-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 91-94
doi:10.5923/j.ajmms.20231302.13
Received: Jan. 6, 2023; Accepted: Feb. 10, 2023; Published: Feb. 15, 2023

Comparative Analysis Treatment of the Use Halo Vest for Odontoid Fractures
Ortiksher I. Quziev
Department of Emergency Neurosurgery Fergana Branch Republican Research Centre of Emergency Medicine, Fergana, Uzbekistan
Correspondence to: Ortiksher I. Quziev, Department of Emergency Neurosurgery Fergana Branch Republican Research Centre of Emergency Medicine, Fergana, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The problems of providing adequate care to patients with injuries of the upper cervical vertebrae are still relevant and far from a final solution. This is indicated by the divergence of views on the choice of treatment tactics for individual specialists. The main task in their treatment is the prevention of secondary displacements, the elimination of deformities, if possible, and the provision of reliable stabilization of the vertebrae [9,11,12].
Keywords: Traumatic injuries, Patients, Women, Craniovertebral, Neck Stabilization, Atlantoaxial complex, Cervical spine
Cite this paper: Ortiksher I. Quziev, Comparative Analysis Treatment of the Use Halo Vest for Odontoid Fractures, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 91-94. doi: 10.5923/j.ajmms.20231302.13.
Article Outline
1. Introduction
- It is well known that the Halo vest was first described by Perry and Nickel in 1959 and has been widely used in the treatment of traumatic injuries of the upper cervical vertebrae. According to some authors, the Halo vest provides the greatest immobilization among all external fixators. There have also been cases of complications and a high incidence of non-union of bone fragments [3-6]. Cases of nonunions can be associated with various factors, including excessive movement of the injured vertebra during daily activities. Traditionally, the effectiveness of the Neck Stabilization Halo vest has been assessed using cadaver models [15-21] and mannequins. In these studies, neck movement in the Halo vest was measured with head loading while the torso remained stationary. Based on this, we were faced with the task of improving the methods of treatment and the fixing structure.
2. Purpose of the Study
- To conduct a morphometric analysis in patients who used the Halo vest and the apparatus developed by us for external correction and fixation of the cervical spine (Halo vest with an arch support).
3. Materials and Methods
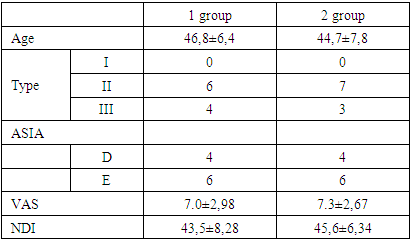
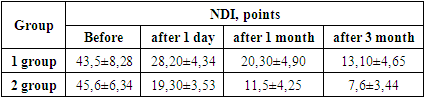
- The analysis of the results of treatment of 20 patients with fractures of the odontoid process of the axis for the period from 2015 to 2021 was carried out in the Department of Emergency Neurosurgery Fergana Branch Republican Research Centre of Emergency Medicine. Of these, men - 16 (80.0%) patients, women - 4 (20.0%) patients. The age ranged from 18 to 72 years, the average age was 31 (±14.5) years. According to the mechanism of injury, road accidents prevailed - 15 (75%) cases, less often - falling from a height - 3 (15.0%) and diving in shallow water - 2 (10.0%). The patients were divided into two groups: the 1st group - 10 patients who used the Halo-vest, and the 2nd group - 10 patients who used the apparatus developed by us for external correction and fixation of the cervical spine (Fig. 1.). The distribution of patients is presented in Table 1.
|
 | Figure 1. Position of the patient using the Halo vest with an arch support and lateral radiography of the cervical spine |
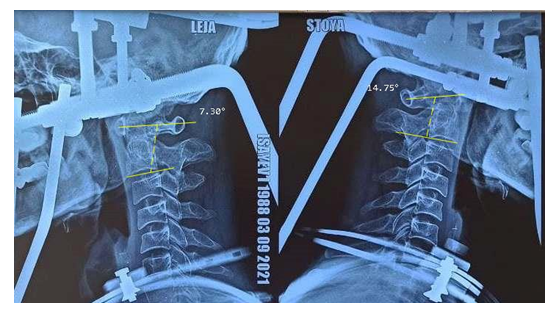 | Figure 2. Measurement of the segmental angle C1 - C2 on lateral radiographs of the cervical spine |
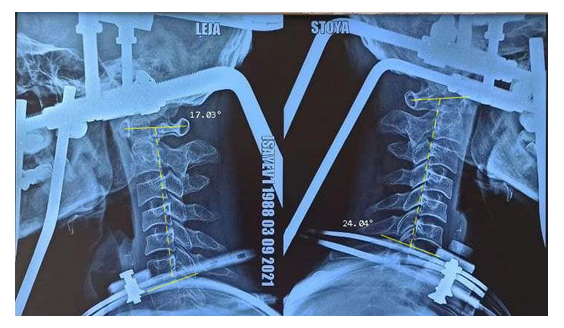 | Figure 3. Measurement of the segmental angle C1 - C7 on lateral radiographs of the cervical spine |
4. Results
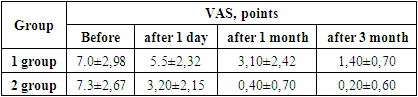
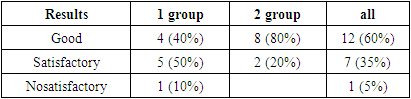
- Cervicalgia syndrome in both groups of patients before treatment was the same within an average of 7.20 - 7.60 points on the VAS scale. The table presents a comparative analysis of pain intensity among groups before and after treatment. In all groups, the VAS pain score decreased after treatment. In group 1 and group 2, the intensity of the pain syndrome is the lowest - 1.50 and 1.05, respectively. The highest intensity of pain syndrome after treatment remained in the control group, which used a hard trench collar. After the injury and before the operation, the intensity of pain on a 10-point VAS scale ranged from 2 to 10 points, on average 6.2 points, immediately after surgery - from 1 to 8 points, on average 6 points, after 1 month - from 0 to 6 points, an average of 2.2 points, after 6 months - from 0 to 3 points, an average of 0.33 points (Table 2).
|
|
|
|
5. Discussion
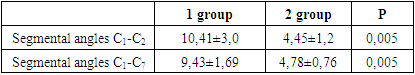
- Clinical studies by several authors have documented changes in cervical lordosis and excessive intervertebral rotation in patients with the Halo vest in prone and supine positions [1,10,13,14]. Curvature of the cervical spine, defined as counter-rotation throughout the cervical spine, is thought to be due to the movement of the torso during the transition from vertical to horizontal and back [1,13]. In the present study, neck movements in the sitting and lying position were determined and compared between wearing the Halo Vest with arch support and the conventional Halo Apparatus. Our results demonstrated an S-shaped curvature due to the Halo Vest, consisting of extension at the upper cervical spine and flexion at the lower spine. In the prone position, there was significantly greater head/C1 extension and C1/2 and C1-7 flexion in patients using the Halo apparatus compared to the Halo apparatus with an arch support. An axial separation of the head and vC7 was observed due to the Halo, which is consistent with the tensile loading that has been observed clinically in Halo patients [1,10,13]. Our model has limitations that should be taken into account. The patient was transferred from a prone position to a vertical position, to a supine position, and neck movements were determined using a halo vest. This protocol was chosen in order to be able to calculate the range of motion of the neck during these simulated activities in daily life. In the future, this work will help investigate the effectiveness of the halo vest in stabilizing the neck during body movements [3]. A halo vest is often used as an alternative to internal fixation to treat patients with type II odontoid fracture or stable Jefferson, facet, or compression fractures. Previous clinical studies have documented up to 10° of total C1/2 range of motion in patients treated with the Halo Machine while performing daily activities [5,10,13]. Patients with a VC2 fracture were treated with the Halo vest and suggested that more than 5° of fracture site displacement may indicate an increased risk of nonunion. Our results showed that the Halo Vest effectively immobilized mean peak C1/2 rotation to less than 4.45° in both the sitting and supine positions. In contrast, the conventional Halo apparatus produced an average peak C1/2 stretch of 10.47° in the supine position. The halo apparatus produced a significant increase in rotation beyond the physiological range in the prone position, in head/C1 extension, and in C4/5 and C7-T1 flexion. These results indicate that an improperly fitted or loose vest can reduce its immobilization capacity, resulting in delayed healing or non-union. The existing patterns of movement of the cervical spine due to the halo vest help us understand its immobilization capabilities and may be helpful to clinicians in choosing the optimal treatment based on the classification, anatomical location, and severity of the neck injury. Our results highlight the importance of monitoring and tightening the vest straps as needed, especially in those who lose weight or chest circumference during halo vest treatment. The results may also be useful to biomechanical engineers to improve the design of the Halo vest to reduce neck tortuous movement in the prone and prone positions.
6. Conclusions
- The modified apparatus for external correction and fixation of the cervical spine proved to be effective in eliminating displacements of bone fragments, restoring anatomical relationships in the craniovertebral region with simultaneous fixation of the cervical vertebrae, which allows early activation and rehabilitation of the victims. In addition, the apparatus proposed by us is more comfortable for patients compared to the classical Halo vest, as it allows them to take horizontal postures.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML