-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 134-137
doi:10.5923/j.ajmms.20231302.22
Received: Jan. 31, 2023; Accepted: Feb. 13, 2023; Published: Feb. 22, 2023

Combined Inguinal Hernia Repair
Usarov Sherali Nasritdinovich1, Davlatov Salim Sulaymonovich2, Rakhmanov Kosim Erdanovich1
1Samarkand State Medical University, Samarkand, Uzbekistan
2Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Usarov Sherali Nasritdinovich, Samarkand State Medical University, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction. Inguinal hernias are among the most common hernias in the world. They are diagnosed more often among men, 10 or more times higher than among women. Objective of the study: to increase the efficiency of surgical treatment of inguinal hernias by improving the technology of strengthening both walls of the inguinal canal. Materials and research methods. The study is based on the results of surgical treatment of 47 patients who underwent hernioalloplasty for inguinal hernia in the surgical department of the clinic of the Samarkand State Medical Institute. Research results. Of the 47 performed hernioalloplasty in 14 (29.8%) cases (the main group), we used the modified method of hernioalloplasty of inguinal hernias. In these patients, after a conventional skin incision, the aponeurosis of the external oblique abdominal muscle was dissected. Highly isolated and removed the hernial sac. Then followed the isolation of the spermatic cord along its entire length. The transverse fascia was exposed at the inner opening of the inguinal canal. The mesh graft 10 × 15 cm was opened intraoperatively, considering individual characteristics. Conclusions. The presented technique of reconstruction of the inguinal canal, aimed at reducing trauma and reducing the time of intervention, can be used in wide practice.
Keywords: Inguinal hernia, Inguinal canal, Graft, Recurrence, Complication
Cite this paper: Usarov Sherali Nasritdinovich, Davlatov Salim Sulaymonovich, Rakhmanov Kosim Erdanovich, Combined Inguinal Hernia Repair, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 134-137. doi: 10.5923/j.ajmms.20231302.22.
Article Outline
1. Introduction
- Inguinal hernias are among the most common hernias in the world. They are more often diagnosed among men, 10 or more times higher than among women [4,9]. However, the existence of inguinal hernias in women should not be discounted because they can occur and are often present differently than in men. For example, men tend to exhibit a mostly bulging mass in the groin, sometimes with accompanying pain. Women tend to have groin pain radiating to the upper thigh, vagina or around the lower back, and may not have a bulging mass in the groin [3]. Surgery for inguinal hernias is the most frequent among elective surgical interventions [1]. At the end of the 19th century, the basic principles of the surgical treatment of inguinal hernias were determined. The classic Bassini method of inguinal hernioplasty served as the basis for various options for inguinal autogernioplasty. Some of them are widely used in surgical practice. However, autogernioplasty performed using the patient's own tissues does not lead to sufficient strength of the restored structures of the groin region and is often accompanied by relapses (10% in primary and up to 30% in repeated hernioplasty) [1,2].Surgical treatment of inguinal hernias using traditional methods involves plastic surgery aimed at strengthening the anterior or posterior wall of the inguinal canal. The operation is performed without the use of foreign materials.The Marcy repair was developed in 1892 and is used only for oblique inguinal hernias. This technique involves the reduction of the hernial sac and the closure of the internal inguinal canal by applying one to three sutures. This leads to tension in the tissues of the inner inguinal ring, which in turn causes the formation of recurrent oblique inguinal hernias, and to a change in the direction of efforts in the area of the bottom of the inguinal canal, which can lead to the formation of direct recurrent inguinal hernias.The Bobrov-Girard method strengthens the anterior wall of the inguinal canal. Above the spermatic cord, first the edges of the internal oblique and transverse abdominal muscles are sewn to the inguinal ligament, and then with separate sutures - the upper flap of the aponeurosis of the external oblique abdominal muscle. The lower aponeurosis flap is fixed with sutures on the upper aponeurosis flap, thus forming a duplicate.Method S.I. Spasokukotsky is that the inner aponeurosis flap of the external oblique abdominal muscle together with the edges of the internal oblique and transverse abdominal muscles is sutured to the inguinal ligament with one row of interrupted silk sutures. Then the outer flap of the aponeurosis is sutured over the inner one.With Cooper's ligament or McVay plastic surgery, the bottom of the inguinal canal is pulled laterally and fixed to the Cooper's ligament under the inguinal ligament. This leads to tissue tension in the area of the bottom of the inguinal canal. To relieve the tension in the tissues of the bottom of the inguinal canal resulting from this method, incisions are often made in the anterior rectus abdominis muscle.Method M.A. Kimbarovsky. After processing and cutting off the hernial sac, the inner flap of the dissected aponeurosis and the underlying muscles are stitched from outside to inside, retreating 1 cm from the edge of the incision. The needle is passed again only through the edge of the internal flap of the aponeurosis, going from the inside out, then the edge of the inguinal ligament is stitched with the same thread. Having applied four or five such stitches, they are tied in turn; while the edge of the internal flap of the aponeurosis is tucked under the edge of the muscles and brought into close contact with the inguinal ligament.The Bassini method is aimed at strengthening the posterior wall of the inguinal canal. After removing the hernial sac, the spermatic cord is pushed aside and under it the lower edge of the internal oblique and transverse muscles is sutured together with the transverse fascia of the abdomen to the inguinal ligament. The spermatic cord is placed on the formed muscle wall. Deep suturing helps to restore the weakened posterior wall of the inguinal canal. The edges of the aponeurosis of the external oblique muscle are sutured edge to edge above the spermatic cord.Plastic on Shouldice is a modification of plastics Bassini, assumes a four-bottom closure of the inguinal canal. After dissection of the oblique hernial sac (if any), the bottom of the inguinal canal is opened from the inner inguinal ring to the pubis. The bottom of the inguinal canal is then closed using four layers of continuous sutures so that the medial edge of the bottom of the inguinal canal overlaps its lateral edge. The next two layers overlap the first two layers, while the edge of the rectus abdominis muscle is pulled closer to the inguinal ligament. When using this technique, the main tissue tension occurs in the area of the bottom of the inguinal canal.The Kukudjanov method is proposed for straight and complex forms of inguinal hernias. It consists in suturing between the outer edge of the vagina of the rectus abdominis muscle and the superior pubic ligament (Cooper's) from the pubic tubercle to the fascial sheaths of the iliac vessels. Then the connected tendon of the internal oblique and transverse muscles together with the upper and lower edges of the dissected transverse fascia is sutured to the inguinal ligament [2, 4, 6]. I. Lichtenstein et al. in search of ways to reduce the number of relapses (1987, 1991) created the concept of a tension-free technique. According to the authors, tension stitching of dissimilar tissues is the main cause of recurrent hernias, as it does not correspond to the biological laws of wound healing. The use of various implants for hernia repair has led to a significant decrease in the number of relapses. The results of using Lichtenstein plastic surgery in non-specialized surgical centers are close to the results of treatment in specialized clinics, which proves the simplicity, safety and effectiveness of the technique. Over the past decades, Liechtenstein plastic has become widespread throughout the world [4,10].For radical treatment, only surgical methods of treatment are used, since defects in the abdominal wall are not capable of recovery and regeneration. Surgical methods of treatment are numerous, and long-term results are not always successful, since for a long-time due attention was not paid to the posterior wall of the inguinal canal as the main supporting anatomical structure [2,3].Modern herniologists L. Nyhus, RE Condon, et al. Argue that any inguinal hernia is the result of a stretching or defect in the transverse fascia. According to the literature, in Russia in 1 year more than 200,000 hernioplasty for inguinal hernias are performed, of which more than 70% are performed by traditional methods. In the United States, out of 700,000 hernia repairs, relapses occur in 10-15%, and the cost of retreatment is more than $ 28 million [4,12].The problem of choosing a relapse-free method of surgical treatment of patients with inguinal hernias has been and remains relevant, due to the wide spread of the disease and the predominant lesion of people of working age (3-7% of the male working population) [2].To date, a large amount of material has been accumulated on the study of the pathogenesis and etiology of inguinal hernias, numerous methods of surgical treatment have been described, and the results do not fully satisfy either patients or surgeons. According to literature data, recurrent hernias occur in 10% of cases with simple forms, and in 30% - with complex ones (recurrent, giant, restrained, sliding). Relapses after traditional methods of hernioplasty are in 20%, and recurrences are in 35-40% of patients. Over the past 40 years, about 50 new methods of hernia repair have been proposed, and the total number of methods and modifications for eliminating inguinal hernias has approached 300 [2]. This testifies to the ongoing search for new, more effective methods of surgery and treatment.Today, the variety of methods for eliminating inguinal hernias can be grouped into two fundamentally different methods: plasty with local tissues and "tension-free" with the use of mesh endoprostheses. Each method has its own advantages and disadvantages. At the present stage, endolaparoscopic hernioplasty is widely introduced into practice. The disadvantages of this method are the complexity of the technique, the high cost of equipment and consumables, a large number of contraindications, the possibility of rare but very dangerous complications [2,11].The number of relapses after endoscopy reaches 15-20%. Despite the enthusiasm for endovideosurgery, the bulk of the interventions will be performed extraperitoneally for a long time, therefore, the issue of widespread use of laparoscopic hernioplasty for inguinal hernias requires further analysis of the effectiveness and viability of this technique [9].The increased claims to the assessment of the postoperative rehabilitation of patients from the standpoint of the quality of life force to reconsider the requirements for the proposed methods. The success of surgical treatment of patients with inguinal hernias, especially in recurrent and complex forms with altered ratios of the layers of the abdominal wall and inguinal canal, can be ensured by reliable strengthening of the posterior wall. The development and introduction into surgical practice of more effective methods of treatment and prevention of the development of recurrent forms of inguinal hernias determines the relevance of the chosen topic.
2. Objective of the Study
- To increase the efficiency of surgical treatment of inguinal hernias by improving the technology of strengthening both walls of the inguinal canal.
3. Materials and Research Methods
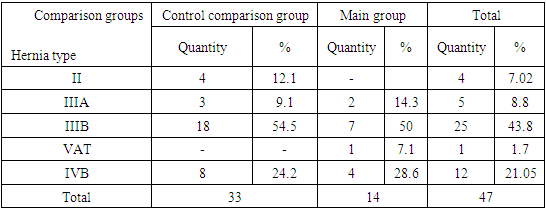
- The study is based on the results of surgical treatment of 47 patients who underwent hernioalloplasty for an inguinal hernia in the surgical department of the clinic of the Samarkand State Medical Institute in the period from 2015 to 2019. To study the effectiveness of the proposed method of inguinal hernia repair, we compared the results of treatment in both groups. The first group of control comparison included 33 (70.2%) hernioalloplasty, produced by the conventional Liechtenstein method. In 14 (29.8%) cases, we used the technique we developed for alloplasty of inguinal hernias and combined these observations into the second main group.In both groups of patients, men were predominant (control group - 94.6%, main group - 91.2%) over fifty years (control group - 76.7%, main group - 80.4%).Table 1 shows the characteristics of patients depending on the type of hernia according to the classification of LM Nyhus (1993). Oblique hernias with a widened displaced inner inguinal ring without protrusion of the posterior wall of the inguinal canal (type II) were observed in 4 (7.02%) patients in the control group. Direct hernias (type IIIA) were detected in 5 (8.8%) patients. Oblique hernias with a large dilated internal inguinal ring (type IIIB) were observed in 25 (43.8%) patients. In 13 (22.8%) cases, recurrent inguinal hernias were detected (type IVA - straight, type IVB - oblique) [1].
|
4. Research Results
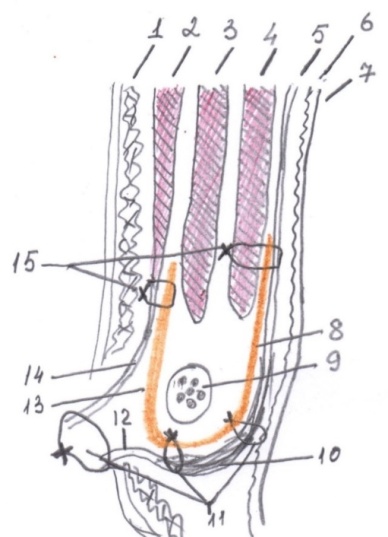
- Of the 47 performed hernioalloplasty in 14 (29.8%) cases (the main group), we used the modified method of hernioalloplasty of inguinal hernias. In these patients, after a conventional skin incision, the aponeurosis of the external oblique abdominal muscle was dissected. Highly isolated and removed the hernial sac. Then followed the isolation of the spermatic cord along its entire length. The transverse fascia was exposed at the inner opening of the inguinal canal. The mesh graft 10 × 15 cm was opened intraoperatively, taking into account individual characteristics. The lower edge of the transverse abdominal muscles was sutured without tension with a 3.0 Prolene suture with the upper inner part of the graft to the transverse fascia. Then the lower edge of the graft was sewn to the pipartligament with interrupted sutures to a point located 2 cm lateral to the inner inguinal ring. Further, in the projection of the center of the inner inguinal ring, a graft was taken into the fold with a clamp and a hole 7-8 mm in diameter was cut out with scissors. The graft was dissected from it vertically upwards. The spermatic cord was placed through the incision into the prepared hole. This achieved an extremely accurate comparison of the exit site of the spermatic cord and the window in the graft. The medial edge of the graft was fixed with a continuous suture to the aponeurosis of the rectus abdominis muscle. Then, with the same thread, the upper edge of the mesh was fixed from the inside with a U-shaped suture to the aponeurosis of the external oblique abdominal muscle. After the final straightening of the mesh, the excess lateral flap was excised. The aponeurosis of the external oblique muscle of the abdomen was sutured edge to edge. The operation was completed by suturing the subcutaneous tissue and continuous intradermal suture. Sutures were applied to the skin (Fig. 1).
5. Conclusions
- Thus, the presented technique of reconstruction of the inguinal canal, aimed at reducing trauma and shortening the time of intervention, can be used in wide practice.This method is more reliable due to the following circumstances: 1. The implant is located under the muscles, but adjacent to the aponeurosis. With this option, firstly, intra - abdominal pressure is evenly distributed over all fixation points and there is less likelihood of tearing the mesh from the tissue, and secondly, when the mesh is fixed to the aponeurosis, the tissue reaction develops less, with the formation of a long-term persistent seroma.2. The method is universal, i.e. can be used for both oblique and direct inguinal hernias.3. Here, to a much lesser extent, the topographic and anatomical relationships in the groin area are disturbed, and in conditions of hernia repair with recurrent and multiple recurrent hernias, these relationships are restored. 4. The method is less traumatic, simple and, most importantly, pathogenetically justified.Conflict of interest. The authors declare no conflicts of interest or special funding for the current study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML