-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 186-190
doi:10.5923/j.ajmms.20231302.33
Received: Feb. 6, 2023; Accepted: Feb. 22, 2023; Published: Feb. 28, 2023

Cumulative Effectiveness of Vitiligo Treatment Depending on the Stage of Clinical Course
U. Yu. Sabirov, A. Sh. Inoyatov, Zh. Sh. Narziev, I. A. Samarkhodzhaeva
Republican Specialized Scientific and Practical Medical Center of Dermatovenerology and Cosmetology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Vitiligo diagnosis and treatment are difficult. The advancement of vitiligo diagnostic procedures highlights the need to determine the severity of the disease, the extent of its progression, and the quality of life, all of which influence the volume of therapeutic measures. According to the World Health Organization, the number of patients with vitiligo in the world is approximately 0,8-2,8% of the total population of the Earth; in recent years, there has been a tendency to increase the number of patients with vitiligo, and the frequency of this disease reaches 10% in various ethnic groups and populations. A large number of papers have been devoted to vitiligo research on a global scale, but the wide variety of methods of treating this pathology indicates a lack of a unified approach, which, in turn, indicates an unresolved pathogenesis of depigmentation in vitiligo.The study included 287 patients with non-segmental vitiligo, with an average age of 28,1±1,3 years and a disease duration of 42,6±3,6 months. All patients were examined and treated at the State Institution RSNPMTSDVIK between 2018 and 2022.In general, 161 (56,1%) of 287 patients received excellent results, 71 (24,7%) received good results, 42 (14,6%) received satisfactory results, 9 (3,1%) received unsatisfactory results, and 4 (1,4%) received progression.Excellent results were significantly more common with stable vitiligo - in 65% vs. 43% of cases (p0,05); good results were equally common - in 27% of cases, satisfactory - more common with unstable vitiligo - in 26% vs. 7% (p0,05).
Keywords: Vitiligo, NB-UVB therapy, Provitilin, Vitiligo treatment, Fr: CO2 laser10600 nm, YAG: Er laser 2940 nm
Cite this paper: U. Yu. Sabirov, A. Sh. Inoyatov, Zh. Sh. Narziev, I. A. Samarkhodzhaeva, Cumulative Effectiveness of Vitiligo Treatment Depending on the Stage of Clinical Course, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 186-190. doi: 10.5923/j.ajmms.20231302.33.
1. Introduction
- Diagnosis and treatment of vitiligo present significant difficulties [1]. The improvement of diagnostic procedures for vitiligo indicates the need to determine the severity of the disease, the degree of its progression and the quality of life, on which the volume of therapeutic measures depends [2]. According to WHO, "the number of patients with vitiligo in the world is approximately 0,8−2,8% of the total population of the Earth; in recent years there has been a tendency to increase the number of patients with vitiligo, and in various ethnic groups and populations the frequency of this disease reaches 10% ..." [8]. In 2011, an initiative was launched to proclaim June 25 as World Vitiligo Day to include it in the UN calendar. Well-known entrepreneur Steve Hargadon organized a private social network Vitiligo Friends.org and the project “Uniquely beautiful”, which is a powerful support for the social adaptation of people with vitiligo. All this once again proves the difficulties of treating vitiligo [7]. A large number of papers have been devoted to vitiligo research on a global scale, but the wide variety of methods of treating this pathology indicates the lack of a unified approach, which, in turn, indicates the pathogenesis of depigmentation in vitiligo that has not been fully disclosed [3,4].
2. Materials and Methods
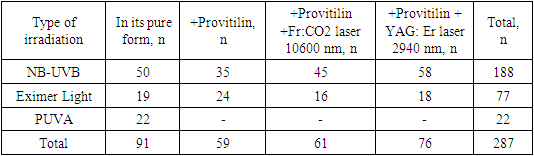
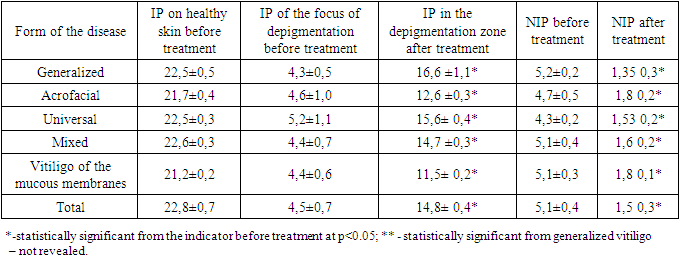
- 287 patients with non-segmental vitiligo were examined, average age = 28,1±1,3 years, disease duration – 42,6±3,6 months. All patients were examined and received treatment in the State Institution "RSNPMTSDVIK" in the period from 2018 to 2022. The ratio of men and women was 1,08, which shows an equal incidence of vitiligo in men and women. At the same time, 78,4% were persons under the age of 45. In our observations, Fitzpatrick skin types III and VI prevailed in persons with vitiligo: 51% and 38%, respectively, there were no persons with type V and VI. The degree of progression of the disease was determined by the presence of the following signs: 1) fuzzy borders of foci or the appearance of new point depigmented areas, 2) the Kebner phenomenon, 3) "trichromic" staining in foci, 4) signs of inflammation, hyperemia and itching in foci [4]. The severity of the disease (prevalence, degree of depigmentation + quality of life) was assessed according to our proposed M-VES scale. In the M-VES scale, we propose to summarize the scores on 2 scales: VES [4] and DIKJ for a full assessment of the severity of vitiligo. Methods of treatment included UFO and laser therapy. PUVA, NB-UVB phototherapy was performed on the NEOLUX Series 3 installation (“Daavlin” USA), in the mode 3-5 times a week. Excimer light treatment was carried out on an Excilite µ 308nm unit (DEKA, Italy). Laser irradiation was carried out by two types of lasers. A fractional Fr:CO2 laser with a wavelength of 10,600 nm was used, irradiation was carried out on a SmartXide installation with Punto technology (DEKA, Italy) in a fractional mode of 10W, 800 ms, 10600 nm. An erbium laser was also used. Laser irradiation with YAG:Er erbium laser was carried out at the Harmony XL Pro installation (Alma Lasers, Israel), in ablation mode, with a 9*9 mm nozzle, at a wavelength of 2940 nm, 1800 J/cm2. Provitilin cream was used locally. The distribution of patients depending on the type of treatment is presented in the table (Table 1).
|
|
3. Results and Discussion
- Unstable vitiligo was detected in 122 (42.5%) patients. The activity of the process (unstable course) was characterized by the presence of all 3 signs: "scalloped" vitiligo, tricolor vitiligo, the presence of the Kebner phenomenon in 85 (29.6%) patients, an increase in the area of existing foci and the appearance of new ones during the last 3 months was in 33 (11.5%) patients, in 4 (1.4%) cases there was the process of inflammation in the foci was revealed. Stable vitiligo – in 165 (57.5%). In our studies, NB-UVB therapy was given to patients with an initially severe course, progressive-unstable vitiligo. Thus, 37 out of 103 patients who received NB-UVB in combination with lasers had progressive vitiligo, which in the first 4-6 months was treated only with narrow-band UVB, and subsequently, laser therapy was connected. When analyzing the results of treatment in patients with stable vitiligo in the general subgroup of combined treatment with NB-UVB+lasers+Provitilin showed mostly good and excellent results. Thus, out of 67 patients with excellent results, 49 (73.1%) had stable vitiligo, 18 (26.9%) had unstable vitiligo. Of the 18 patients with a good result, 15 (83%) had stable vitiligo, 3 (17%) had unstable vitiligo at the beginning of treatment. In the general subgroup NB-UVB+lasers+Provitilin out of 37 patients with unstable vitiligo, only 17 (45.9%) had an excellent result, 3 (8.1%) had a good result, 14 (37.8%) had a satisfactory result, and 3 (8.1%) had an unsatisfactory result. Out of 66 patients with stable vitiligo, 49 (74%) had an excellent result, 15 (22.7%) had a good result, and only 2 (3%) patients had a satisfactory result.In general, out of 287 patients, 161 (56.1%) had excellent results, 71 (24.7%) had good results, 42 (14.6%) had satisfactory results, 9 (3.1%) had unsatisfactory results, and 4 (1.4%) had progression (Table 3).
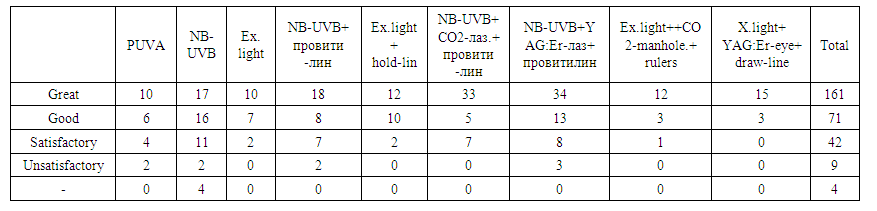 | Table 3. Distribution of patients depending on the result of treatment |
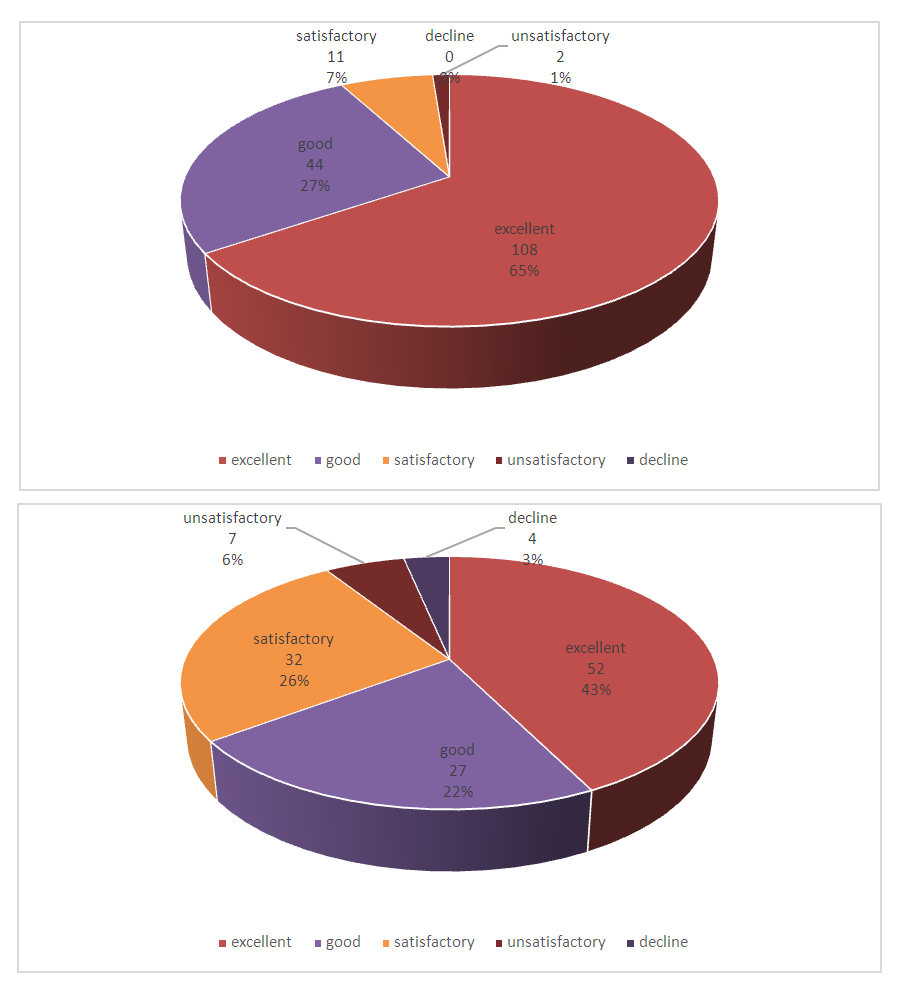 | Figure 1. Results of treatment of stable and unstable vitiligo |
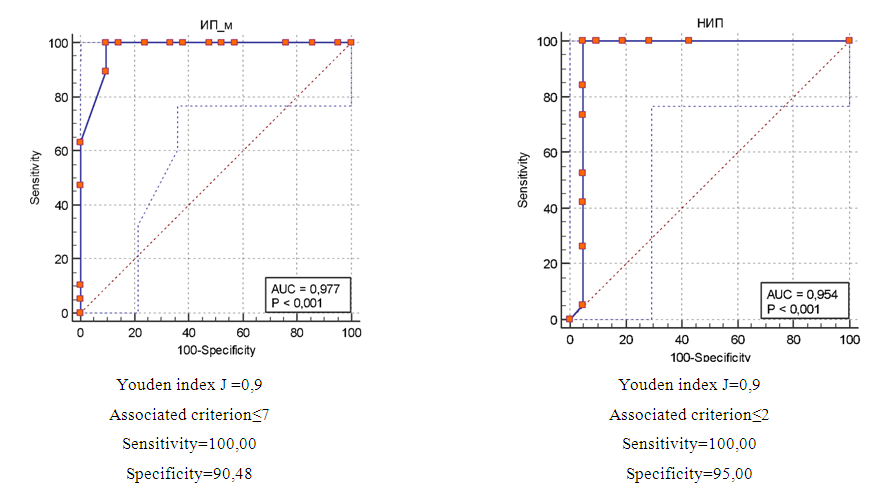 | Figure 2. ROC curve for the diagnostic efficiency of IP and IM according to the data of mex |
|
4. Conclusions
- 1. Excellent results were significantly more common with stable vitiligo - in 65% vs. 43% of cases, respectively (p<0.05); good results were equally common – in 27% of cases, satisfactory – more common with unstable vitiligo - 26% vs. 7% (p<0.05).2. Mex is an objective way to assess the reserve depigmentation in vitiligo, because the specificity of the normalized pigmentation index of NIP and IP was 95% and 90.5%, respectively. 3. The cut-off thresholds for the prediction of a good and excellent repigmentation result were for IP> 7 for IP with 100% sensitivity and 90% specificity; for NIP>2 with 100% sensitivity and 95% specificity.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML