-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(2): 71-73
doi:10.5923/j.ajmms.20231302.09
Received: Jan. 22, 2023; Accepted: Feb. 12, 2023; Published: Feb. 13, 2023

Pathomorphology of Fibrous Polyps of the Female Urethra
Boboev R. A.
Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Boboev R. A., Andijan State Medical Institute, Andijan, Uzbekistan.
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article studied histotopography and specific morphological changes in fibrous urethral polyps in women. As a material, 32 biopsy materials obtained from patients treated in 2018-2021 were histologically examined. in the department of urology of the clinic of Andijan State Medical Institute. With a fibrous polyp, the presence of many fibrous structures in the connective tissue in the area directly under the integumentary epithelium is determined, they are characterized by a small number of blood vessels. In the deep parts of the stroma, connective tissue cells and fibrous structures are rarely located due to the presence of swelling in the interstitium, they contain blood vessels. An analysis of the etiology of the urethral polyp showed that if we take into account the causes and pathogenesis of the polyp, then the development of the polyp tissue is accompanied by inflammatory, degenerative and dysregenerative processes, and it was found that the changes characteristic of these processes persist in the stroma, which is the basis of the polyp.
Keywords: Urethra, Polyp, Fibrosis, Morphology, Histotopography, Inflammation, Dystrophy, Destruction
Cite this paper: Boboev R. A., Pathomorphology of Fibrous Polyps of the Female Urethra, American Journal of Medicine and Medical Sciences, Vol. 13 No. 2, 2023, pp. 71-73. doi: 10.5923/j.ajmms.20231302.09.
Article Outline
1. Introduction
- Female urethral polyps are usually located in the area of the external outlet, clinically they cause pain, stinging during urination, pollaturia, stranguria, urethrorrhagia and wetness of urine [1,2,3]. The causes of urethral polyps are poorly understood and remain unclear. According to the majority of scientific studies, polyps of the urethra in most cases are not considered safe tumors, but are hyperplastic processes characterized by focal proliferation of the epithelium due to the violation of the relationship between the mesenchymal tissues and the epithelium in the urethra wall for unknown reasons [4,5,6]. In appearance, urethral polyps are tumor-like structures in the area of the back lip of the external outlet opening, the size of which is from 2 mm to 1-2 cm, and the outgrowth often consists of a wide leg, the surface is smooth, sometimes hemorrhages and erosions are detected. There are 2 types of polyp tissue structure: fibrotic and adenomatous. Fibrous polyp often occurs alone on the basis of infectious and inflammatory processes. Fibromatous polyp grows slowly and rarely spreads to surrounding tissues. In some cases, elastic fibers have grown a lot, blood vessels have proliferated, and angiomatous tissue may have appeared [2,4,6]. This type of polyp is called urethral caruncle. Urethral caruncle was first identified by Fere in 1926 as a structure rich in blood vessels the size of a raspberry, located in most cases on the back wall of the urethra, strongly hyperemic in appearance, and bleeding when touched. In addition, in the fibromatous type of urethral polyp, the reasons for the growth of coarse fibrous connective tissue in the stroma, the relatively low development of blood vessels and the development of myxomatous process changes in the interstitial substance, the main reason why this type of polyp is relatively common, have not been fully studied.
2. Material and Methods
- As material, 32 biopsy materials obtained from patients who underwent inpatient treatment in 2018-2021 at the urology department of the Andijan State Medical Institute clinic were studied histologically. After drying in 10% formalin solution for 48 hours, the biopsy pieces were dehydrated in increasing concentration of alcohols and embedded in paraffin, and sections were prepared. Histological sections of 4-5 μm were prepared from paraffin blocks, stained with hematoxylin-eosin, van Gieson stains, and observed under a light microscope, and the calcareous areas were photographed.
3. Research Results and Discussion
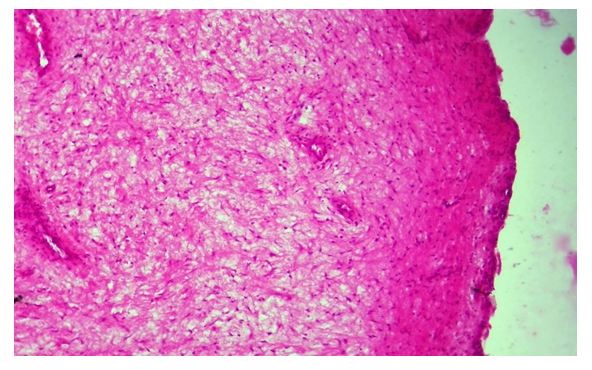
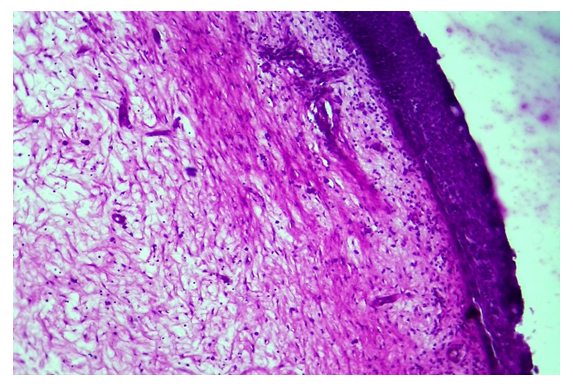
- A polyp is a tumor-like process that develops in almost all organs and tissues covered with epithelium and macroscopically manifests itself in the form of a nodule-like structure. In our material, it was observed that the polyp was located on the back wall of the urethra, close to the blood, in most cases of women undergoing observation and examination. The histological study of the fibrous polyp of the urethra showed that although they are similar in structure and composition, it was found that they differ in the composition of the fibrous tissue, the abundance and location of cellular and fibrous structures in it. It is determined that the epithelium covering the surface of the polyp consists of multi-layered epithelium that varies histotopographically, but in some places it is metaplasia to multi-layered non-coagulated flat epithelium, and there are nodules of cells of the basal layer that have grown into acanthose fibrous tissue of various degrees. It is determined that epithelial cells are densely located in the areas of metaplasia to flat epithelium, most of them are hyperchromic in appearance. It is found that in the areas that have preserved the appearance of multi-layered changing epithelium, the epithelial cells have a round and cubical structure and have maintained a row-by-row arrangement relative to each other. In fact, the growth process of any polyp tumor starts from the private plate of the mucous membrane with connective tissue, and the reason for this is the excessive tissue formation due to chronic inflammation in the connective tissue, excessive hyperplasia of cells and tissue structures, and it protrudes on the surface of the mucous membrane. The fibromatous stroma of the polyps that we studied in this study had a unique structure in each polyp. The histotopographic condition characteristic of all of them is that in the stroma of the polyp there is a predominance of the amount of coarse connective tissue that has grown in the form of fibromatosis. In the area immediately below the covering epithelium, it is determined that the connective tissue contains a large number of fibrous structures and that they are located parallel to the epithelium, and consists of fibromatous tissue, characterized by a small number of blood vessels (Fig. 1). In the deeper areas of the tissue, it is determined that the cells and fibrous structures of the connective tissue are sparsely located due to the presence of swelling in the interstitium, and blood vessels are located in them. It is determined that most of the blood vessels consist of arterioles with a thick wall, and there is an inflammatory infiltrate around them.
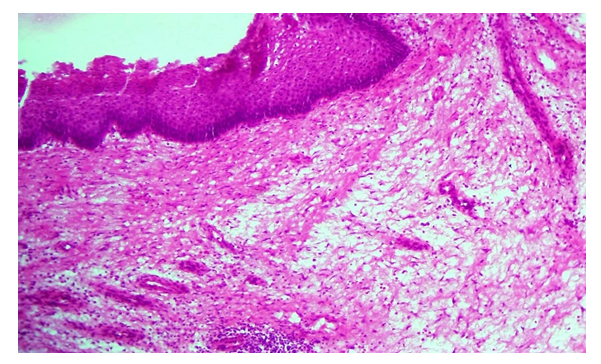 | Figure 1. 42-year-old female urethral fibromatous polyp, covering epithelial metaplasia, fibrous stroma in some areas dense, other areas sparse. Paint: G-E. Magnified: 10x40 |
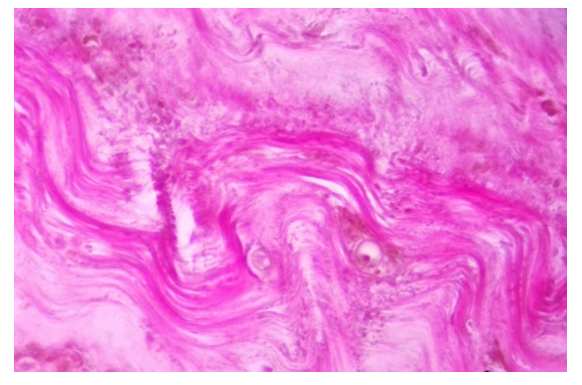 | Figure 3. A 52-year-old woman shows a fibromatous polyp of the urethra, where the collagen fibers are crooked, thickened, and homogenized. Paint: van Gieson. Magnified: 10x40 |
4. Conclusions
- Fibrous polyps of the urethra are similar in structure and composition when studied histologically, but it was found that they differ in the composition of the fibrous tissue, the abundance and location of cellular and fibrous structures in it.In fibrotic polyp, it is determined that there are many fibrous structures in the connective tissue in the area immediately below the covering epithelium, and they are characterized by a small number of blood vessels. In the deep areas of the stroma, the connective tissue cells and fibrous structures are sparsely located due to the presence of swelling in the interstitium, and blood vessels are located in them. Analyzing the etiology of the urethral polyp showed that if the causes and pathogenesis of the polyp are taken into account, the development of the polyp tissue is accompanied by inflammatory, dystrophic and dysregenerative processes.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML