20.5%).Type 3 - severe pathological changes in the spectrogram - reverse or zero diastolic blood flow of the pulse wave and pathological pulsation index above 95 percentile for a given gestational age. In our study, with 3 types of circulatory disorders, pregnancy was prolonged by no more than 1 day in women 14 (5.5%).- Studies have shown that the reduction of the Fisher criterion to 5 points with the appearance of pathological abnormalities of cardiotocography has a sensitivity of 84% and a specificity of 49% for early delivery in CAH.- The study of blood flow in the ductus venous of the fetus made it possible to assess the hemodynamics of the fetus in CAH with a sensitivity of 85% and a specificity of 56%, which allows controlling the reserve capacity of the fetus and timely diagnosing threats to fetal conditions.
References
| [1] | ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. AmericanCollege of Obstetricians and Gynecologists. Obstet Gynecol. 2009 Jul; 114(1): 192-202. |
| [2] | Adam K. Lewkowitz, Methodius G. Tuuli, Alison G. Cahill. Perinatal outcomes after intrauterine growth restriction and intermittently elevated umbilical artery Doppler // American Journal of Obstetrics & Gynecology MFM. — March 2019. |
| [3] | World health statistics 2017: monitoring health for the SDGs, Sustainable Development Goals. |
| [4] | Alfirevic Z, Devane D, Gyte GM. Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour. Cochrane Database Syst Rev. 2013 May 31; 5: CD006066. |
| [5] | Amanda S. Trudell, Alisson G. Cahill, Methodius G. Tuuli. Risk of stillberth after 37 weeks in pregnancies complicated by small-for-gestational-age fetuses // American Journal of Obstetrics & Gynecology. — 2013. — №208. — P. 3763. |
| [6] | Ayres-de-Campos D1, BernardesJ; FIGO Subcommittee. Twenty-five years after the FIGO guidelines for the use of fetal monitoring: time for a simplified approach? Int J Gynaecol Obstet. 2010 Jul; 110(1): 1-6. |
| [7] | Barker D.J. The origins of the developmental origins theory // Journal of International Medicine. — 2007. — №261. — P. 412-417. |
| [8] | Baschat A.A. Neurodevelopment after fetal growth restriction // Fetal Diagnosis and Therapy. — 2014. — №36. — P. 136-142. |
| [9] | Basky Thilaganathan. The ASPRE pre-eclampsia trial: implications for basic research and clinical practice // Cardiovascular Research. — 2018. — №114. — P. 60-61. |
| [10] | Benavides-Serralde A., Scheier M., Cruz-Martinez R., et al. Changes in central and peripheral circulation in intrauterine growth-restricted fetuses at different stages of umbilical artery flow deterioration: new fetal cardiac and brain parameters // Gynecologic and Obstetric Investigation. - 2011. - №71. - P. 274-280. |
| [11] | Ganzevoort W., Mensing Van Charante N., Thilaganathan B., et al., for the TRUFFLE Group. How to monitor pregnancies complicated by fetal growth restriction and delivery before 32 weeks: post-hoc analysis of TRUFFLE study // Ultrasound in Obstetrics and Gynecology. — 2017. — №49. — P. 769-777. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML