-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 170-175
doi:10.5923/j.ajmms.20231302.30
Received: Feb. 10, 2023; Accepted: Feb. 23, 2023; Published: Feb. 28, 2023

Diagnosis, Management and Outcomes of Non-Immune Hydrops Fetalis in Uzbekistan
Pulatova G. A., Yusupbaev R. B.
Republican Specialized Scientific-Practical Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan
Correspondence to: Pulatova G. A., Republican Specialized Scientific-Practical Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article presents the results of a survey of 51 pregnant women with non-immune hydrops fetalis. Of these, 9 pregnancies were terminated due to the high risk of chromosomal abnormalities in early pregnancy, and these pregnant women were excluded from further stages of the study. Pregnancy in 20 pregnant women was carried out on the basis of a diagnostic and management algorithm developed for non-immune hydrops fetalis. The remaining 22 pregnant women refused active management of pregnancy with non-immune hydrops fetalis and were carried out on the basis of expectant management. The outcomes of pregnancy in 2 groups were discussed. The etiological factors that led to this disease, the methods of their detection, the results of etiological and symptomatic treatment, the principles of pregnancy management in non-immune hydrops fetalis are analyzed. Data on intrauterine interventions and their results in examined patients with non-immune hydrops fetalis are presented.
Keywords: Non-immune hydrops fetalis, Paracentesis, Thoracocentesis, Amnioreduction, Immunoglobulin therapy, Fetal arrhythmias
Cite this paper: Pulatova G. A., Yusupbaev R. B., Diagnosis, Management and Outcomes of Non-Immune Hydrops Fetalis in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 170-175. doi: 10.5923/j.ajmms.20231302.30.
Article Outline
1. Relevance
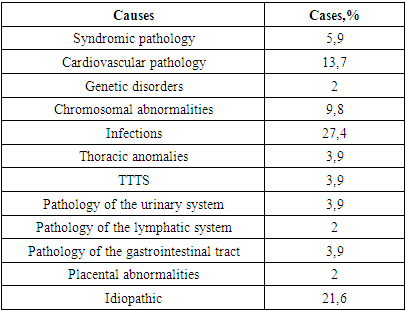
- Despite many advances in fetal medicine, non-immune hydrops fetalis still remains one of the most pressing problems nowadays and plays a significant role in the structure of perinatal morbidity and mortality. Among all cases of hydrops fetalis, non-immune hydrops account for approximately 90% [3,15]. Its frequency, according to large-scale studies, ranges from 1:2000-1:3000 pregnancies [3,12]. Non-immune hydrops fetalis is the final stage for a number of intrauterine diseases and its treatment, of course, requires highly specialized high-tech minimally invasive intrauterine interventions which used in modern fetal medicine. The survival rate of newborns with this pathology is 27-36%, only with the use of high-tech methods of fetal medicine in the antenatal period and intensive care of newborns in the neonatal period, this indicator can increase [11]. Non-immune hydrops fetalis (NHF) characterized by the abnormal accumulation of fluid in at least two fetal compartments in the absence of RBC alloimmunization, including ascites, pleural effusion, pericardial effusion and skin edema. In some cases, it may be also associated with placentamegaly and polyhydramnios [3,15].Non-immune hydrops fetalis has multifactorial causes (more than 150 nosologies), which, according to the results of a large study by Bellini et al. (a systematic review including an analysis of 6361 cases of non-immune hydrops fetalis) were divided into 14 categories: chromosomal abnormalities (13,4%), pathology of the lymphatic system (5,7%), cardiovascular pathology (21,7%), syndromic pathology (4,4%), infections (6,7%), hematological diseases (10,4%), thoracic anomalies (6,0%), TTTS (5,6%), pathology of the urinary system (2,3%), extrathoracic tumors (0,7%), metabolic disorders (1,1%), pathology of the gastrointestinal tract (0,5%), miscellaneous (3,7%) and idiopathic (17,8%) [2].Diagnosis of non-immune hydrops fetalis in the prenatal period using ultrasound is not difficult, but at the same time, determining the etiology of nonimmune hydrops fetalis is considered a difficult diagnostic task, and its successful implementation largely depends on the laboratory and instrumental equipment of hospitals [8].Non-immune hydrops fetalis, manifesting before 22 weeks of gestation, is associated with a high risk of chromosomal abnormalities and adverse outcomes, while after 22 weeks the prognosis is more favorable [8,11].Much attention to the problem of the etiology of non-immune hydrops fetalis is due to the fact that it is a decisive factor in the choice of pregnancy management tactics, intrauterine treatment options and prospects. Thus, according to the Canadian Society of Obstetricians and Gynecologists (SOGC), with a normal fetal karyotype, a gestation period of more than 18 weeks, fetal therapy and/or surgical interventions lead to positive results. The type of intrauterine intervention is determined depending on the etiology, clinical manifestations and concomitant pathology of non-immune hydrops fetalis [8,14].The development of skin edema, especially in the skull area, is a sign of generalized hydrops and is often a sign of the late stage of non-immune hydrops fetalis.
2. Research Material and Methods
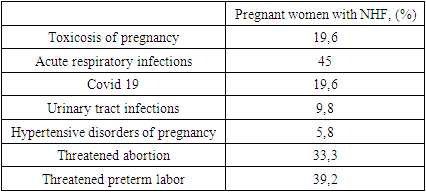
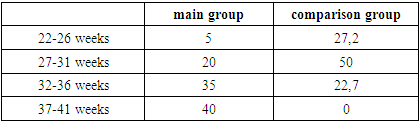
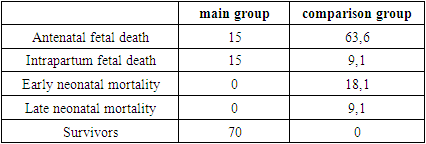
- This study is the first scientific study on non-immune hydrops fetalis in Uzbekistan. The study included 51 pregnant women who were diagnosed with non-immune hydrops fetalis during 2020-2022 at the Republican specialized scientific-practical medical center of obstetrics and gynecology (RSSPMCOG).Criteria for inclusion of study participants:1. Informed consent to participate in the study;2. Age of patients 18-45 years;3. The presence of non-immune hydrops fetalis;4. The participant underwent outpatient and / or inpatient treatment at the RSSPMCOG.Exclusion criteria for study participants:1. Immune hydrops fetalis;2. Lack of medical documentation data;3. The desire of the patient to voluntarily refuse to participate in the study.Nine of 51 pregnant women with NHF had a pregnancy termination in the 1st trimester due to a high risk of chromosomal abnormalities and these women were excluded from further stages of the study. The remaining 42 pregnant women were divided into 2 groups depending on their choice of expectant or active management of pregnancy in NHF. The main group consisted of 20 women who underwent active tactics for NHF, and the comparison group consisted of 22 women who refused active tactics and chose expectant tactics for NHF.Based on the recommendations of the world's leading communities on the management of pregnancy in pregnant women with NHF, as well as on the basis of the clinical and diagnostic capabilities of the state institution RSSPMCOG, an internal protocol for the management of pregnancy in pregnant women with NHF was developed and put into practice in 2020 (Fig.1). Pregnancy in patients of the main group was carried out according to this protocol.
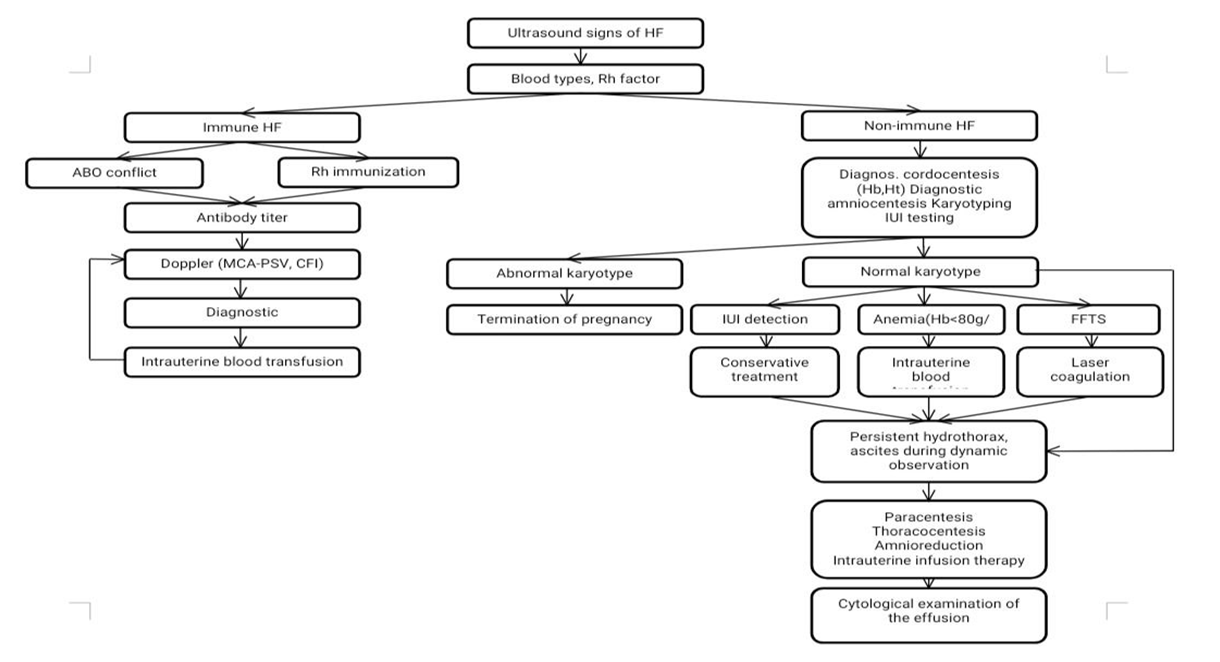 | Figure 1. Internal protocol for the management of pregnancy with NHF |
|
|
3. Comparative Analysis between the Main Group and the Comparison Group
- In the main group, therapeutic measures were carried out depending on the etiopathogenesis and clinical manifestations of non-immune hydrops fetalis:1. Etiopathogenetic treatment: antiarrhythmic treatment, antiviral treatment, immunoglobulin treatment, antibiotic treatment.2. Symptomatic treatment: amnioreduction, thoracocentesis, paracentesis, thoracoamniotic shunting, administration of cardiac glycosides, administration of corticosteroids.The most important part of intrauterine treatment is etiopathogenetic treatment, which depends on the exact etiology. In situations where etiopathogenetic treatment is not possible in the antenatal period, symptomatic treatment is considered the most appropriate, this method allows you to prevent or eliminate complications and prolong pregnancy for a longer period, if possible to the full term, and take it out of etiopathogenetic treatment in the neonatal period. This condition is often observed in pathologies requiring complex surgical interventions [8].The methods of treatment performed in pregnant women of the main group were as follows: etiopathogenetic conservative therapy was most often used in 80% (16/20), including immunoglobulin therapy, antiarrhythmic therapy, antiviral and antibacterial therapy. Amnioreduction was performed in 45% (9/20), paracentesis in 25% (5/20), thoracocentesis in 10% (2/20) and intrauterine drug adminstration in 10% (2/20).There have been a number of large studies on the use of immunoglobulin therapy in pregnancy. Intravenous immunoglobulin can be used in children, newborns, at any stage of pregnancy and is considered safe [9]. Immunoglobulin therapy is used during pregnancy for autoimmune diseases, Rh sensitization, recurrent miscarriage, intrauterine infections and Covid 19 [4,6,13].Aera Han et al (2021) investigated the teratogenic effects of immunoglobulin therapy on the fetus and obstetric complications in their study. The study was conducted on 370 pregnant women in 4 major hospitals in Korea. According to the conclusion of the researchers, the use of immunoglobulin therapy during pregnancy did not increase obstetric complications and indicators of teratogenic effects on the fetus, it was considered safe for the mother and fetus [1].Geriak M. et al (2022) studied the efficacy of immunoglobulin therapy in pregnant women infected with Covid 19. Investigators used intravenous immunoglobulin therapy in combination with glucocorticoid therapy in pregnant women with moderate to severe Covid 19. A positive result was recorded in all pregnant women. According to researchers, immunoglobulin therapy is a safe and effective treatment for pregnant women infected with Covid 19 [10].Immunoglobulin therapy was used in 11 patients of the main group. As indications for immunoglobulin therapy for NHF, it is accepted:Main indications:• Positive results of TORCH infection (PCR, IFA)• High titers of proinflammatory mediators (IL6, PCT, C-reactive protein)Additional indications:• Clinical manifestations of the disease (anamnesis)• Ultrasound signs of infection in the fetus (hyperechoic bowel, ventriculomegaly, placentitis, cardiopathy, hepatosplenomegaly, calcification and hyperechoic areas in parenchymal organs, polyhydramnios)The effectiveness of treatment was assessed by the number of pro-inflammatory mediators and ultrasound markers of inflammation in the fetus. We observed that inflammatory markers decreased after treatment in all cases of immunoglobulin treatment in this study. The drug Valaciclovir was used against the background of immunoglobulin therapy in 7 patients with HSV and CMV viruses. Appointed valaciclovir 1000 mg/day for 5 days. In 3 out of 11 cases (27.3%), the treatment ended ineffectively. In the remaining 8 cases (72.7%), the pregnancy outcome ended positively with the effectiveness of treatment.Fetal arrhythmias in 10% of cases and supraventricular tachycardia in 40-50% of cases cause non-immune hydrops fetalis. Various antiarrhythmic drugs are used for fetal tachyarrhythmias, and digoxin is the drug of choice in many countries for fetal tachyarrhythmias and heart failure [5,7].In our study, 4 cases of fetal tachyarrhythmias were observed, 1 of which was observed in a patient with NHF caused by parvovirus B19. In 7 patients, cardiac glycosides were used to relieve symptoms of fetal heart failure. All our patients underwent slow digitization for 6 days and, with positive dynamics, they were transferred to a maintenance dose, and in all cases, potassium preparations were used along with digoxin to prevent hypokalemia. During the treatment with digoxin, pregnant women underwent ECG, fetal echocardiography, cardiotocography and dopplerometry according to the indicated scheme under strict control. In all cases of fetal arrhythmias 100% (4/4), treatment with digoxin was successfully completed, and therefore there was no need to use other antiarrhythmic drugs (Fig.2). Antenatal and intranatal fetal death, despite treatment, occurred in 3 of 7 cases of heart failure (43%).In the main group, severe polyhydramnios was observed in 45% (9/20) of cases, pregnant women underwent amnioreduction procedures (Fig.3). The indications for amnioreduction were signs of AFI≥35cm or MVP≥15cm.In the main group, fetal paracentesis was performed in 25% (5/25) of patients. In these 25% of cases, the fetus developed severe symptoms of ascites, and fetal paracentesis was performed in cases where conservative treatment was ineffective or impossible (Fig.4). The operation was performed by removing ascitic fluid accumulated in the abdominal cavity of the fetus for the purpose of diagnosis and treatment.
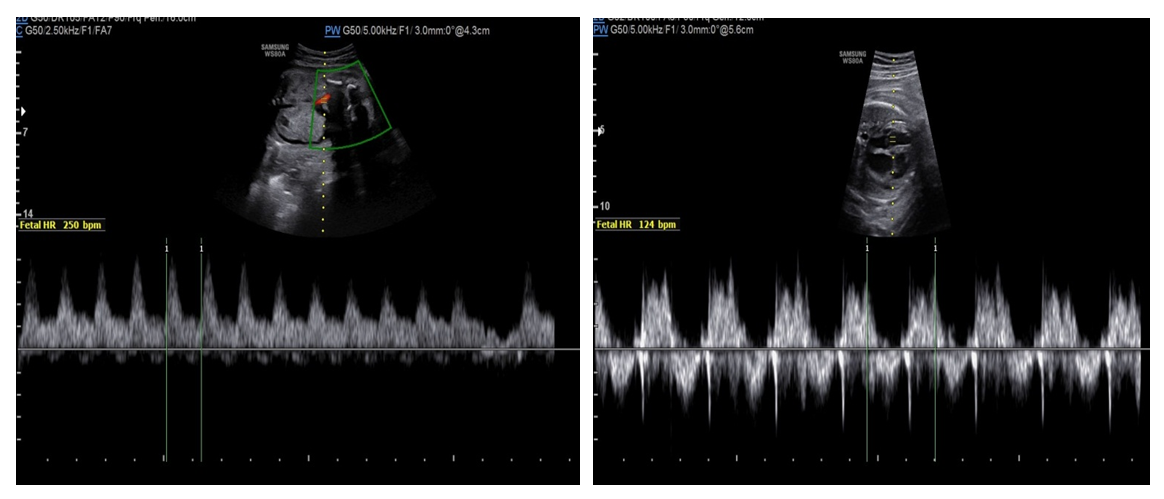 | Figure 2. Patient M. Paroxysmal fetal tachycardia on the left (before treatment with HR-250 per minute). Restored normal sinus rhythm on the right (after treatment with HR-124 beats/min) |
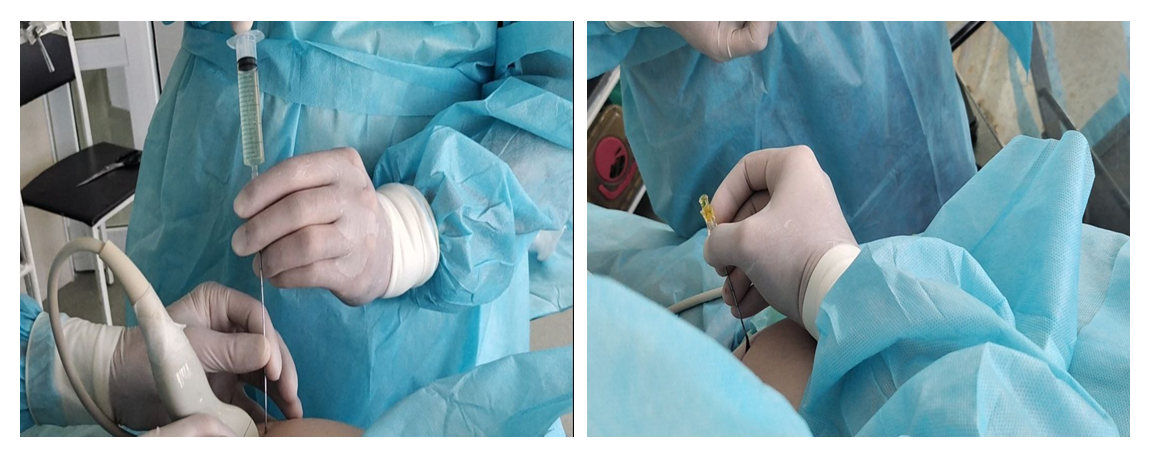 | Figure 3. Amnioreduction |
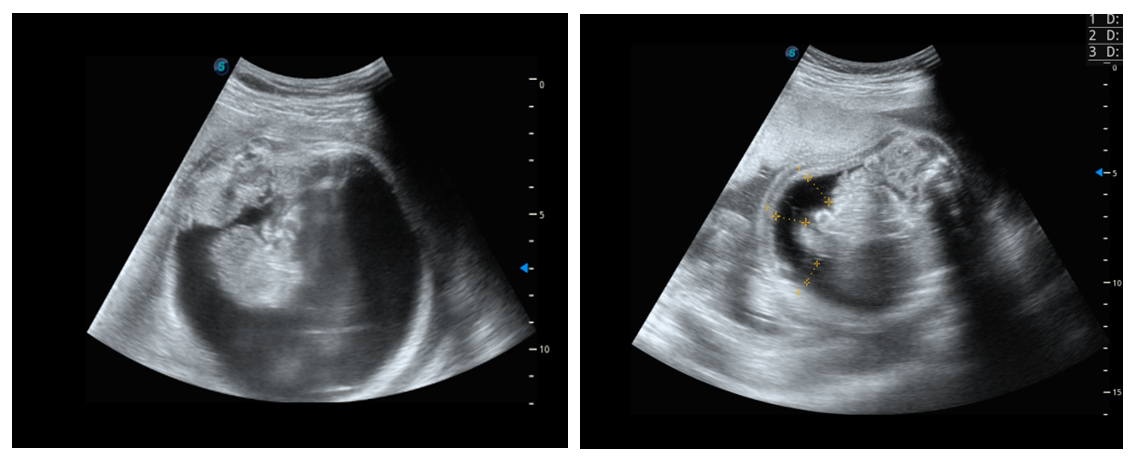 | Figure 4. Patient D. Fetal paracentesis before (left) and after (right) |
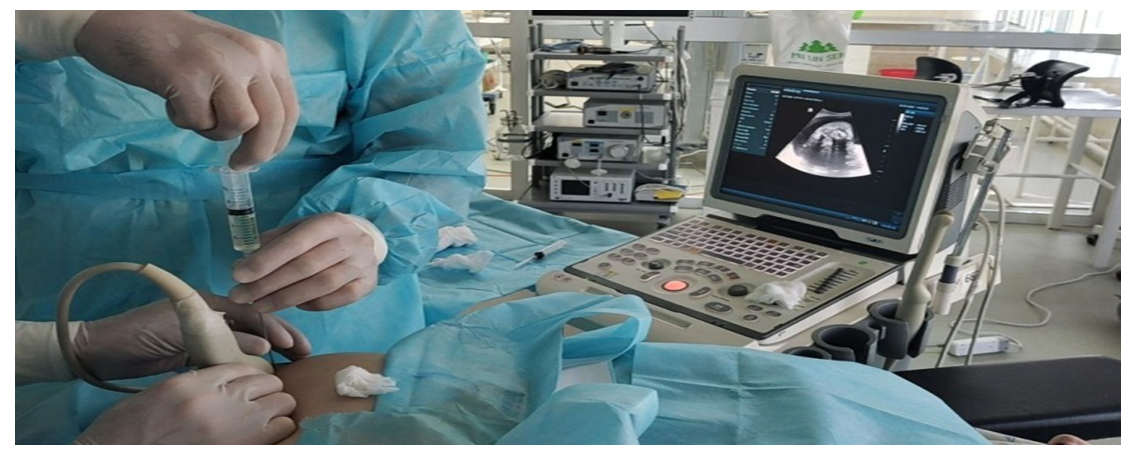 | Figure 5. Patient M. Fetal thoracocentesis process |
|
|
4. Conclusions
- Patients at risk should undergo the following studies: expert ultrasound, fetal Doppler, screening for infections, karyotyping. Early detection of non-immune hydrops fetalis is essential to prevent perinatal morbidity and mortality, and the development of complications should be carefully assessed and monitored in order to initiate treatment in a timely manner. The use of minimally invasive methods of fetal medicine improves the prognosis of this disease. Pregnancy with non-immune hydrops fetalis should be prolonged as long as possible, preferably until full-term pregnancy, especially if active management of pregnancy is chosen. Premature delivery in non-immune hydrops fetalis does not improve perinatal outcomes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML