-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(1): 28-33
doi:10.5923/j.ajmms.20231301.07
Received: Dec. 20, 2022; Accepted: Jan. 5, 2023; Published: Jan. 13, 2023

Results of Laparoscopic Pyeloplasty Depending on the Method of the Upper Urinary Tract Drainage
Bakhadyrkhanov M. M.1, Mukhtarov Sh. T.1, Akilov F. A.2, Ayubov B. A.1, Nazarov D. A.1, Nasirov F. R.1, Nuriddinov Kh. Z.1, Soliev T. Kh.1
1Republican Specialized Scientific and Practical Medical Center of Urology, Tashkent, Uzbekistan
2Tashkent Medical Academy, Department of Urology, Tashkent, Uzbekistan
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

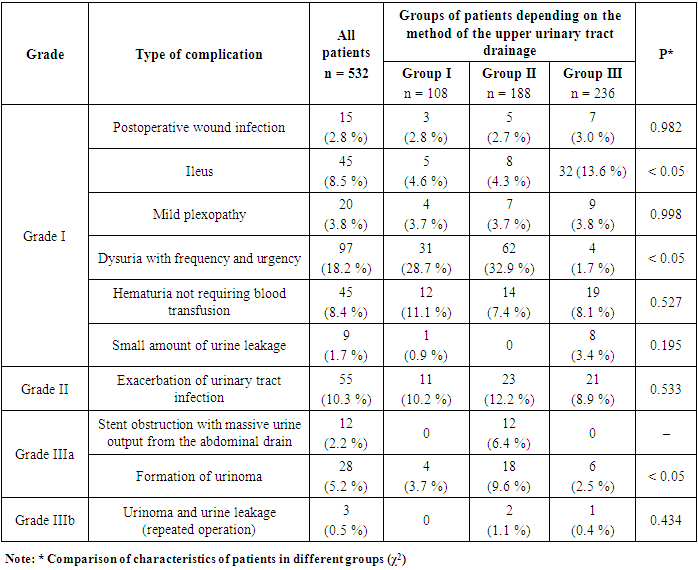
The aim of the study was to analyze the results of laparoscopic pyeloplasty depending on the method of the upper urinary tract drainage. Introduction. To date, laparoscopic pyeloplasty is widely used for the treatment of ureteropelvic junction obstruction. But the issue of the optimal method for drainage of the upper urinary tract during laparoscopic surgeries has not been resolved yet. Material and methods. 532 patients were selected. The mean age of the patients was 25.8 ± 12.6 years. All patients were divided into 3 groups: Group I - 108 (20.3%) patients who had a nephrostomy and ureteral stent installed during laparoscopic pyeloplasty; Group II - 188 (35.3%) patients who were performed only an ureteral stent; Group III - 236 (44.3%) patients who had a nephrostomy and ureteral intubator installed through the skin. Results. The shortest duration of surgery was observed in the group of patients with a ureteral stent (92.5 ± 10.9 minutes versus 125.1 ± 23.0 minutes and 124.0 ± 12.6 minutes; p < 0.05). The lowest intensity of postoperative pain on the 1st day was observed in the group of patients with ureteral stent (4.7 ± 1.2 versus 6.2 ± 1.0 and 6.2 ± 0.9). The method of the upper urinary tract drainage also did not affect the duration of inpatient treatment (on average 3.7 ± 0.7 days). The incidence of postoperative wound suppuration (2.7-3.0%), mild plexopathy (3.7-3.8%), hematuria (7.4-11.1%) and exacerbation of urinary tract infection (8.9-12.2%) did not differ statistically between the groups (p>0.05). Discussions. In our study, dysuric phenomena when using only stents were observed in 32.9% of cases; when installing a nephrostomy and a ureteral stent – in 28.7%, and when draining with a nephrostomy and an intubator – in 1.7% of cases. In Group I, despite the use of a ureteral stent, the presence of nephrostoma significantly reduced the frequency of urinoma formation. Additional interventions had to be performed to treat this complication (percutaneous nephrostomy, stent replacement or nephrostomy) or laparoscopy with repeated formation of the anastomosis was performed, as it was in 2 (1.1%) patients from Group II and in 1 (0.4%) patient from Group III. Conclusions. The installation of a nephrostomy or ureteral stent after laparoscopic pyeloplasty is equally effective for the upper urinary tract drainage. Although the ureteral stent requires less time to install and is associated with less traumatism, it has the most postoperative complications requiring additional interventions.
Keywords: Laparoscopy, Pyeloplasty, Nephrostomy, Ureteral stent
Cite this paper: Bakhadyrkhanov M. M., Mukhtarov Sh. T., Akilov F. A., Ayubov B. A., Nazarov D. A., Nasirov F. R., Nuriddinov Kh. Z., Soliev T. Kh., Results of Laparoscopic Pyeloplasty Depending on the Method of the Upper Urinary Tract Drainage, American Journal of Medicine and Medical Sciences, Vol. 13 No. 1, 2023, pp. 28-33. doi: 10.5923/j.ajmms.20231301.07.
1. Introduction
- Ureteropelvic junction (UPJ) obstruction is a relatively common cause of supravesical obstruction which requires surgical correction [1]. The main goal of treatment is to relieve symptoms and preserve or improve kidney function. Most patients benefit from timely reconstructive surgery [2]. Laparoscopic reconstructive surgeries have taken a special place in the treatment of patients with urological diseases for the last decades. The possibility of performing reconstructive surgeries on the kidney and in the ureter by laparoscopic method contributed to their greater introduction into practice. To date, the advantages of these surgeries over the traditional open method for many diseases in urology are beyond doubt. The main advantages of access are cosmetic effect, a short postoperative period and a quick return to normal life [3-4]. So, in particular, after the presentation in 1993 by Schuessler et al. results of his research on the laparoscopic approach to pyeloplasty [5], it has been accepted worldwide as a minimally invasive alternative to open pyeloplasty and endopyelotomy [6] and is today considered the “gold standard” for the correction of ureteropelvic junction obstruction [7].But the problem of the optimal method for draining the renal pyelocaliceal system during laparoscopic surgery has not been solved yet. Each type of drainage used for draining the upper urinary tract (UUT) has its own disadvantages and advantages. There are isolated works in the literature devoted to this problem. The aim of the study was to analyze the results of laparoscopic pyeloplasty depending on the method of the upper urinary tract drainage.
2. Material and Methods
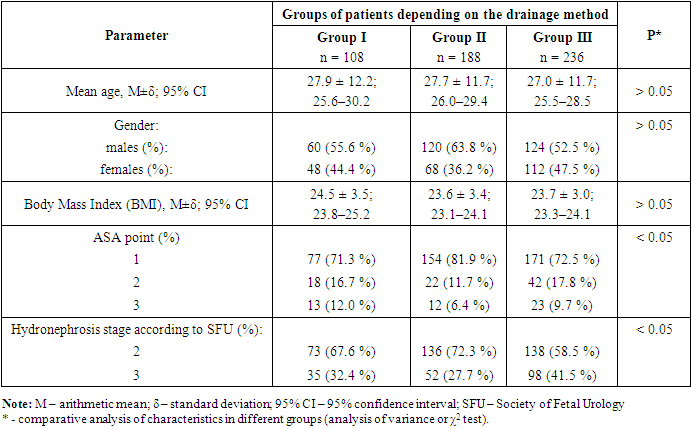
- 532 patients who underwent laparoscopic pyeloplasty at the Republican Specialized Scientific-Practical Medical Center of Urology in the period from 2012 to 2022 were selected for the study. The age of the patients ranged from 4 to 73 years (the mean age was 25.8 ± 12.6 years (M±δ)). There were 302 (56.7%) males and 230 (43.3%) females. Laparoscopic pyeloplasty on the left was performed in 221 (41.5%) cases, on the right – in 311 (58.5%) patients. All patients were divided into 3 groups: Group I - 108 (20.3%) patients who had a nephrostomy and ureteral stent installed during laparoscopic pyeloplasty; Group II - 188 (35.3%) patients whom were installed only a ureteral stent; Group III - 236 (44.3%) patients who had a nephrostomy and ureteral intubator installed through the skin. The baseline characteristics of the patients did not differ significantly between the groups (see Table 1).
|
3. Results
- The shortest duration of surgery was observed in group II patients who had a ureteral stent installed after laparoscopic pyeloplasty (M ± δ - 92.5 ± 10.9 minutes; 95% CI - 90.9-94.1; p < 0.05). In group I, it was 125.1 ± 23.0 minutes (M±δ; 95% CI, 121-129), and in group III, 124.0 ± 12.6 minutes (M±δ; 95% CI, 122– 126 minutes). The duration of the operation in groups I and III did not differ significantly (t-test; p > 0.05; see Figure 1).
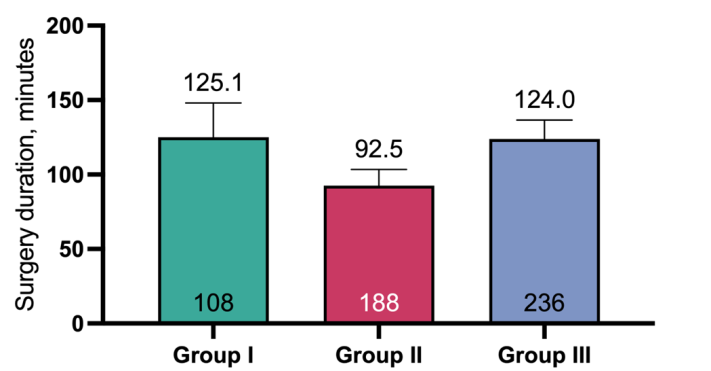 | Figure 1. Analysis of the duration of surgical intervention in comparison of three groups (ANOVA test; p<0.05) |
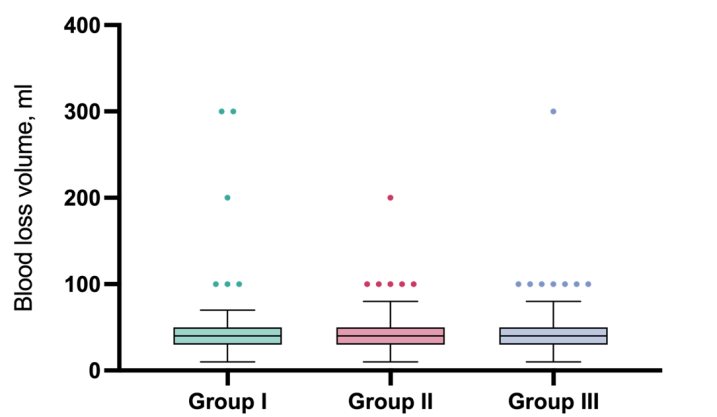 | Figure 2. Box-plot chart of intraoperative blood loss volume analysis in comparison of three groups (Kraskel-Wallis test; p>0.05) |
|
4. Discussion
- Long-term practice has shown that laparoscopic pyeloplasty is an effective and safe method of treating ureteropelvic junction (UPJ) obstruction with easily reproducible results [10]. However, the method of draining the UUT after this operation has not been precisely defined. There are many ways to drain the renal pelvo–calyceal system after laparoscopic pyeloplasty, such as nephrostomy tube, ureteral stent, nephroureteral stent and others [11-12]. In our opinion, the choice of drainage method should be based on several parameters. There are few publications in the literature regarding the effect of installing a certain UUT drainage method on the duration of the surgery. When using only a ureteral stent, the duration of the operation is shorter, since the technique of installing a nephrostomy tube is more complicated at laparoscopic intervention and requires certain skills. An increase in the duration of inpatient treatment with the use of a nephrostomy tube has been reported, but these studies were conducted at the open pyeloplasty [14-17]. We did not observe the effect of increasing inpatient treatment depending on the drainage method. It was found that Foley catheter drainage is important for decompression of the bladder in the early postoperative period. Wollin et al. described the potential benefit of bladder drainage with a urethral catheter for pyeloplasty [13]. We think that an empty bladder can protect the anastomosis from increased pressure, thereby reducing the probability of postoperative suture failure. In addition, decompression of the bladder will prevent the formation of vesicoureteral reflux with the development of reflux nephropathy and ascending infection. Retrograde urine flow at the increased pressure in the bladder is especially often observed with a ureteral stent. Therefore, we installed a urethral catheter for 7-10 days for all patients with ureteral stents. Many studies focus on the fact that ureteral stents are associated with fewer postoperative complications than nephrostomy tubes [14-16]. However, these studies use an open pyeloplasty technique and the number of participants is not large enough to reliably speak about the benefits of stents. Ureteral stents can cause mechanical irritation of the bladder triangle. McMullin et al. observed this phenomenon in 11.1% of patients [15]. Braga H.P. et al. noted symptoms of bladder spasm in 2.9% of patients who required early stent removal [17]. Garg R.K. et al. in a comparative analysis reported that symptoms of dysuria were observed in 85% of cases with ureteral stent versus 25% of cases with nephrostomy [18]. In some cases, these symptoms are associated with stent migration, which can be observed in 2.5–16.6% of cases [15,17]. In our study, when using only stents, dysuric phenomena were observed in 32.9% of cases, when installing a nephrostomy and a ureteral stent – in 28.7% of cases, and when draining with a nephrostomy and an intubator we observed 1.7% of cases. These data should be taken into account by the doctor when choosing a drainage method, since the symptoms of dysuria can significantly reduce the quality of life of patients and require early removal of drainage, which can cause a relapse of the disease. Braga H.P. et al. noted the formation of urinoma in 1.2% of cases in the ureteral stent group and in 0.4% of cases with pyeloureteral stent [20]. In our study the frequency of urinoma formation was higher (on average 5.2%). In the presence of nephrostomy drainage, the frequency of urinoma formation was 3-4 times less (from 2.5% to 3.7%) than with ureteral stent (9.6%). It is interesting to note that in Group I, despite the use of a ureteral stent, the presence of nephrostoma significantly reduced the frequency of urinoma formation. To treat this complication, additional interventions had to be performed (percutaneous nephrostomy, stent replacement or nephrostomy) or laparoscopy was performed with repeated formation of the anastomosis, as it was done in 2 (1.1%) patients from Group II and in 1 (0.4%) patient from Group III. Nephrostomy drainage has a number of advantages over ureteral stents. It is possible to install a drainage of a larger diameter than a ureteral stent, which allows to drain the kidney effectively. A larger drainage diameter reduces the risk of obturation by blood clots and promotes their active evacuation. Nephrostomy drainage allows to calculate the amount of urine excreted by the kidney per day, it is also possible to assess the quality of urine – the detection of hematuria and pyuria. Patients who have been installed a nephrostomy in the postoperative period can be performed antegrade pyeloureterography, which allows to assess the volume of the pelvis, patency of the ureteropelvic junction and ureter. However, nephrostomy drainage significantly reduces the patient’s life quality in the postoperative period [19,20]. Thus, the choice of the UUT drainage method after laparoscopic pyeloplasty should be based on a comprehensive analysis of clinical and anatomical data and the patient's desire.
5. Conclusions
- The installation of a nephrostomy or ureteral stent during laparoscopic pyeloplasty is clinically effective for drainage of upper urinary tract. However, nephrostomy requires additional intervention or lengthens the duration of the surgery. Although the ureteral stent is associated with less trauma and postoperative pain, this type of drainage has the most postoperative complications, and for the treatment of some of them patients require additional surgical interventions or repeated reconstructive surgery. The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML