-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 99-102
doi:10.5923/j.ajmms.20231302.15
Received: Jan. 12, 2023; Accepted: Feb. 9, 2023; Published: Feb. 15, 2023

Determining the Neurosurgical Indication for Decompressive Laminectomy in Compression Fractures of the Thoracic and Lumbar Vertebrae in Elderly Patients
Shavkatbek Kholikov1, Norov Abdurakhmon2
1Andijan State Medical Institute
2Bukhara Regional Multi-Network Medical Center
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Complications such as persistent pain syndrome and worsening of neurological changes after surgery for compression fractures in the thoracic and lumbar spine are one of the urgent problems of modern neurosurgery, traumatology and vertebrology. The aim of the research: to determine neurosurgical indications for decompressive laminectomy manipulation in compression fractures of the thoracic and lumbar vertebrae in older and elderly patients. Source and research methods: Clinical materials were collected from 2012-2021, the main group consisted of 41 elderly patients (18 men, 23 women, mean age 64.07±0.99 years) and the control group consisted of 59 middle-aged patients (34 1 male, 25 female, average age 51.58±0.47 years). Patients in the study underwent percutaneous vertebroplasty, transpedicular fixation, combined method (vertebroplasty and transpedicular fixation together) and decompressive laminectomy manipulation. Result and discussion: 1 year after surgery in the main group, 33 (80.5%) patients had excellent results, 8 (19.5%) patients had good results. In the control group, 1 year after surgery, 49 (83%) patients had excellent results and 10 (17%) patients had good results. Conclusion: In case of compression fractures in the area of thoracic and lumbar vertebrae in elderly and elderly patients, it is advisable to determine the degree of relative stenosis of the spinal canal in the area where the vertebro-medullary conflict is located, and perform decompressive laminectomy manipulation.
Keywords: Spinal canal stenosis, Vertebro-medullary conflict, Decompressive laminectomy
Cite this paper: Shavkatbek Kholikov, Norov Abdurakhmon, Determining the Neurosurgical Indication for Decompressive Laminectomy in Compression Fractures of the Thoracic and Lumbar Vertebrae in Elderly Patients, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 99-102. doi: 10.5923/j.ajmms.20231302.15.
1. Introduction
- Closed injuries of the spine make up an average of 3.3% of all injuries to the human body, and are one of the most common pathological conditions in traumatology and neurosurgery practice. 55-94% of these injuries occur in the area of the lower thoracic and lumbar vertebrae, and in 85% of cases, compression and distraction type occur [1]. Compression fractures of the thoracic and lumbar vertebrae in elderly patients are primarily caused by osteoporosis [5] and aggressive hemangiomas [8]. Although neurological changes do not develop in the injuries that occur, the pathology of biomechanical instability of the spine develops, and as a result, migration of bone fragments and an increase in the angle of kyphotic deformation are observed. In this case, distribution of static and dynamic loads falling on the front part of the spine is disturbed, displacement of the intervertebral disc and bone fragments into the spinal canal is observed. As a result of the above pathology, neurological disorders develop due to compression of the spinal cord and nerve roots, secondary CSF-hemodynamic disorder occurs due to compression of the dural membrane and venous entanglements. In the past, conservative treatment of uncomplicated compression fractures in the thoracic and lumbar regions was recommended, in which strict bed rest and orthopedic regimen and partial analgesics were recommended. The disadvantage of conservative treatment is the low rate of long-term bed rest and complete consolidation of the fracture. Development of kyphotic deformity causes pathological conditions such as instability syndrome, neurological changes or vertebrogenic pain syndrome in 57-70% of cases. Due to the shortcomings of conservative treatment, it is recommended to eliminate compression fractures in the area of the thoracic and lumbar vertebrae by surgical stabilization of the spine [2,3]. In compression fractures of the thoracic and lumbar vertebrae, after the reconstruction of the spinal canal, the need for reliable immobilization of the vertebral-movement segment, consolidation of the fracture, and the selection of the optimal surgical method of treatment aimed at restoring the anatomical shape of the fractured vertebral body are of great importance [4,8,9]. Currently, the pathogenesis of compression-ischemic myelopathy in kyphotic deformations is interpreted as follows. The dural sac with its contents moves to the bent side due to deformation, to the attachment points of the dura mater (large foramen of the neck and hump). In this case, the dural bag tightly presses the upper areas and crushes the anterior side. The dura mater of the brain is firmly attached to the skull and the skull, and is considered to have low mobility and inelastic properties. During the flexion of the spine, the tension of the dura mater increases, in the process of returning to its original state, it stretches even more, mainly when kyphosis develops, and the spinal cord spreads along the anterior wall of the spinal canal and crushes it. The second pathogenetic mechanism is the increased deformation of the vertebral column due to the tension of the spinal cord in the axial formation, which occurs due to the inability of the dural sac to move ventrally [6]. According to the interpretation of the literature, revision and decompression of the spinal canal in kyphotic deformations of the thoracic and lumbar vertebrae is performed not only in patients with severe neurological changes, but also in cases where the stenosis of the spinal canal has exceeded the limit and neurological symptoms have not developed. Currently, there are various methods to determine the degree of stenosis of the spinal canal.In conclusion, prevention of complications such as persistence of pain syndrome and worsening of neurological changes in patients after surgical procedures remains one of the urgent problems facing neurosurgeons, traumatologists and vertebrologists.
2. Source and Research Methods
- In our study, a total of 100 middle-aged people who underwent surgery for compression fractures in the thoracic and lumbar regions of the spine at the neurosurgery department of the Republican Scientific and Practical Medical Center of Narcology, at the neurosurgery department of the Andijan branch of the Republican Emergency Medical Center, and at the neurosurgery and vertebrology departments of the Andijan State Medical Institute clinic, area, degree, clinical-neurological symptoms and treatment results of compression fractures in older and elderly patients were studied. Clinical materials were collected from 2012-2021, the main group consisted of 41 older and elderly patients (18 men, 23 women, mean age 64.07±0.99 years) and the control group consisted of 59 middle-aged patients (34 men, 25 women, average age 51.58±0.47 years).In the control and all patients of the main group who participated in the study, according to the current relevant diagnostic and treatment standards of SSV, general clinical (general blood and urine analysis, biochemical analysis of blood, ECG, ExoKG with instructions, chest X-ray, UTT), special (spine X-ray, CT, MSCT, MRT) and functional tests were used.Decompressive laminectomy manipulation was carried out by determining the degree of relative stenosis of the spinal canal in the area where the vertebro-medullary conflict is located in the spinal canal in case of compression fractures of the thoracic and lumbar vertebrae in elderly and elderly patients.
3. Result and Discussion
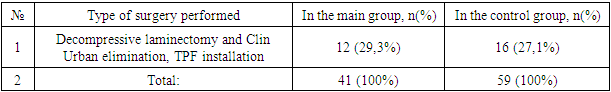
- The AOSpine classification (The AO Spine Thoracolumbar Spine Injury Classification System, 2013) was used to assess the type of compression fractures in the control groups. In our study, according to this classification, groups A0 to A4 were studied, and type V and C fractures were not included in the investigation.In the surgical treatment of compression fractures in the area of the thoracic and lumbar vertebrae of elderly and elderly patients, such methods as vertebroplasty of the compressed area, kyphoplasty, installation of posterior spondylodesis TPF and combined method (joint application of vertebroplasty and TPF) are used. The surgical method of treatment was selected according to the type of compression fractures of the thoracic and lumbar vertebrae in the patients who participated in the investigation according to the AO Spine classification (see diagram 1).
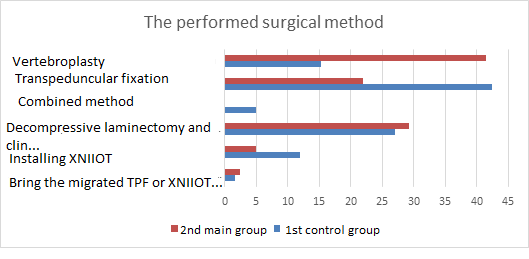 | Diagram 1. Surgical methods performed in the main and control groups |
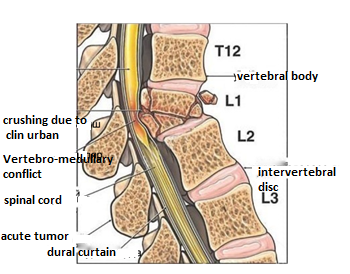 | Figure 1. Occurrence of vertebro-medullary conflict due to compression fracture of the VL1 vertebra |
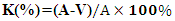 In this formula: K is the relative size of the stenosis; A – sagittal dimension of the neutral part of the subarachnoid space; V – the sagittal dimension of the maximum crushed part of the subarachnoid space;The level of central stenosis of the spinal canal and the degree of vertebro-medullary discord determined by the MSCT or MRI examination of compression fractures in the thoracic and lumbar regions of the spine have been proven to be a neurosurgical indication for decompressive laminectomy and clinical Urban elimination manipulation. During surgery, in addition to the two methods used (TPF device installation and combined method), we eliminated the spinal cord or nerve root compression factor by decompressive laminectomy and clinical Urban elimination manipulation, and achieved the prevention of the above complications (see Figure 2).
In this formula: K is the relative size of the stenosis; A – sagittal dimension of the neutral part of the subarachnoid space; V – the sagittal dimension of the maximum crushed part of the subarachnoid space;The level of central stenosis of the spinal canal and the degree of vertebro-medullary discord determined by the MSCT or MRI examination of compression fractures in the thoracic and lumbar regions of the spine have been proven to be a neurosurgical indication for decompressive laminectomy and clinical Urban elimination manipulation. During surgery, in addition to the two methods used (TPF device installation and combined method), we eliminated the spinal cord or nerve root compression factor by decompressive laminectomy and clinical Urban elimination manipulation, and achieved the prevention of the above complications (see Figure 2).  | Figure 2. Performing a decompressive laminectomy |
|
4. Conclusions
- It is appropriate to choose surgical methods of treatment of compression fractures in the thoracic and lumbar region depending on the degree of deformation of the compressed vertebral body, the angle of kyphotic deformation, signs of instability in the damaged segment, and the degree of vertebro-medullary conflict in the spinal canal.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML