-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 87-90
doi:10.5923/j.ajmms.20231302.12
Received: Jan. 19, 2023; Accepted: Feb. 3, 2023; Published: Feb. 13, 2023

The Significance of Transcutanic Oximetry in Determining the Tactics of Treatment of Distal Foot Gangrene in Patients with Diabetes Mellitus
К. J. Matmurotov, P. Yu. Ruzmatov, T. Sh. Atajanov, B. A. Ruzmetov, I. Yu. Yakubov
Department of General Surgery, Tashkent Medical Academy, Farobi 2, Almazar District, Tashkent, Uzbekistan
Correspondence to: К. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Farobi 2, Almazar District, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

At present, research is ongoing in the world to improve the results of surgical treatment of patients with gangrene of the lower extremities on the background of diabetes mellitus, which is associated with the steady growth of this contingent of patients with bleeds, the ambiguity of approaches in matters of surgical tactics and unsatisfactory results of treatment. The analysis of the literature data indicates that today there are a number of unresolved issues of surgical tactics for purulent-necrotic lesions of the feet of various localization, in particular, staging or simultaneity depending on the affected area of the foot, clear indications for combined minimally invasive endovascular interventions with a combination of infectious process and limb ischemia, which in general should be aimed at improving the treatment and diagnostic algorithm in the treatment of patients with gangrene of the lower extremities against the background of diabetes. The results of treatment of 126 patients with critical ischemia of the lower extremities on the background of diabetes mellitus were analyzed; after the final diagnosis and localization of the affected segment, all patients underwent transluminal balloon angioplasty of the arteries of the lower extremities.
Keywords: Diabetes mellitus, Diabetic foot syndrome, Gangrene
Cite this paper: К. J. Matmurotov, P. Yu. Ruzmatov, T. Sh. Atajanov, B. A. Ruzmetov, I. Yu. Yakubov, The Significance of Transcutanic Oximetry in Determining the Tactics of Treatment of Distal Foot Gangrene in Patients with Diabetes Mellitus, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 87-90. doi: 10.5923/j.ajmms.20231302.12.
Article Outline
1. Introduction
- Currently, in modern surgery, the criteria and methods for diagnosing critical lower limb ischemia (CLLI) in patients with diabetes mellitus (DM) include comprehensive assessment of symptoms and signs of peripheral arterial disease (PAD), as well as an objective instrumental examination. According to the International Consensus on the Diabetic Foot (2015), CLLI is characterized by one of the followings two criteria: 1) persistent pain at rest requiring regular analgesics for two weeks or more and/or 2) trophic ulcer or gangrene of fingers’ or foot, which arose against the background of chronic arterial insufficiency [1,7,11]. Routine non-invasive methods for assessing the severity of ischemic limb damage are the measurement of the ankle and finger pressure with the assessment of ankle-brachial index (ABI) and the finger-brachial index (TBI), respectively, and transcutaneous oximetry [2,3,14]. In this case, CINC is defined as systolic pressure in the arteries ofthe lower leg below 50–70 mm Hg. Art., and at the level of afinger - below 30-50 mm Hg. Art. [4,5,9]. The use of these tests plays an important role at the stage of primary diagnosis of peripheral arterial diseases, but hasa number of significant limitations. According to our data, the measurement of ankle pressure in patients with CLLI against the background of diabetes mellitus is in many cases not very informative due to the presence of mediacalcinosis,as well as in the case of occlusion of both arteries - the posterior tibial artery (PTA) and dorsal artery offoot (DAF), are commonly used to measure ABI [6,8,15].With severe calcification of thevascular wall in patients with DM, renal failure and severe peripheral neuropathy,decrease in elastic properties and stiffness of arteries can spread to the digital arteries, which leads to unreliable study results. Often, in patients with DM with trophic changes in the distal foot, or due to small amputations, it is impossible to measure digital systolic pressure [4,16]. In patients with severe chronic complications of DM, for an objective assessment ofCLLI severity, it is extremely important to study microcirculation and tissue metabolism disorders using transcutaneous oximetry [3,9].The advantages of transcutaneous oximetry indiagnosis of CLLI compared to other routine methods arethat it does not depend onseverity of peripheral arterial mediacalcinosis and is more informative among patients with DM, the possibility of determining the level of limb amputation and ulcer healing prognosis [10]. Measurement of oxygen partial pressure for the purpose of primary diagnosis of limb ischemia in patients with DM and dynamic assessment of blood flow after the intervention does not require special training of a specialist and is easily implemented at the primary level. The threshold value for diagnosing critical limb ischemia is 30 mm Hg of oxygen tension (TcpO2). Art. The high cost of equipment, maintenance costs and consumables are factors limiting its widespread use [12]. At the same time, the question of the information content of method in the presence of infectious inflammation on the foot remains open, peripheral edema and other concomitant pathological conditions that affect the results of thestudy [2,11,13].In this regard, the purpose of our study was to evaluate the significance of transcutaneous oximetry (TcpO2) in the diagnosis and follow-up of patients with critical lower limb ischemia associated with diabetes after percutaneous transluminal balloon angioplasty (PTBA).
2. Materials and Methods
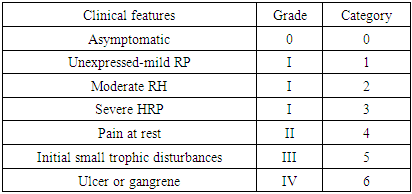
- The treatment resultsof 126 patients (148 limbs) with CLLI against the background of diabetes mellitus, who received inpatient treatment in the Department of Purulent Surgery and Surgical Complications of Diabetes Mellitus at the multidisciplinary clinic ofTashkent Medical Academy from 2020 to 2022, were analyzed. All patients underwent transluminal balloon angioplasty (TLBAP) of arteries of the lower extremities after establishing the final diagnosis and localization of theaffected segment.22 patients (17.5%) underwent surgery on two lower limbs, 104 patients (82.5%) on one limb. All patients were diagnosed with chronic arterial insufficiency at the stage of critical ischemia of the affected limb according to TASC II criteria [2]. In the presence of specific signs of limb ischemia, asymmetry or absence of pulsation in the arteries of the foot, physiological tests and transcutaneous oximetry were used. Measurements of ABI were carried out with the patient lying on his back after a 10-minute rest. The ABI was calculated as the ratio of the highest systolic pressure on the PBA or TAS to the highest systolic pressure on thebrachial artery of the right or left upper limb.The evaluation of the measurement results was carried out according to modern recommendations. The main instrumental method for assessing the state of macrocirculation was ultrasound duplex scanning of thelower extremities, performed on an ultrasound duplex system Acuson-128 XP/10 (Acuson, USA) and multislice computed tomography of the arteries of the lower extremities (MSCT). MSCT was performed in all patients, which determined the level of stenosis and occlusion of arteries, degree of narrowing of the artery, the extent of alesion, andexact location of atherosclerotic plaques.The severity of peripheral arterial disease (PAD) was assessed according to Rutherford classification (Table 1.). In the postoperative period, ultrasound examination of lower extremityarteries was carried out in order to assess their patency, verify morphological and clinical restenoses. TLBAP was considered technically successful in restoring continuous antegrade blood flow to the foot of at least one leg artery without residual stenoses of more than 50%.In the presence of purulent-necrotic lesions, patients undergo the multi-stage surgical operations on the foot, local wound treatment, antibiotic therapy and regulation of metabolic disorders. The study of transcutaneous oximetry was carried out before TLBAP, then on days 5–7 after the intervention, after 1, 3 and 6 months of observation. A transcutaneous oximeter (Radiometer Copenhagen) was used to assess TcpO2.Measurement of TcpO2 was carried out on the skin of the dorsum of the foot with a uniform capillary bed without large arteries and veins, ulcers or hairline. The patient during the study was in a supine position in a calm and relaxed psycho-emotional state. The temperature in the room where the study was conducted was 21–23°C. Before the start ofthe study, theelectrode was calibrated with atmospheric air.The electrode was installed in a fixed ring on the skin after pre-treatment with an alcohol solution. The cavity of the fixed ring was preliminarily filled with an electrolyte solution (2–3 drops). Then a sensor was installed fixed ring on the skin. Registration of TcpO2 indicators after sensors were placed on the skin was carried out when they stabilized after 15–20 minutes andskin temperature reached 43°C.
3. Results and Discussion
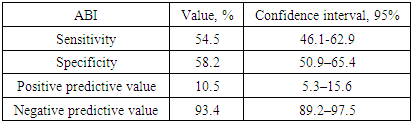
- The number of operated patients was 126, of which 89 (70.6%) were men and 37 (29.4%) were women. The mean age of the patients was 64.4±10.1 years. Type 1 diabetes was diagnosed in 2 (1.6%) patients, type 2 diabetes in 124 (98.4%). The state of carbohydrate metabolism indicated a pronounced decompensation of DM according to the average level of glycated hemoglobin (8.0±1.3%). More than half of the patients had a severe form of neuroischemic form of diabetic foot syndrome (DFS) - 77 (61.1%). 48 (38%) patients were obese (body mass index (BMI) >30 kg/m2). Of the concomitant cardiovascular diseases, 26 (21%) patients had a history of acute myocardial infarction (AMI), 25 (20%) had an acute cerebrovascular accident (ACV), respectively. Most patients were diagnosed with severe microvascular complications of DM.Diabetic preproliferative and proliferative retinopathy was detected in 39 (31%) patients. Chronic kidney disease (CKD) was present in 75 (60%) patients, of which 43 (34%) had a glomerular filtration rate (GFR) <60 ml/min/1.73 m2. Replacement therapy with program hemodialysis was received by 3 (2.3%) patients, and donor kidney transplantation was previously performed on 1 (0.8%) patients.When using the criteria for the correspondence of the severity of critical ischemia to the ABI values proposed by the American Heart Association [10], it was found that in 32 (25.4%) patients the ABI values corresponded to normal or were increased, while in 89% of the examined patients it was established diagnosis of KINK.At the same time, ABI values < 0.6, corresponding to severe limb ischemia, were registered only in 49 (38.8%) patients. In 9 (7.1%) patients, systolic pressure was not measured. In the structure of PAD severity, according to the Rutherford classification, patients with CLLI and foot ulcers predominated. Thus, 108 (85.7%) patients had long-term non-healing wound defects on the foot, often complicated by infection, as well as gangrene of one or more fingers.Thus, the first appeal for medical help occurred in such patients already at the terminal stage of critical ischemia, when there was a real threat of high limb amputation. 14 (11.1%) patients were diagnosed with severe intermittent claudication (IC) - category 3 lesions according to Rutherford (Table 1), and 12 (9.5%) patients complained of severe pain at rest - 4th degree of ischemia, respectively.
|
|
|
4. Discussion
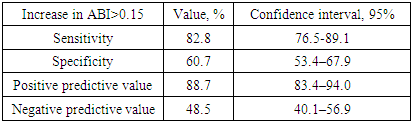
- Most patients with CLLI, chronic renal failure, severe peripheral polyneuropathy, and concomitant mediacalcinosis had normal or high ankle pressure values, and a moderate decrease in ABI did not reflect the severity of PAD. On the other hand, the measurement of ABI in patients with CLLI has shown its importance in evaluating the effectiveness of endovascular intervention. In cases where it was possible to measure systolic pressure in the arteries of the lower leg, a clinically significant improvement in blood flow after revascularization of the limb was accompanied by an increase in ABI of at least 0.15 from the initial value.After revascularization of the limb in aperiod of dynamic follow-up, our study noted a high incidence of restenosis in the treated arterial segments, which was detected during ultrasound. A comprehensive examination of patients, including transcutaneous oximetry, in the vast majority of cases excluded the recurrence of clinical manifestations of CLLI. Thus, the lack of patency of the main arteries of the lower extremities after TLBAP was most often associated with morphological restenoses. A slight increase in the number of clinical relapses of CLLI is explained by timely repeated endovascular interventions.Thus, it is important to note that the main goal of endovascular intervention was the healing of trophic ulcers and postoperative wounds in patients with diabetic foot syndrome, thus avoiding major amputations. In the future, a decrease in TsrO2 values below the threshold value, due to the development of restenoses in arteries of the lower extremities, was not the main indication for re-intervention in the absence of trophic disorders. When deciding whether to repeat TLBAP, a combination of clinical signs and symptoms of CLLI, concomitant complications of the underlying disease, as well as data from objective methods for assessing peripheral blood flow were taken into account.
5. Findings
- 1. The method of transcutaneous oximetry allows assessing the severity of CLLI in patients with DM, as well as predicting the effectiveness of the planned TLBAP, followed bychoice of tactics for minor surgical interventions on the foot.2. Topical diagnosis of occlusive lesions of the peripheral arteries of the lower extremities is important for assessing percutaneous oxygen tension in patients with CLLI against the background of DM: the level of TcO2 at the dorsal foot at rest is determined to a greater extent by the patency of PTA and DAF.3. Measurement of oxygen tension (TcpO2) after endovascular intervention is one of the important informative diagnostic methods for dynamic clinical monitoring of patients, timely re-endovascular intervention and choice of surgical tactics.
Consent
- It is not applicable.
Ethical Approval
- It is not applicable.
Competing Interests
- Authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML