Ismoilova Nigora Bakhtiyorovna
Assistant of the Department of Neurology, Bukhara State Medical Institute, Uzbekistan
Correspondence to: Ismoilova Nigora Bakhtiyorovna, Assistant of the Department of Neurology, Bukhara State Medical Institute, Uzbekistan.
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
In recent years, issues related to the assessment of cognitive functions in myasthenia gravis have been widely studied. The need for early assessment of cognitive changes in patients with myasthenia gravis, improvement of patient quality of life, improvement of the quality of medical care for patients, and the need to develop a unified principle of patient management became the basis for choosing this research topic. The article presents the results of a comprehensive neuropsychological examination of patients with myasthenia gravis.
Keywords:
Myasthenia gravis, Memory, Neuropsychology, Cognitive, Intellectual
Cite this paper: Ismoilova Nigora Bakhtiyorovna, Study of the Patient's Cognitive and Neuropsychological Condition in Myasthenia Gravis and Evaluation of Its Impact on the Course of the Disease, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 160-164. doi: 10.5923/j.ajmms.20231302.28.
1. Introduction
Worldwide and in Uzbekistan, myasthenia gravis is a rare neurological disease, and women have a higher risk of developing myasthenia gravis than men [7]. The prevalence of myasthenia gravis is 17.5-20.3 per 100 thousand of the population, the figure increases by 5-10% annually. The first signs of myasthenia are manifested in the form of lethargy and weakness of skeletal muscles compared with a high load during the day, in addition, in a calm state, there is a tendency to decrease. The prognosis of myasthenia gravis, in relation to both life and recovery, if pathogenetic therapy is not carried out in a timely manner, is very unfavorable. In recent years, issues related to the assessment of cognitive functions in myasthenia gravis have been widely studied. It is known that the hypothalamus, hippocampal gyrus, midbrain, and cerebral cortex contain acetylcholine receptors that are structurally and genetically similar to receptors on the postsynaptic membrane of the neuromuscular synapse [5,6]. However, the question of the possibility of the interaction of antibodies circulating in the blood with neuronal cholecystitis has been discussed so far noreceptors [7]. Indirect signs of dysfunction of the basal cholinergic system of the brain were revealed according to n u - pillometry and using the method of cognitive evoked potentials of the brain [8,9]. Other authors are of the opinion that due to the ultra-low concentration of antibodies in the cerebrospinal fluid and the structural features of neuronal cholinoreceptors, their interaction is unlikely [10].
2. Purpose of the Study
To identify the main clinical signs of myasthenia gravis, determine the frequency of their occurrence, systematize and develop a scheme for diagnosing the disease during the initial (pre-hospital) examination of the patient.
3. Materials and Methods
92 patients with myasthenia with various forms of the disease were examined (generalized form - 71 (77.3%) patients, ophthalmic - 17 (12.6%), pharyngeal - 34 (10.1%) aged 18 to 72 years and duration diseases from six months to 19 years. In 73 (7.8%) of them, myasthenia gravis was combined with thymoma.. Women were 62 (67.1%), men 30 (32.9%), the average age of patients was 36.2 years Of the 92 patients with myasthenia gravis, 40 (43.3%) underwent thymectomy, the rest of the patients received drug pathogenetic therapy.An analysis of the clinical and neurological development and course of various forms of myasthenia gravis was carried out, depending on the nature of the initial symptoms, the timing (duration) of the development of the full clinical picture of the disease, and the severity of the proserin test. To identify the most significant clinical and neurological criteria for the diagnosis of myasthenia gravis, systematization and evaluation of the results obtained were carried out on the basis of long - term tamnestic observation. Statistical analysis was carried out using the STATISTICA 8.0 package (StatSoft®, Inc., USA).
4. Results and Its Discussion
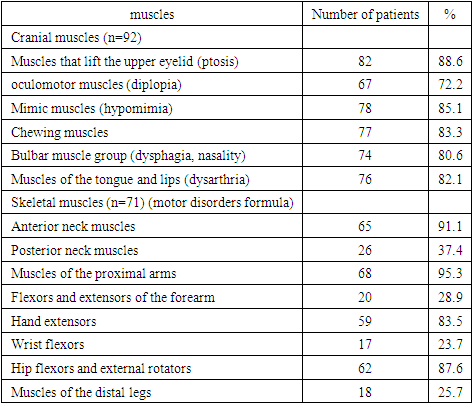
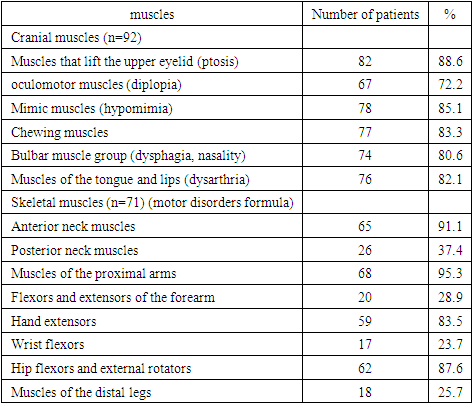
The clinical picture of myasthenia gravis is based on varying degrees of dysfunction of the striated muscles, and the process may involve striated muscles of various localization: cranial, neck, trunk, limbs.In the patients examined by us, the picture of the onset of the disease and the features of its clinical course were quite polymorphic. A high frequency of damage to the cranial muscles and a significant selectivity of damage to the skeletal muscles, which is considered as a specific formula of motor disorders in myasthenia gravis, were revealed (Table 1).Table 1. The frequency of damage to the cranial and skeletal muscles in myasthenia gravis
 |
| |
|
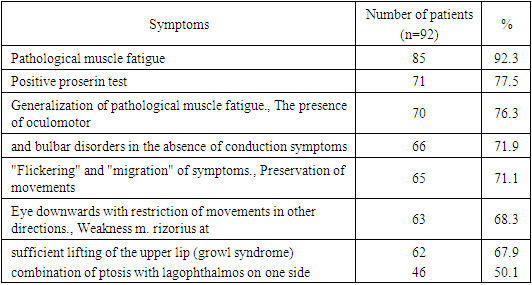
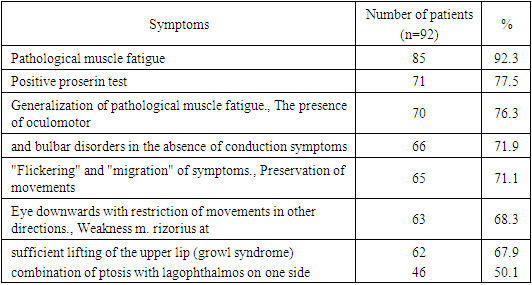
From Table 1 it follows that oculomotor disorders were found much more often and are associated with damage to the external muscles of the eyes. Ptosis was more common (bilateral asymmetric, less often unilateral), which was detected in 82 (88.6%) patients. Its intensity fluctuated during the day, intensifying in the evening. When fixing the gaze (at the level of the horizon line or slightly higher), ptosis increased rapidly, indicating pathological muscle fatigue (pathognomonic symptom of myasthenia gravis). Long-term fixation of the gaze made it possible to detect in 6 (4.6%) patients subclinical pathological weakness of the muscle of the upper eyelid - the appearance of ptosis, which was not noted before the test.In addition to ptosis, according to the results of our observation, 67 (72.2%) patients with myasthenia gravis had diplopia in the vertical, horizontal, or oblique plane, which was caused by weakness of the external muscles of the eye and significantly increased during exercise (visual or physical). Decreased diplopia after rest and in the morning. The severity of the limitation of the movements of the eyeballs in patients with myasthenia gravis was of varying degrees (from mild to complete ophthalmoplegia). In milder cases (43.5%).Diplopia was intermittent and appeared with fatigue of the muscles of the eyes. It should be noted that oculomotor disturbances in myasthenia gravis did not correspond to disturbances in the innervation of the cranial nerves (III, IV and VI pairs).The next symptom of myasthenia in lesions of the muscles of the cranial region was weakness and pathological fatigue of the mimic muscles, which was detected in 78 (85.1%) patients. Myasthenic symptoms mostly evenly spread to all the muscles of the face, but somewhat more often and to a greater extent, the circular muscles of the eyes were affected, the weakness of which increased with general or local physical exertion. In addition, the function of the circular muscle of the mouth and the muscles that pull the corners of the mouth outward (mm. rizorius) were impaired to a greater extent; the strength of the levator lip muscle remained sufficient. In such patients, an unnatural smile was noted, a pathognomonic symptom of "growling" was formed, which was noted in 62 (67.9%) of our patients. The face of patients with myasthenia gravis, as a rule, was hypomous and - soft and unimpressive.Weakness of the masticatory muscles was noted in 77 (83.3%) of our patients with myasthenia gravis, but the degree of its severity was different: from slight fatigue during chewing, which practically did not disturb food intake, to permanent paralysis, when the act of chewing became almost impossible.An important clinical syndrome in myasthenia gravis was paresis or paralysis of the bulbar muscle group, which manifested itself as a swallowing disorder as a result of dysfunction of the predominantly pharyngeal muscles. In 74 (80.6%) of our patients, swallowing disorder was detected in varying degrees: from slight "choking" during meals to complete inability to swallow even saliva. It should be noted that this syndrome, much more often than other myasthenic symptoms, was proserin -resistant, and, consequently, was stopped worse by anticholinester’s - drugs.Speech impairment was also observed quite often and was detected in 76 (82.1%) patients and was expressed by dysphonia, up to aphonia (due to weakness of the muscles of the larynx), nasal (due to weakness of the muscles of the soft palate) and dysarthria (due to difficulty in movements). tongue and lips).Along with the muscles of the cranial region, in most cases with myasthenia gravis, the function of the muscles of the neck, trunk, and extremities was impaired as a result of the generalization of the myasthenic process.Pathological weakness of the skeletal muscles was revealed as a result of a detailed study of the initial strength in all muscle groups and after exercise (repeated contractions). In addition to the general generalization of the myasthenic process in the skeletal muscles in myasthenia, there was some selectivity of muscle weakness, which is typical and most constant. The presence of such a feature allows us to speak about the formula of motor disorders in this disease. It should be noted that the selectivity of muscle weakness was more pronounced in skeletal muscles than in cranial ones.To assess the clinical and neurological diagnostic significance of the formula for movement disorders, we analyzed the selectivity of skeletal muscle damage in 716 patients with generalized myasthenia gravis (Table 1). It follows from the table that in 65 (91.1%) patients, lesions of the anterior neck muscle group were detected, much less often - in 26 (37.4%) patients, the posterior neck muscle group suffered.In the proximal parts of the upper extremities in 68 (95.3%) patients, the dentate, deltoid, pectoral and infraspinatus muscles were predominantly affected, which made it difficult or limited to raise the arms to and above the horizontal, bring them forward (to the medial line) and rotate outwards. The muscle strength of the flexors and extensor of the forearm often remained intact and only in 20 (28.9%) patients decreased slightly. In the distal parts of the hands, in 59 (83.5 %) patients, the extensors of the hand and fingers, as well as the abductors and adductors of the fingers, were predominantly affected, often unevenly. The ulnar group suffered the most (usually the 4th and 5th fingers). Significantly less often and to a lesser extent, weakness in the flexors of the distal arms was revealed - in 17 (23.7%) patients.In the lower limbs, in 62 (87.6%) patients, the proximal muscle group was affected to a greater extent - the flexors and external rotators of the thighs. The strength of the thigh muscles often remained intact, and the decrease in the strength of the leg flexors was less pronounced and was observed in 50 (70.7%) patients. Movement disorders in the distal parts of the legs were relatively rare, only in 18 (25.7%) patients, mainly with severe myasthenia gravis, more often in the extensors of the feet.Trunk muscles were affected in 54 (76.5%) patients, more often evenly and with a moderate degree of severity. However, in severe generalized form of myasthenia gravis in 78 (10.9%) patients, the pathological process spread to the intercostal muscles, which led to difficulty in breathing in the form of a feeling of “lack of air”.Our studies showed that the formula of movement disorders was clearly registered in 65 (91.9%) patients, which is a pathognomonic symptom of myasthenia gravis.In addition, we analyzed and identified a number of the most common pathognomonic diagnostically significant symptoms, with existing only myasthenia gravis, and revealed their frequency of occurrence (Table 2).Table 2. The frequency of occurrence of the most significant symptoms for the diagnosis of myasthenia gravis
 |
| |
|
There are several contemporary issues related to MG that remain to be resolved. Issues pertaining to MuSK MG include determining the pathophysiologic role of MuSK antibodies in the development of MG, whether the immunological attack on the endplate region in MuSK MG is similar to that of SP MG, and whether thymectomy benefits patients with MuSK MG. The benefit of thymectomy in non-thymomatous SP MG is poorly defined at present, and an international, multicenter trial is currently being undertaken to determine whether and to what degree thymectomy is beneficial in non-thymomatous disease. Whether corticosteroid treatment begun early in the course of ocular MG can prevent generalization has yet to be demonstrated. Finally, it remains to be determined whether and under what circumstances can immune modulation be discontinued without significant risk of relapse in MG patients that have achieved remission with immunotherapy.So, for example, the variability of the localization of ptosis of the upper eyelid (the appearance of ptosis on one side, its disappearance and then appearance on the other side), changing variants of oculomotor disorders or their replacement with bulbar symptoms exclude any focal process in the central nervous system and orient to the presence of pathology. synaptic transmission. Such variability of symptoms was found in 65 (71.1%) of our patients.An analysis was made of several more basic diagnostic features and special research techniques that facilitate the clinical recognition of myasthenia gravis.The first of these is a clear dissociation between the usually pronounced oculomotor and bulbar disorders (which resembles an organic lesion of the brain stem) and the absence of any conduction disorders. This dissociation of symptoms was clearly observed in 66 (71.9%) patients.The second diagnostic sign, which was revealed in 46 (50.1%) patients, is a peculiar and illogical (from the standpoint of the localization of the organic process) combination of symptoms. For example, the combination of ptosis of the upper eyelid on one side with pronounced lagophthalmos on the same side (according to the routine schemes of topical diagnostics, such phenomena occur with lesions of different levels of the trunk).As an example, we can also mention the frequent preservation of eye movements downwards with limitation or impossibility of their movements in other directions, which contradicts the classical ideas about the symptoms of an organic stable lesion of the oculomotor nerves and their nuclei, which was recorded in 63 (68.3%) patients. All these phenomena make it possible, already at the first examination of the patient, to reject assumptions about an organic lesion of the nervous system and to suspect the possibility of a disease of the neuromuscular system.The next step in the clinical diagnosis of myasthenia gravis is a special targeted technique, which, as a result of repeated active movements, allows you to register an increase in pathological muscle fatigue leading to paresis or paralysis and restore them to their original state after rest. This pathognomonic symptom of myasthenia gravis was detected in 85 (92.3%) of our patients. In 70 (76.3%) patients, a pathognomonic, inherent only in myasthenia, phenomenon of “generalization of muscle fatigue” was also registered. Its peculiarity lies in the fact that with the fatigue of some muscle groups, weakness arises or increases in other muscle groups that were not subjected to direct load. One of the most frequent manifestations of this phenomenon is the “oculo-palpebral symptom”, described by V.S. Lobzin: with repeated horizontal eye movements, ptosis of the upper eyelids appears or increases.In a clinical examination of patients, an essential diagnostic criterion is a proserine test, which is based on the detection of pathological muscle fatigue. Patients were injected subcutaneously with 2.0 ml of a 0.05% prozerin solution. Muscle strength was assessed according to a five-point system before the introduction of prozerin and after 30-40 minutes. In the presence of myasthenia, there was a complete or partial regression of my asthenic symptoms. The results were evaluated depending on the reduction of symptoms: a sharply positive test - the disappearance of all myasthenic symptoms, a positive proserin test - regression of most myasthenic symptoms, weakly positive - all symptoms persist, but their severity decreases markedly, a doubtful test - a slight regression of myasthenic symptoms. Diagnostically significant criteria are the first three variants of the proserin test, which were identified in 71 (77.5%) of our patients.Based on the results of the study, in order to optimize the clinical diagnosis of myasthenia gravis, we analyzed the frequency of occurrence of the most significant symptoms of the disease. The results of the study showed that the most frequent and pathogenic The main symptoms of myasthenia gravis are pathological muscle fatigue (92.3%) and a specific form of movement disorders (91.9%), which was found in patients with a generalized form of myasthenia gravis.As already mentioned, the myasthenic formula of motor disorders is determined by the selectivity of the defeat of individual muscle groups and the severity of their weakness. For example, in our patients with a generalized form of the disease, the following muscle groups were most often affected: muscles of the proximal arms (95.3%), anterior neck muscles (91.1%), extensors of the hand and fingers, abductors and adductors of the fingers (83.5%), flexors and external rotators of the hips (87.6%). The muscles of the distal legs (25.7%), flexors of the hands (23.7%), flexors and extensors of the forearms (28.9%) were involved and posterior neck muscles (37.4%). It should also be noted that in this muscle group, the severity of pathological muscle fatigue was only mild or moderate.The second most common group of clinical signs of myasthenia gravis is a positive proserin test (77.5%), generalization of pathological muscle weakness to muscles not involved in physical activity (76.3%), dissociation between severe oculomotor and bulbar disorders, and the absence of conduction symptoms (71.9%), “flickering” of symptoms - their instability during the day, week (71.1%), decreased strength of the calf flexors (70.7%). Somewhat less common is such a pathognomonic symptom as a combination of ptosis with lagophthalmos on one side (50.1%).
5. Conclusions
The presented features of the clinical manifestations of myasthenia gravis, the frequency and combination of pathognomonic symptoms of the disease, the presence of pathological muscle fatigue and the selectivity of lesions of individual muscle groups (myasthenic formula of movement disorders) made it possible to develop a clinical diagnostic scheme, the use of which makes it possible already at the first (prehospital) examination of the patient to diagnose myasthenia gravis or suspect the disease.
References
| [1] | Agafonov B.V., Kotov S.V., Sidorova O.P. Myasthenia gravis and congenital myasthenic syndromes. - M.: Medical Information Agency, 2013. - 224 p. |
| [2] | Gadzhiev S.A., Dogel L.V., Vanevsky V.L. Diagnosis and surgical treatment of myasthenia gravis. - L.: Medicine, 2019. - 255 p. |
| [3] | Kuzin M.I., Gecht B.M. Myasthenia. - M.: Medicine, 2016. - 224 p. |
| [4] | Sepp E.K., Lantsova V.B. Myasthenia. - M.: Nevromed, 2008. - 112 p. |
| [5] | Baranov, V.V. Optimization of the diagnosis and treatment of myasthenia gravis (clinical-immunol. and with - next): Abstract of the thesis. dis.... cand. honey. n auk. - St. Petersburg, 2003. - 24 p. |
| [6] | Gecht B.M., Lantsova V.B., Sepp E.K. The role of autoantibodies to AChR in the pathogenesis of myasthenia gravis // Neurological journal. - 2013. - V. 8, Appendix No. 1. - S. 35-37. |
| [7] | Hamed S, Mohamed M, Youssef A, et al. Assessment of cognitive function in patients with myasthenia gravis. NeuroimmunolNeuroinflamm. 2014; 1 (3): 141. doi: 10.4103/2347-8659.143671. |
| [8] | Ходжиева, Дилбар Таджиевна, and Нигора Бахтиёровна Исмоилова. "ИЗУЧЕНИЕ клинико-неврологических особенностей миастении, оптимизация лечения. (литературный обзор)." журнал неврологии и нейрохирургических исследований 3.5 (2022). |
| [9] | Xuseynovna KSA et al. Optimization of the Diagnosis and Treatment of Oral Epulis Based on Morphological and Cytological Analysis // Texas Journal of Medical Science. - 2022. - T. 6. - S. 24-26. |
| [10] | Khaidarova DK, Kazakov B. Sh. - 2021. - Vol. 2. - No. 4. |
| [11] | Khodzhieva, Dilbar Tadzhievna, Dildora Kadirovna Khaidarova, and Sitora Bakhramovna Barnaeva. "Clinical and neurological aspects of the study of risk factors for vascular seizures in hemorrhagic stroke." journal of neurology and neurosurgical research 3.2 (2022). |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML