-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 81-86
doi:10.5923/j.ajmms.20231302.11
Received: Jan. 19, 2023; Accepted: Feb. 3, 2023; Published: Feb. 13, 2023

Leg Amputations: A Differentiated Approach to Performance Depending on the Lesion of the Arterial Basin
К. J. Matmurotov, I. S. Sattarov, P. Yu. Ruzmatov, D. D. Rahimov, I. Yu. Yakubov
Department of General Surgery, Tashkent Medical Academy, Farobi 2, Almazar District, Tashkent, Uzbekistan
Correspondence to: К. J. Matmurotov, Department of General Surgery, Tashkent Medical Academy, Farobi 2, Almazar District, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study is aimed at improving the results of amputations at the level of the lower leg, taking into account the affected part of the foot (angiosomes) and the appearance of the primary pathological focus. This paper presents an analysis of the results of examination and treatment of 73 patients with gangrene of the lower extremities on the background of diabetes mellitus. The patients were hospitalized in 2018-2021. in the center of the department of purulent surgery at the multidisciplinary clinic of the Tashkent Medical Academy. The main instrumental research method was multislice computed tomography of the arteries of the lower extremities (MSCT) and duplex scanning of the arteries of the lower extremities, which provided final information about the state of the peripheral arterial bed. All patients underwent amputation of the lower leg at the level of the upper third by a new differentiated method.
Keywords: Diabetes mellitus, Diabetic foot syndrome, Gangrene
Cite this paper: К. J. Matmurotov, I. S. Sattarov, P. Yu. Ruzmatov, D. D. Rahimov, I. Yu. Yakubov, Leg Amputations: A Differentiated Approach to Performance Depending on the Lesion of the Arterial Basin, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 81-86. doi: 10.5923/j.ajmms.20231302.11.
Article Outline
1. Introduction
- Diabetes mellitus (DM) is by far the most common endocrine disease. According to the IDF Diabetes Atlas, there will be 537 million patients with diabetes in the world by 2021, and according to preliminary forecasts, 1 billion people will suffer from diabetes by 2045 [1]. According to statistics, by 2018, 2,982,865 patients with DM were registered in our country [6].Diabetic foot syndrome (DFS), which manifests itself as the development of purulent-necrotic lesions in the lower extremities, is considered one of the most severe complications of DM, leading to surgical manipulations. Diabetic foot syndrome develops on average in 35-60% of diabetic patients [3]. In foreign epidemiological studies, the number of DFS occurs from 30% to 80% of the total number of patients with type 2 Diabetes Mellitus [4]. Late admission of patients with purulent-necrotic lesions of the feet against the background of DFS in most cases is associated with an asymptomatic course of DM, therefore, approximately 30% of patients upon admission to the hospital already have widespread purulent-necrotic lesions of the foot, up to total gangrene[2,5].The prevalence and appearance of clinical signs of critical ischemia of the lower extremities on the background of diabetes mellitus increases with age: among patients aged 40 years it is about 3%, among patients aged 60 years – 9%. Of interest is the fact that 10 to 50% of patients with diabetic foot syndrome never see a doctor about symptoms, as most develop severe neuropathy. Untimely treatment of patients and treatment of purulent-necrotic lesions of the foot leads to limb loss [6].A comparative analysis of the frequency of surgical interventions showed that high amputations of the lower extremities in patients with DM are performed 17-45 times more often than in people without DM [7]. To select the optimal level of amputation, it is necessary to determine the severity of lower limb ischemia at the expected level of surgical intervention, since a poorly supplied stump becomes necrotic, which is the cause of severe purulent-septic complications [8]. Determining the level at which the blood supply to the stump can provide wound healing and nutrition to the remaining part of the limb is the main difficulty in deciding the level of amputation [9].It is widely believed that an increase in the ratio of below-the-knee amputation to above-the-knee amputation should inevitably lead to a higher failure rate. However, this opinion is not confirmed by a comparative analysis of the results [11]. According to published studies on the rate of late healing and revision after amputation below the knee, the rate of primary healing ranged from 30 to 92% (mean 70-75%), and the frequency of re-amputation - from 4 to 30% (mean 15%). Approximately another 15% of cases had delayed or secondary healing, which in some cases required debridement and further operations, such as wedge excision, in order to preserve the length of the lower limb. Of the 30% of below-the-knee amputees whose wounds do not heal initially, approximately half require re-amputation at a higher level. More blood flow is needed to heal a postoperative wound than to maintain the viability of the skin without surgery. After wound healing with a high amputation below the knee, only 4% of patients subsequently require a higher amputation [12,14].In general, the more often an attempt is made to save the knee, the more often it succeeds. Thus, the use of an aggressive team approach to amputations led to an increase in the ratio of below-the-knee amputation to above-the-knee amputation from an unusually low rate of 0.14 to 2.1 [13]. According to modern standards, amputation at the level of the femur should be performed in cases where the patient has contraindications for performing amputation of the lower leg.The purpose of this study– to improve the results of leg amputations in patients with critical lower limb ischemia (CLLI) on the background of DM.
2. Material and Methods
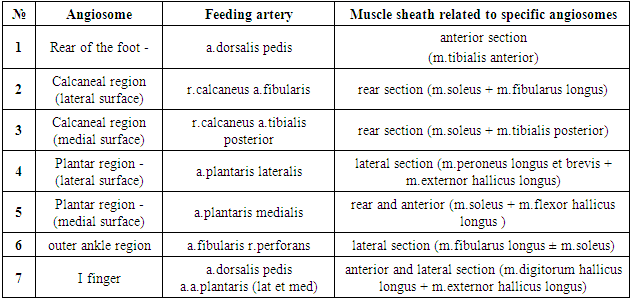
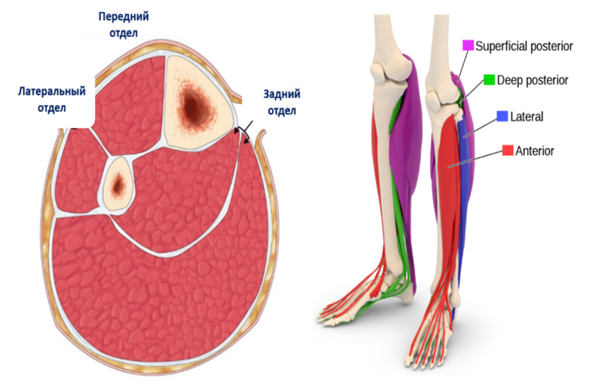
- This study analyzed the results of surgical treatment of 73 patients with gangrene of the lower extremities due to diabetes mellitus, who received inpatient treatment with amputation of the lower leg at the level of the upper third, in the department of purulent surgery and surgical complications of diabetes mellitus at the multidisciplinary clinic of the Tashkent Medical Academy from 2018 to 2021 year.The average duration of diabetes mellitus in patients was 12.5±3.9 years. The age of the patients ranged from 27 to 79 years (average 50.6±5.7 years). The patients included 49 (67.1%) men and 24 (32.9%) women. The neuroischemic form of the diabetic foot syndrome was diagnosed in 52 (71.2%) patients, the ischemic form in 21 (28.8%) patients. The duration of inpatient treatment of patients averaged 4-7 days.15 (20.5%) patients had signs of Ischemic Heart Disease, 6 (8.2%) patients had a past Myocardial Infarction. In 9 (12.3%) patients, Transient Cerebrovascular Accidents occurred, 5 (6.8%) patients suffered an Acute Cerebrovascular Accident in the past. 21 (28.8%) patients had Arterial Hypertension.The instrumental method was ultrasound duplex scanning and the multislice CT of the arteries of the lower extremities. After receiving information about the state of the peripheral arterial bed and the impossibility of restoring blood flow, all patients underwent leg amputation at the level of the upper third. Statistical data processing was carried out using the application software for statistical processing of the database DBASE and STAT4. Statistical methods for estimating differences in mean values using Student's t-test were used for calculations.Today, the angiosomal theory of tissues of the human body is of particular interest to specialists. The term "angiosome" was proposed by Taylor and Palmer in 1987 to refer to vessels that feed certain areas of the human body. Angiosome is an anatomical unit of tissue supplied by a single artery. The essence of the theory is that each anatomical unit of tissues (skin, subcutaneous tissue, fascia, muscles and bones), or angiosome, is supplied with blood within one artery.In total, there are 40 angiosomes in the human body. On the lower leg and foot, 7 angiosomes were identified, while neighboring angiosomes are connected by a collateral network (Fig. 1). Zones were identified for the foot, which are fed by the anterior tibial artery (ATI), posterior tibial artery (PTA), and peroneal artery (PA).
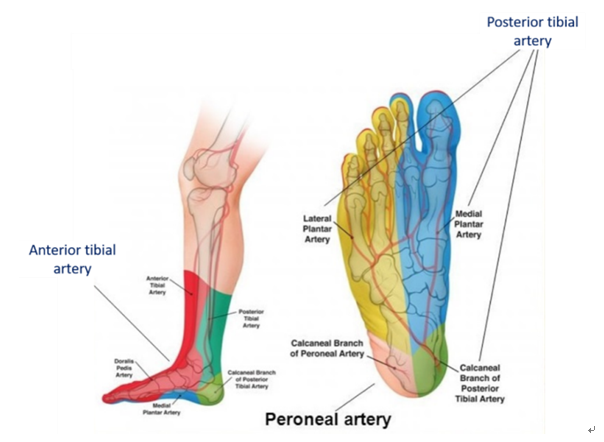 | Figure 1. Angiosomal structure of the foot and blood supply to the arteries |
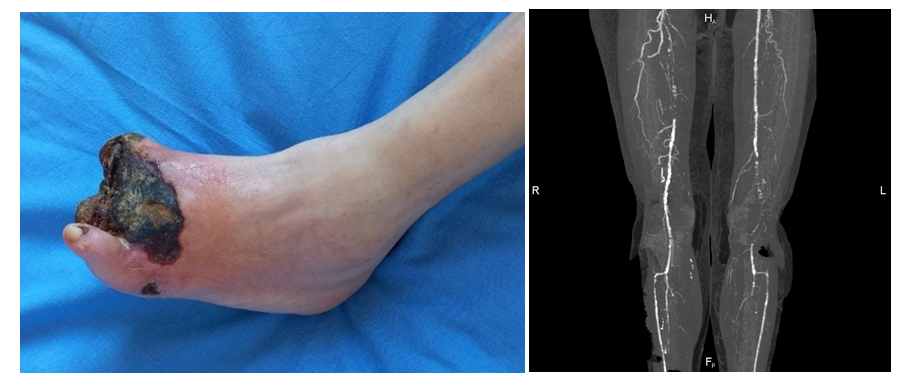
 | Figure 2. Muscular sheaths of the lower leg. |
|
3. Results and Discussion
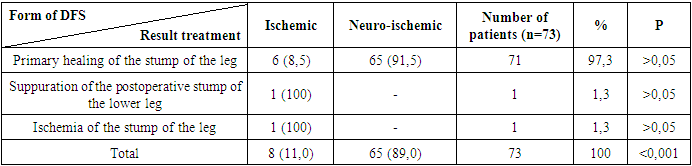
- When analyzing the results of treatment of patients, the primary healing of the postoperative wound of the stump was considered a favorable immediate outcome of amputation. Suppuration, secondary healing, re-amputation, as well as death, we attributed to the unfavorable results of amputation. The use of an adequate algorithm for performing leg amputation, taking into account the affected angiosome of the foot, will allow achieving favorable results even in those patients who have a high risk of developing postoperative complications (Fig.3).
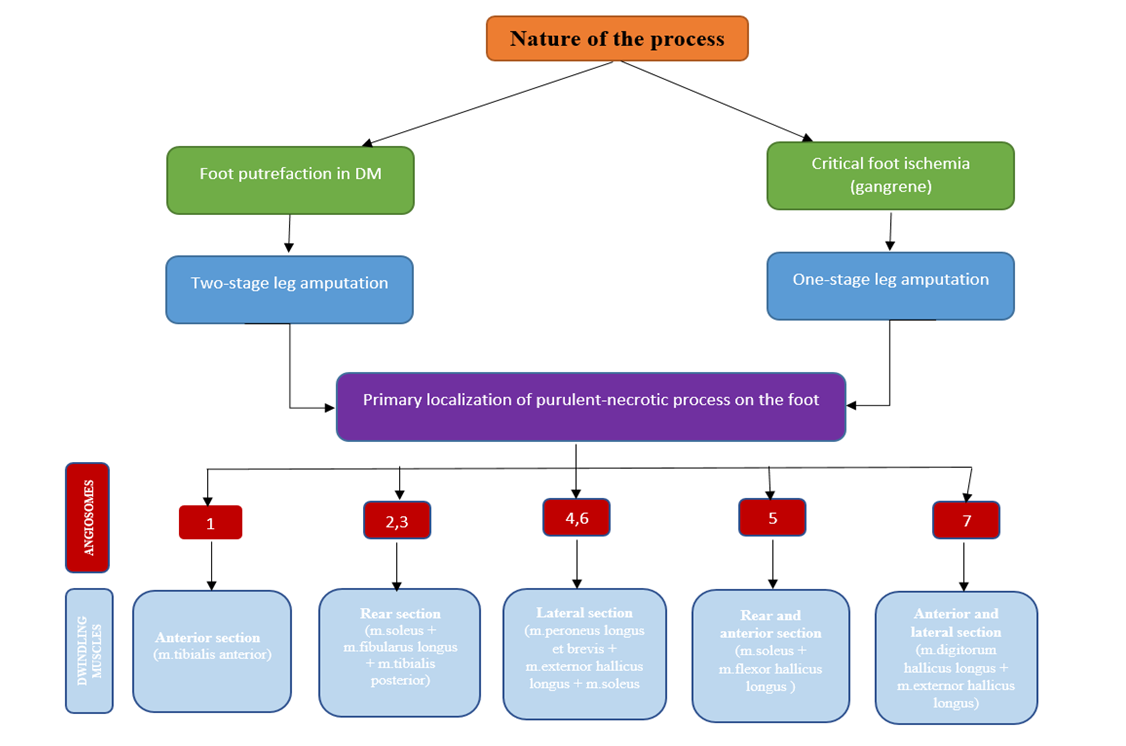 | Figure 3. Algorithm for performing leg amputation |
 | Figure 5. View of the shin stump on the 2nd day after amputation (there is a through drainage tube through the soleus muscle bed under the resected tibia) |
 | Figure 6. The patient's condition after 3 months (limb prosthetics) |
|
4. Discussion
- Summing up the information, it should be noted that the developed differentiated new method for performing amputation of the lower leg in diabetic gangrene of the lower extremities with the removal of the muscle sheath, depending on the affected arterial basin (i.e., angiosomal structures) while maintaining the integrity of the nutrient artery of the tibia, made it possible to significantly improve the results of treatment in terms of preservation of the knee joint by 12.3%. The main effect of this developed method was achieved by reducing the degree of postoperative complications in the stump area and the complete absence of patients who required reamputation at the level of the thigh, which ensured the preservation of the relative support function of the lower extremities. Removal of the leg muscles, taking into account the prevention of ischemia, depending on the affected arteries, and anatomically justified resection of the leg bones contributed to the smooth course of the postoperative period, which made it possible to achieve favorable treatment results.
5. Findings
- 1. When the necrotic process of the focus is located on the dorsum of the foot and in the region of the outer ankle, ischemia of the muscles of the anterior section is noted, with damage to the plantar surface, there is a violation of the arterial blood flow of the muscles of the lateral section and the superficial case of the hind leg. With gangrene of the heel region of the foot, there is ischemia of the superficial and deep muscle case of the posterior leg.2. Performing tibial amputation with a differentiated method in patients with diabetic gangrene of the lower extremities, depending on the localization of the pathological process on the foot, can reduce the incidence of postoperative complications of the tibia stump to 2.7% and increase the frequency of knee joint preservation to 100%.
Consent
- It is not applicable.
Ethical Approval
- It is not applicable.
Competing Interests
- Authors have declared that no competing interests exist.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML