-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 147-152
doi:10.5923/j.ajmms.20231302.25
Received: Feb. 7, 2023; Accepted: Feb. 19, 2023; Published: Feb. 22, 2023

Combination of the Upper Urinary Tract and Bladder Drainage Methods after Laparoscopic Uretercystoneoanastomosis
M. M. Bakhadirkhanov1, Sh. T. Mukhtarov1, F. A. Akilov2, B. A. Ayubov1, D. A. Nazarov1, F. R. Nosirov1, Kh. Z. Nuriddinov1
1Republican Specialized Scientific-Practical Medical Center of Urology, Tashkent, Uzbekistan
2Tashkent Medical Academy, Department of Urology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

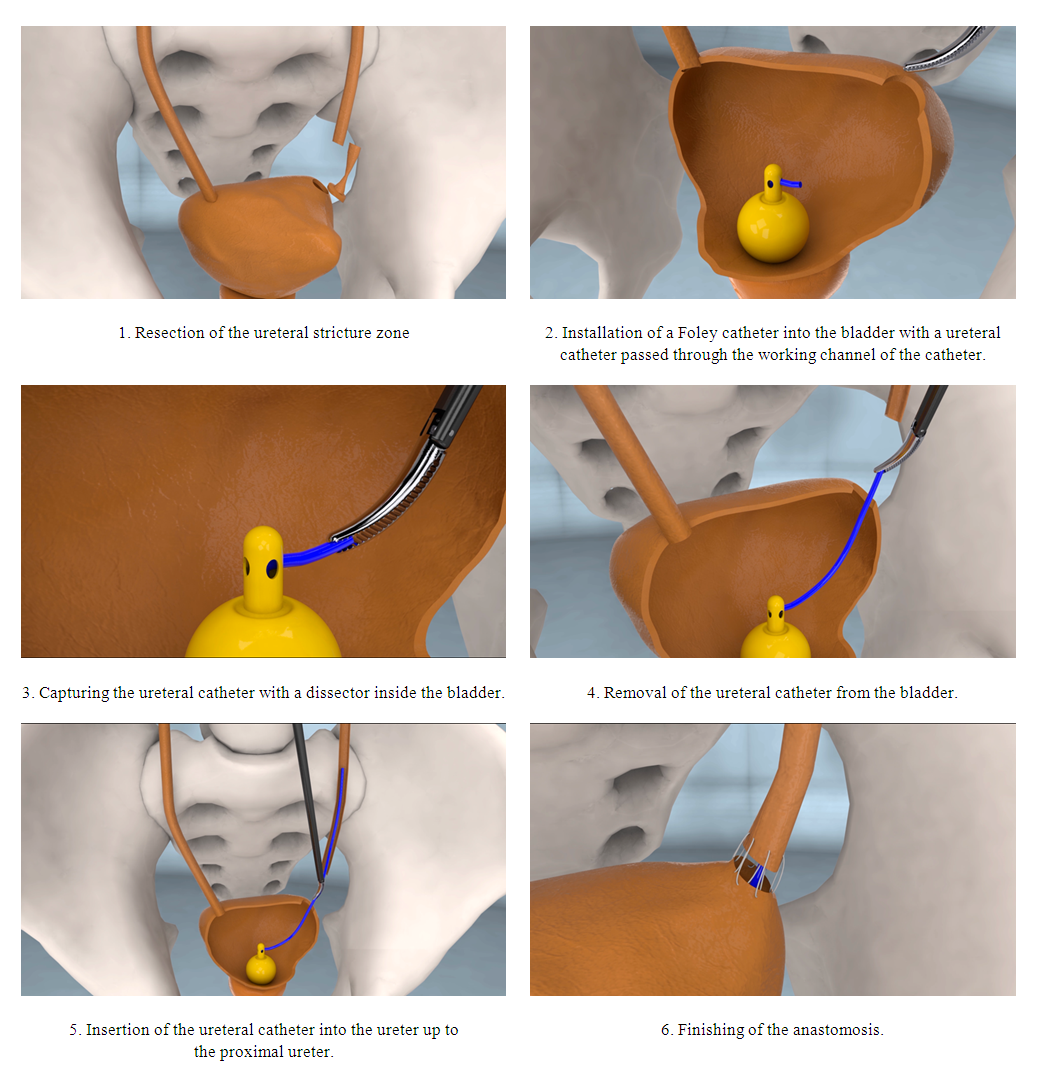
The aim of the study was to evaluate the efficiency and safety of the upper urinary tract and bladder combination drainage method after laparoscopic uretercystoneoanastomosis. Introduction. Laparoscopic interventions have developed from a simple diagnostic procedure into complex reconstructive surgeries. One of the reconstructive procedures performed in urology is laparoscopic ureterocystoneoanastomosis or reimplantation of the ureter. The authors developed an alternative technique for drainage of the upper urinary tract and bladder during laparoscopic ureteroneocystostomy without the use of a ureteral stent. Material and methods. 40 patients who received surgical treatment of the lower third of the ureter stricture in the period from 2019 to 2022 were selected for the study. The mean age of all patients was 31.9 ± 14.0 years (M±δ). All patients were divided into 2 groups according to the upper urinary tract drainage method and intubation of the ureter. Group A consisted of 23 patients who were used a ureteral stent. Group B consisted of 17 patients who were performed the developed technique of a combination of bladder and ureter drainage of the upper urinary tract and intubation of the ureter. Results. The mean duration of surgery was lower when using a ureteral stent (103.3 ± 12.3 minutes versus 122.1 ± 14.0 minutes; M±δ). The analysis of intraoperative blood loss, intensity of postoperative pain and duration of inpatient treatment revealed no difference between the groups. The median duration for the removal of the urethral catheter in the group with a ureteral stent was lower than the new technique group (8 days versus 18 days). However, the median duration of ureteral intubation was lower with the new technique in comparison with the ureteral stent (18 days versus 29 days). The frequency of postoperative complications did not differ between the groups. Conclusion. The developed technique of combination drainage for the bladder and ureter during laparoscopic uretercystoneoanastomosis has similar efficacy and safety in compare with the use of an ureteral stent.
Keywords: Laparoscopy, Ureteroneocystostomy, Ureteral stent, Urethral catheter, Ureter reimplantation
Cite this paper: M. M. Bakhadirkhanov, Sh. T. Mukhtarov, F. A. Akilov, B. A. Ayubov, D. A. Nazarov, F. R. Nosirov, Kh. Z. Nuriddinov, Combination of the Upper Urinary Tract and Bladder Drainage Methods after Laparoscopic Uretercystoneoanastomosis, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 147-152. doi: 10.5923/j.ajmms.20231302.25.
1. Introduction
- Laparoscopic interventions have developed from a simple diagnostic procedure into complex reconstructive surgeries. Today, the advantages of this method over open interventions are no longer in doubt, and laparoscopy has almost completely replaced open surgery as the first line of treatment for various urological diseases [1]. One of the reconstructive procedures performed in urology is laparoscopic ureterocystoneoanastomosis (UNC) or reimplantation of the ureter. Ureteral reimplantation is most often performed in pediatrics for the treatment of vesicoureteral reflux. In adults, reimplantation of the ureter is indicated for the strictures of the lower third of the ureter. The ureteroneocystostomy with or without Psoas-hitch is the standard surgery in such cases. Ureteral stent is used for drainage of the upper urinary tract (UUT) and ureteral intubation in laparoscopic UNC. However, this type of drainage is associated with a high frequency of postoperative complications [2]. Alternative methods of UUT drainage and ureteral intubation have not been described in the literature. We have developed a special method for combining drainage of the upper urinary tract and the bladder during laparoscopic UNC. The aim of the study was to evaluate the efficiency and safety of the upper urinary tract and bladder combination drainage method after laparoscopic uretercystoneoanastomosis.
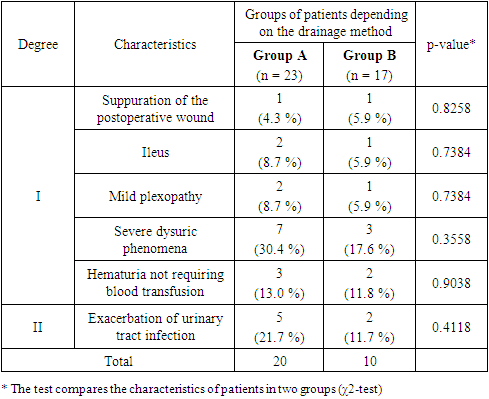
2. Material and Methods
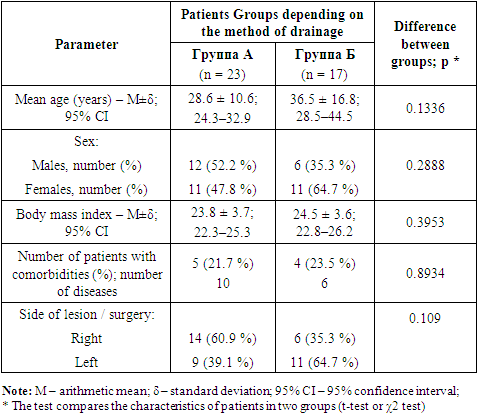
- 40 patients who received surgical treatment of the lower third of the ureter stricture in the period from 2019 to 2022 at the Republican Specialized Scientific-Practical Medical Center of Urology. The mean age of all patients was 31.9 ± 14.0 years (M±δ). There were 18 (45%) males and 22 (55%) females. All patients were performed standard clinical, laboratory and instrumental examinations: a complete blood count, biochemical blood analysis, ultrasound and X-ray investigation methods. The diagnosis of the disease was determined on the basis of the clinical picture, ultrasound examination and multispiral computed tomography with urinary tract contrast. Laparoscopic pyeloplasty was performed using endovideosurgical equipment and instruments of KARL STORZ company (Germany). All surgeries were performed by one surgeon. Surgical intervention was performed according to the standard technique. The patient was placed in the Trendelenburg position with the operating table tilted 15-45°. Access to the abdominal cavity was carried out according to the Hasson method. After installing trocars and inserting instruments into the abdominal cavity through the Todlt line, the corresponding part of the large intestine was mobilized and the retroperitoneal space was opened. Having identified the ureter and the narrowed area, it was resected. The normal end of the ureter was spatulated. The bladder was filled with isotonic solution and a cystotomy was performed at the site of ureter implantation. The anastomosis began with the application of a muscle retaining suture that passed through all layers of the bladder and ureter wall. The ureter was placed in the detrusor trough, and then the edges of the detrusor muscle were brought together over the ureter, creating a submucosal tunnel. A ureteral catheter or stent was installed to drain the upper urinary tract before completing the anastomosis. We have developed a technique for combining methods of the upper urinary tract and bladder drainage during laparoscopic uretercystoneoanastomosis. In this technique a ureteral catheter has been passed through the Foley catheter. First, the balloon has been inflated with isotonic solution up to 3-5 ml or with air. A hemostatic clamp has been inserted into the inner hole of the Foley catheter and new hole is made on the catheter between the inner hole itself and the balloon. Then, the balloon has been deflated. The ureteral catheter is grasped with a clamp and pulled inside the new hole. Then a clamp is passed into inner hole and exit through a new hole next to the ureteral catheter. The other end of the ureteral catheter is grasped with a clamp and pulled inwards. With the fingers of the hand or a clamp, the entire catheter is dragged through the working channel of the Foley catheter and brought out. By injecting 3-5 ml of isotonic sodium chloride solution into a special channel of the can, its integrity is checked. The prepared catheter is shown in Figure 1.
 | Figure 1. Foley catheter 18 Fr with a conducted ureteral catheter |
 | Figure 2. Various stages of the combination of bladder and upper urinary tract drainage with ureteral intubation during laparoscopic ureteroneocystostomy |
|
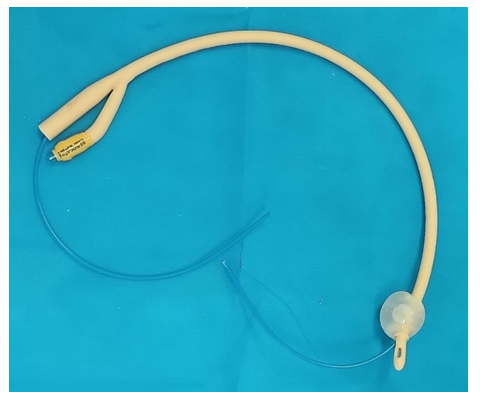
3. Results
- The mean duration of surgery in group A who had a ureteral stent placed during UNC was 103.3 ± 12.3 minutes (M±δ). And in patients of group B, who were performed the developed technique for combining drainage of the bladder and ureter, the duration of the surgery was 122.1 ± 14.0 minutes (M±δ). Statistically significant difference (p < 0.05) in the duration of the surgical intervention may be related to the additional time required for the preparation of the Foley catheter and the difficulty of inserting the ureteral catheter into the ureter (Fig. 3).
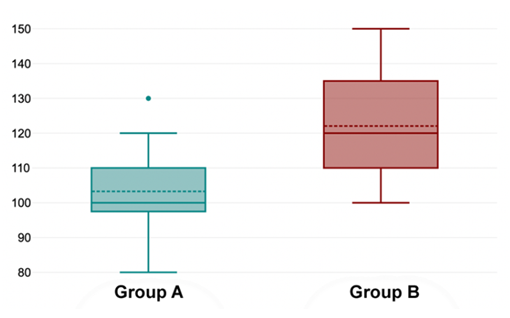 | Figure 3. Boxplot of the duration of surgery in comparison of two groups (p < 0.05): Group A - ureteral stent (n =23); Group B - a combination of drainage of the bladder and ureter (n = 17) |
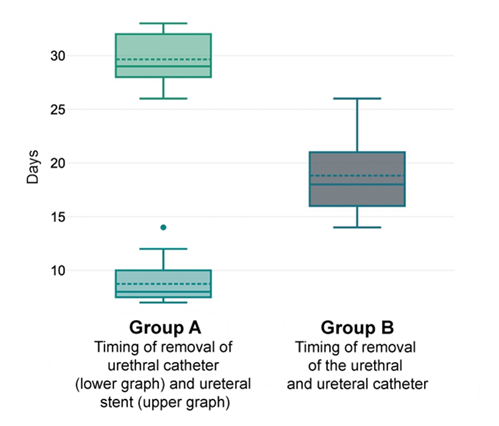 | Figure 4. Comparative boxplots analysis of the urinary tract drainage duration after laparoscopic UNC in two groups (p < 0.05) |
|
4. Discussion
- Laparoscopic surgery has become an integral part of urological practice. Laparoscopic surgery has become an integral part of urological practice. The possibility of performing laparoscopic ureterocystoneoanastomosis was first described by R.M. Ehrlich et al. in 1994 [5]. E. M. McDougall in 1995 performed a laparoscopic ureteral reimplantation on pigs and showed the possibility of creating an antireflux mechanism [6]. Over the past decade, several studies have evaluated laparoscopic ureteral reimplantation and good results and a low complication rate even in cases of complex anatomy were received [7,8]. In 2016, Farina et al. conducted a systematic review evaluating laparoscopic ureteral reimplantation. They concluded that the technique was safe and effective. They reported success rates of up to 96%, shorter hospital stay, less bleeding and less pain in compare with open surgery [9]. M. Riquelme et al. reported a success rate of 95.8% in 81 patients with minor complications requiring reoperation in 2 (2.4%) cases [9]. Rohan Batra et al. compared laparoscopic and robotic UNC and reported about the efficiency of 94.7% and 95.5%, respectively [10]. The efficiency of laparoscopic UNC in our study was 97.5%.Gupta et al. comparatively evaluated the results of open and laparoscopic UNC. According to the authors, laparoscopic UNC takes longer time (228 minutes), associated with less bleeding (166 ml) and less hospital stay (5.36 days). However, the efficiency of the operation was less than open surgery (96% versus 100%, respectively) [11]. In our study, the average duration of the surgery was 103.3 ± 12.3 minutes (M±δ) in Group A, and 122.1 ± 14.0 minutes (M±δ) in Group B, and the median volume of blood loss in both groups was 50 ml. Similar results were obtained in the study of Zhu et al: the duration of the surgery – 115.0 ± 19.5 minutes, blood loss volume 10.0 ± 1.8 ml [12]. Many authors described postoperative complications of laparoscopic UNC in their studies. So, there were 22.4% of postoperative complications cases in the study of D. F. Alcaraz in patients who underwent laparoscopic UNC. In this study, postoperative wound suppuration and ileus were not observed in the laparoscopic UNC group, while in the open surgery group it was 12% and 8%, respectively [13]. However, in our study, 2 (5.0%) patients had suppuration of the postoperative wound and 3 (7.5%) patients had ileus. Studies report a very high incidence of exacerbations of urinary tract infections (48-68 %) [5,10,13,14], which was not revealed in our research. This complication occurred in 17.5% of cases.In all studies ureteral stent was used for ureteral intubation and drainage of the upper urinary tract. Alternative drainage methods have not described in the literature.
5. Conclusions
- The developed technique of combining drainage of the bladder and ureter during laparoscopic UNC has similar efficiency and safety in compare with the use of a ureteral stent. However, the duration of the surgical intervention is lengthened due to the time required to prepare the drainage. Although our proposed method is effective and safe, we think further studies are needed in the long term.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML