-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2023; 13(1): 1-5
doi:10.5923/j.ajmms.20231301.01
Received: Oct. 27, 2022; Accepted: Jan. 10, 2023; Published: Jan. 13, 2023

The Etiopatogenesis of Intestinal Necrosis in Acute Mesenteral Thrombosis Early Detection
Sh. Ya. Sattarov, D. A. Sapaev
Khorezm Branch of the Republican Research Center of Emergency Medine, Uzbekistan
Correspondence to: Sh. Ya. Sattarov, Khorezm Branch of the Republican Research Center of Emergency Medine, Uzbekistan.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Values were established that predicted the development of necrosis in the presence of acute mesenteric thrombosis (AMT). Using innovative laboratory markers such as D-dimer, as well as instrumental methods such as CT of the abdominal organs with further use of CT angiography of the abdominal aorta, we were able to significantly reduce the time from admission to the final diagnosis of AMT from 35.1±28.8 in the comparison group up to 10.7±9.3 hours in the main group, p=0.0003. Based on the information received, we can state that this laboratory and instrumental set of measures, which was presented to optimize the diagnosis of AMT, showed the greatest effectiveness in relation to the classical scheme for examining this pathology.
Keywords: Acute mesenteric thrombosis, Diagnosis, Prognosis for the development of intestinal necrosis
Cite this paper: Sh. Ya. Sattarov, D. A. Sapaev, The Etiopatogenesis of Intestinal Necrosis in Acute Mesenteral Thrombosis Early Detection, American Journal of Medicine and Medical Sciences, Vol. 13 No. 1, 2023, pp. 1-5. doi: 10.5923/j.ajmms.20231301.01.
Article Outline
1. Introduction
- Acute mesenteric ischemia (AMI) is a serious disease that develops as a result of a violation of both arterial and venous blood flow and is accompanied by high mortality [Esipov A.V., Patsenko M.B. 2015]. The number of patients with AMI is constantly growing, which is associated with an increase in the number of elderly and senile people, as well as an increase in cardiovascular diseases (CVD) [2,7]. Mortality in acute intestinal ischemia remains high for many years and is 65-95% [9,11]. A variety of reasons for the development of AMI, the absence of specific symptoms and common diagnostic criteria significantly complicate the treatment of this disease [4,16]. In recent decades, there has been a clear desire to improve the results of treatment of patients suffering from acute disorders of mesenteric blood flow and its complications through the development and implementation in practice of early diagnosis methods and ways to complete surgical benefits [13]. A wide variety of etiologies of acute mesenteric thrombosis (AMT), lack of specialized symptoms and specific diagnostic algorithms increase the complexity of the therapy. A large number of classical diagnostic methods have low perception and specificity for detecting this pathology [6,8,12]. Currently, there is an active development of alternative methods for detecting acute embolic occlusion of the vessels of the mesenteric artery by a thrombus.Identification of the AMT pathology at an early stage will improve the efficiency and carry out surgical interventions at the stages of intestinal hypoxia, i.e. remove a thrombus and/or embolus without bowel resection. To date, high efficiency in the diagnosis of obstruction of the mesenteric arteries is the use of CT and CT angiography [1,15]. Even if angiography is the main diagnostic method in most medical institutions, this type of diagnostics has a number of negative aspects, such as: obligatory violation of the integrity of the main vessels, which entails an increased likelihood of developing hemorrhagic burdens in the initial stages of the postoperative period [3,10,14].The main factors of late detection of acute dysfunction of mesenteric hemodynamics is the absence of a typical clinical picture characteristic of this pathology. The course of this pathology is similar to such pathologies as: acute pancreatitis, cholecystitis, infectious food poisoning, etc. Most pathologies with a similar clinical picture do not require active surgical intervention, and the main therapy is medication, which entails late detection of acute dysfunction of mesenteric hemodynamics of mesenteric vascular thrombosis (MVT), which is fraught with formidable complications: ischemic necrosis, intestinal perforation [5,17].To date, there is no single algorithm for combating AMT. AMT today has the status of an emergency surgical pathology, the results of the therapy of which are not sufficiently optimized.The aim of the study: to determine the early clinical signs of the development of intestinal necrosis in acute mesenteric thrombosis.
2. Materials and Methods of Research
- The conducted scientific work is based on the results of a survey of 165 people with AMT. This diagnosis was established based on information from the anamnesis, the clinical picture, the results of an objective study, as well as the results of laboratory research methods, MSCT without the use of a contrast agent, as well as in the presence of a contrast agent (contrast injection into the portal, arterial, venous phases, etc.). d.). The final diagnosis was made after undergoing an inpatient examination in the course of surgical intervention, as well as in the course of clinical and radiological examination in dynamics.The age of the patients varied from 24 to 93 years, the average age was 62.6±1.2 years. According to the frequency of occurrence of AMT depending on gender, the predominance of men over women was established, their ratio was 1.31:1.The most common causes of dysfunction of mesenteric hemodynamics are the pathology of the superior mesenteric artery (SMA) - 88.1%, the inferior mesenteric artery (IMA) - in 3.1% and in 8.8% of cases their combination.Obstructive dysfunction has developed due to the presence of a thrombus or embolus, there are also cases of their combination. In the course of researching information from literary sources and our studies, it was concluded that there is still no consensus on the values of the occurrence of embolism and thrombosis localized in the mesenteric arteries. It should be noted that in most cases we were not able to determine the true etiology (thrombus or embolus). This phenomenon is associated with an illiterate interpretation of the available diagnostic results, as well as the fact that distinguishing a thrombus from an embolism causes significant difficulties in general. It is also worth mentioning that in the presence of an embolism, the clinical picture has an acute course, while the presence of a thrombus has an increasing character up to several days.The most common nosology in patients with AMT is high blood pressure, which was recorded in 75.8% of cases. Acute myocardial infarction and acute impairment of cerebral hemodynamics occurred in 12.7% of cases, it is also worth noting that in 10.3% of cases these individuals had AMT.The data obtained were subjected to statistical processing on a personal computer using programs developed in the EXCEL-2019 package using a library of statistical functions.
3. Results of the Study
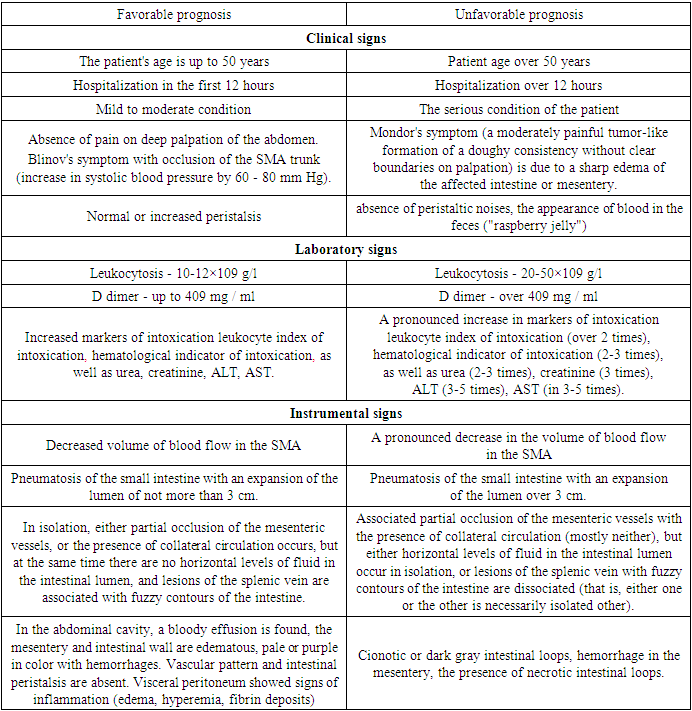
- CT manifestations of the hypoxic status of the intestine are such manifestations as: an increase in the intestinal lumen, flatulence, accumulation of fluids in the intestine with the presence of a horizontal line, the presence of a decrease (arterial dysfunction) or increase (with venous dysfunction) of the thickness of the intestinal wall, local or generalized change in accumulation of contrast material in the intestine, separation of the intestinal wall (halo sign), the presence of free gases in the intestinal wall, the absence of clear contours of the intestinal wall, the presence of effusion in the lumen of the abdominal cavity, as well as compaction of the adjacent lipid tissue.Clinical and radiation manifestations of AMT, which contribute to the development of tissue destruction, are: severe general status of the patient (p=0.015), increase in the level of white blood cells (p=0.031), increase in creatinine (p=0.003), D-dimer values exceed the mark at 409 mg/ml; the presence of free gas in the thickness of the intestinal wall (p=0.001), the absence of clear contours of the intestinal wall (p=0.001), the presence of fluid in the lumen of the abdominal cavity (p=0.016), the compaction of the adjacent lipid tissue (p=0.016), as well as the detection of destruction intestinal tissues during surgery (p=0.039).In the process of performing a statistical type analysis, Fisher's criteria were applied, the chances of developing intestinal destruction were increased in the presence of pathology at the mouth of the SMA (p=0.047), with a decrease in the density of formed thrombi (p=0.039), with the development of hypoxic changes in the intestine (increased lumen (p=0.012), detection of a horizontal line of fluid in the cavity of the small and large intestines (p=0.024), the presence of free gas in the thickness of the intestinal wall (p=0.001), the absence of clear contours of the intestinal wall (p=0.001), the presence of fluid in the lumen of the abdominal cavity (p=0.016), thickening of the adjacent lipid tissue (p=0.016).In the presence of the third stage of this pathology, necrotic changes develop in 88% of cases, while in the second and first stages 65.2% and 25%, respectively (P<0.001).In the formation of thrombi in the central branches (p=0.039), in the presence of pathology in the mouth of the SMA (p=0.047), with the size of the destructive part of the intestine from 3 to 5 cm (p=0.025), in the process of introducing a contrast agent into the SMA and its adjacent branches beyond the level of obturation through collaterals (p=0.003).Taking into account all the above indicators, we are successful in predicting the development of destruction of intestinal tissues in 87% of cases through a discriminant study.The main fundamental reasons for the progress of necrosis are: the stages of pathology, the level of obstruction of the mesenteric arteries, the presence of irreparable damage to the intestinal wall. The presence of these indicators leads to a successful diagnosis in 81%.The discriminant function for predicting the development of necrosis processes is presented as: Y1 = 0.84X1 - 1.71X2 + 0.94X3 (where X1 is the stage of the disease, X2 is the degree of obstruction of the SMA lumen, X3 is irreparable damage to the intestinal wall).The discriminant function for predicting the development of lethal outcomes is presented as: Y2 = 2.6X9 – 1.56X105 + 2.37X41 – 2.65X27 – 0.39 (where X9 is a severe condition, X105 is the preserved lumen of the SMA with a diameter of 7 mm to 9 mm, X41 is the absolute occlusion of the lumen vessel, X27 - dysfunction of arterial hemodynamics).In the process of performing a statistical type analysis on intestinal necrosis, the negative consequences of AMT were associated with increased lethal outcomes, even in the first 24 hours from the onset of the pathology.During the first and second stages of clinical manifestation, most of the patients with obstruction of the visceral branches of the aorta had a history of surgical manipulations on the extremities, organs of the chest and abdominal cavity.In the course of the third clinical stage of the pathology in persons in serious condition with the presence of peritonitis, areas of necrosis or signs of diffuse peritonitis were found during CT scan without the use of a contrast agent. Further information obtained through angiography had no impact on further surgical interventions.As a result, it can be concluded that CT angiography is not safe for persons at the 3rd stage for persons with AMT. It should be noted that the number of studies is inversely proportional to the severity of the general condition of the patient.According to the analysis of the statistical type of deaths with a one-sided disproportionate coefficient of 39%, the presence of atherosclerosis is a sign. It should be noted that in persons with a severe general status, mortality in the absence of atherosclerosis was observed in 96.2% of cases, while in those with its presence, only 36.4%. in persons with mild and moderately severe course, mortality without atherosclerosis was noted in 18%, while with its presence, these values were noted in every third of the subjects.The uncertainty index increased from 39 to 55% with a prognosis based on three features: patient status, atherosclerosis, obstructive conditions of the abdominal aorta. It should be noted that in persons with a severe general status, mortality in the absence of atherosclerosis and the presence of a limited or combined defect was noted in 95.2% of cases.In persons with mild and moderate general status, mortality in the absence of atherosclerosis and the presence of a limited or combined defect was not observed in any of the cases.As a result, based on the above data, we are able to obtain 55% of the data on the prognosis of the course of AMT.According to the analysis of the statistical type on the generalization of the manifestation of the combined pathology of the mesenteric veins with vague borders of the intestine and the presence of hypoxic changes in the small intestine in 75%, we are able to determine the absence of the development of intestinal necrosis.In the pathology of the mesenteric arteries without hypoxic changes in the small intestine in 75% there is no development of intestinal necrosis. It is worth noting that dissociation in one of the groups of manifestations in 89% of cases has the ability to portend the development of necrosis.When combining such signs as: the presence or absence of a horizontal level of fluid in the intestine, defects in the splenic veins with vague borders of the intestine, and the association of incomplete obstruction of the mesenteric vessels with optimal hemodynamics of the collateral vessels, the prognosis of necrosis is 55%.A group of persons with an optimal course is noted, in which necrosis and other above-mentioned signs are absent.In other cases, necrotic lesions were noted in 84% of cases.It should be noted that in the presence of obstruction of the mesenteric vessels with optimal collateral hemodynamics, and with slight manifestations of the fluid level, dissociated sections of the splenic vein with blurry boundaries, necrosis develops in 95 cases.The classification based on priority probabilities predicts the presence of necrosis with success in 86 cases out of 100.In the process of contrast study of the intestinal thickness in the presence of generalized changes in the oxygen starvation of tissues, as well as vague boundaries of the intestine, accompanied by dissociated horizontal fluid phenomena, the detection of necrosis is 12.5%.In the next stage of the work, we developed prognostic criteria for the development of necrosis in AMT, on the basis of which we subsequently gave recommendations on the tactics of treating this cohort of patients (Table 1).
|
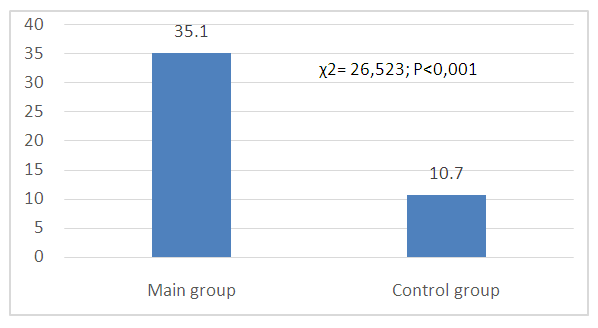 | Figure 1. Terms of establishing the correct diagnosis in the examined groups of patients (hours) |
4. Conclusions
- Values that foreshadowed the development of necrosis in the presence of AMT were established, it is worth noting that the presence of intestinal necrosis in 97% of cases was noted in the presence of associated subocclusion of the mesenteric vessels with dissection of the intestinal walls and the association of the presence of a fluid level in the intestinal lumen during the introduction of contrast into the distal branches. Necrosis was detected in 12.5% of cases in associated generalized hypoxia of the intestine with vague boundaries of the defect in the small intestine, as well as in the presence of dissociation of the presence of a liquid level in the horizontal plane in the large intestine with the introduction of a contrast agent.Based on the action plan drawn up using innovative laboratory markers such as D-dimer, as well as instrumental methods of examination such as CT of the abdominal organs with further use of CT angiography of the abdominal aorta, we were able to significantly reduce the time from the moment of admission to the final diagnosis of AMT.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML