-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1354-1357
doi:10.5923/j.ajmms.20221212.37
Received: Dec. 6, 2022; Accepted: Dec. 28, 2022; Published: Dec. 31, 2022

Clinical and Pathomorphological Changes of Idiopathic Coxarthrosis in Patients with COVID-19
Ibrahimjon Nazarov1, Nosirjon Mahkamov2
1Department of Pathological Anatomy, Andijan State Medical Institute, Andijan, Uzbekistan
2Department of Pediatric Traumatology Orthopedics and Neurosurgery, Andijan State Medical Institute, Andijan, Uzbekistan
Correspondence to: Ibrahimjon Nazarov, Department of Pathological Anatomy, Andijan State Medical Institute, Andijan, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this scientific study, the morphogenesis and specific pathomorphological changes of aseptic necrosis of idiopathic coxarthrosis developed in patients infected with COVID-19 were studied. As an object, surgery was performed on 11 patients, and the area of the femoral head with aseptic necrosis, the external membrane of the bone, and the proximal part of the femur were removed. In the initial period of aseptic necrosis of the femur, it was found that necrobiotic changes developed due to the narrowing and thrombosis of blood vessels in the outer membrane and soft tissues around the bone. Necrobiotic changes were found as a result of necrobiosis of interstitial osteoid material in the femur head and neck bone, resulting in the formation of spaces with destroyed osteoblasts, osteoclasts, and fibroblasts, and then the development of dystrophic and destructive changes in the solid pillars of the bone. During the III period of the process of aseptic necrosis, sequestrations from solid bone columns, and structureless dendrites from intermediate osteoid structures were observed.
Keywords: Idiopathic coxarthrosis, COVID-19, Femoral head, Degenerative, Aseptic necrosis, Morphogenesis, Pathomorphology
Cite this paper: Ibrahimjon Nazarov, Nosirjon Mahkamov, Clinical and Pathomorphological Changes of Idiopathic Coxarthrosis in Patients with COVID-19, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1354-1357. doi: 10.5923/j.ajmms.20221212.37.
Article Outline
1. Introduction
- In 2019, the world was covered by the coronavirus infection caused by SARS-CoV-2. From the first day, international medical teams began to study the acute phase of this infection, but later it became clear that the presence of delayed consequences of a multisystem character, manifested in various forms, was confirmed. In the autumn of 2021, at the suggestion of the World Health Organization, the name "post-covid syndrome", risk factors, pathogenesis and clinical-morphological course were discussed. Since the post-covid syndrome has a multisystem character, it was determined that necrotic-degenerative diseases develop as a result of aseptic necrosis of bones, including aseptic necrosis of the femur [1,2]. In addition, multiple comorbidities have been observed to aggravate the course of SARS-CoV-2, often resulting in death. It was confirmed that arterial hypertension - 55.4%, diabetes - 17.5%, obesity - 35.5%, CKD - 21.6%, and degenerative diseases of the femoral head - 18.4% were diagnosed among people over 60 years of age. Several factors are important in the development of post-covid syndrome; state of immune deficiency, preservation of residual damage, exacerbation of concomitant diseases, reactivation of the virus, catabolic syndrome, persistent viremia, relapse of infection, endothelial dysfunction, vascular thrombosis [3,4,5]. Osteonecrosis disease, which has polyetiological causes, including damage to bone marrow and bone columns observed in the post-covid syndrome, occurs in 20,000 people around the world every year [1,4]. It should be noted that foci of aseptic necrosis can be detected in several bones in one patient, of which 13% of cases occur in the femoral head and ankle. In idiopathic coxarthrosis complicated aseptic necrosis, the death of osteocytes and bone marrow cells occurs as a result of bone infarction, the reason for which is the lack of collateral vessels in the arteries that supply blood to the bone and the development of thrombosis due to COVID-19.Due to the lack of information in the scientific literature about the morphogenesis and pathogistological changes of aseptic necrosis of the pelvic bone tissue due to COVID-19, the study of its development pathogenesis, morphogenesis and pathogistological changes of the aseptic necrosis developed in the bone tissue is an urgent problem. Taking into account these discussions, the scientific research aimed to determine the morphogenesis and characteristic pathomorphological changes of aseptic necrosis of the femoral head developed in patients infected with COVID-19.
2. Material and Methods
- As a material, the clinical-anamnestic and surgical tissue materials of 19 patients who underwent treatment with dystrophic-degenerative diseases of the femoral head in the orthopaedic department of the Andijan Regional Orthopedic and Traumatology Hospital during 2019-2022 were studied. The age of the patients ranged from 25 to 60 years, with an average age of 42.6 years. In 19 patients, various degrees of aseptic necrosis of the femoral head were detected, and in 11 of them, surgery was performed, the area of the femoral head affected by aseptic necrosis, the outer membrane of the bone, the membrane of the femur, and the neck of the femur were removed together. Tissue pieces were examined macroscopically, and 1.5-1.5 cm pieces were cut from each and frozen in 10% formalin with phosphate buffer solution for 72 hours. The bony part of the slices was decalcified in 10% nitric acid. Then, after washing in running water for 3-4 hours, they were dehydrated in alcohols of increasing concentration, paraffin with wax was added, and bricks were prepared. Histological sections of 5-7 μm were taken from paraffin blocks, deparaffinized, and stained with hematoxylin and eosin. Histological preparations were studied under a light microscope, and pictures were taken from the necessary places.
3. Results and Discussion
- According to the results of X-ray and MRI examinations conducted in patients with the post-covid syndrome of aseptic necrosis complicated by idiopathic coxarthrosis, the focus of aseptic necrosis in the area of the femoral head with the presence of necrosis foci in the form of magnetic resonance signals of different degrees, sickle-shaped lines around these foci in T1-VI coronal projection of different degrees It is determined by the appearance of magnetic resonance signals and two lines on T2-VI coronal projection, one with inner high intensity and the other with outer low intensity (see Fig. 1).
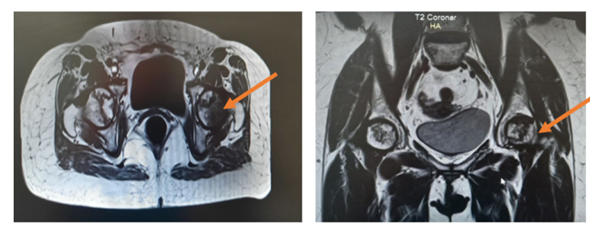 | Figure 1. Aseptic necrosis of the femoral head in idiopathic coxarthrosis caused by COVID-19, low on T1-VI projection, and high on T2-VI projection MRI signals |
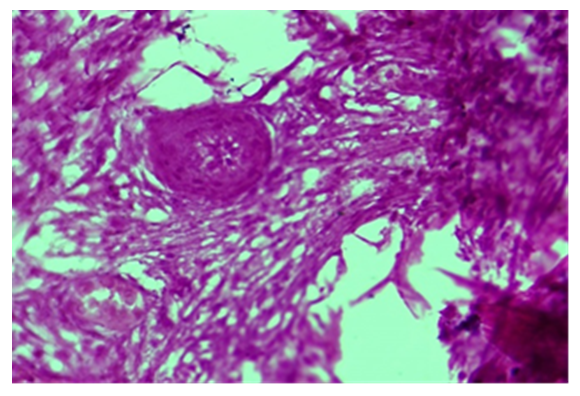
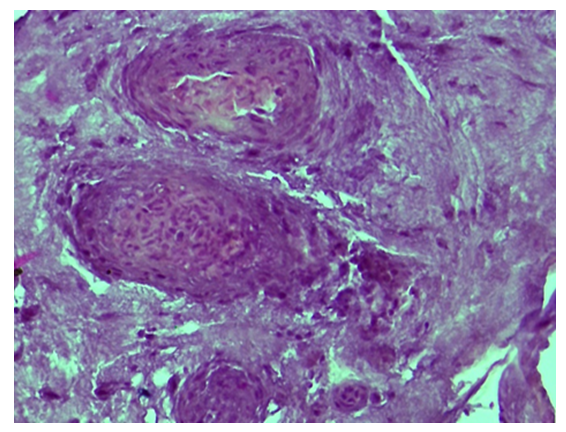 | Figure 3. The proliferation of blood vessel wall cells in the periosteum, narrowing of the cavity. Paint: G-E. Floor: 10x40 |
4. Conclusions
- In idiopathic coxarthrosis, the focus of aseptic necrosis in the head of the femur shows signals of different intensities in the MRT examination, if there is blood, the intensity of the signals increases, if the tissue fluid is absorbed, and if osteosclerosis develops, a decrease is observed. Necrobiotic changes develop as a result of narrowing and thrombosis of blood vessels in the tissues. Initially, the interstitial osteoid substance becomes necrobiosis in the femoral head, creating spaces where destroyed osteoblasts, osteoclasts and fibroblasts are located, then necrobiotic changes occur due to the development of dystrophic and destructive changes in the solid columns of the bone. The process of aseptic necrosis During the III period, during the formation of foci of true necrosis, sequestrations from solid bone pillars, and structureless dendrites from intermediate osteoid structures are determined. In conclusion, it can be said that the full diagnosis of diseases leads to the improvement of the effectiveness of treatment, which is a task performed for the social, and economic development and prosperity of our people.
ACKNOWLEDGEMENTS
- The authors acknowledge the immense help received from the scholars whose articles are cited and included in references to this manuscript. The authors are also grateful to the authors/ editors/publishers of all those articles, journals and books from where the literature for this article has been reviewed and discussed.The authors report no conflicts of interest. The Source of funding is nil.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML