-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1341-1345
doi:10.5923/j.ajmms.20221212.34
Received: Dec. 6, 2022; Accepted: Dec. 23, 2022; Published: Dec. 30, 2022

Outcomes of Surgical Treatment of Patients with Aortic Valve Diseases and Post-Stenotic Expansion of the Ascending Aorta
Aliev Sherzod Makhmudovich, Kayumov Arabbek Ravshanovich
State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery, Named after Academician V.Vakhidov", Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective. The study aimed to compare the results of supracoronary prosthesis and ascending portion of the aorta (APA) endoprosthesis with aortic valve (AV) replacement. Material and methods. The object of the study was 90 patients operated on at the State Institution Republican Specialized Scientific and Practical Medical Center for Surgery, named after academician V.Vakhidov (Tashkent) for AV diseases for the period from 2017 to 2019, who had a concomitant expansion of the APA with a diameter of 40 up to 55 mm. The patients of the first group (n=40) underwent standard AV replacement (AVR) and supracoronary ascending aortic replacement (SCAAR+AVR group); the second group (n=50) patients underwent AVR in combination with exoprosthetic ascending aortic repair (EAAR+AVR). Results. EAAR+AVR compared with SCAAR+AVR allowed to obtain good early postoperative results; in particular, the duration of CPB was reduced from 152.68±48.87 min to 96.62±32.49 min (p<0.001), the aortic occlusion time was decreased from 114.33±29.26 min to 72.28±24.34 min (p<0.001), the frequency of cases of the need for prolonged mechanical ventilation was reduced from 50% to 20% (p<0.001), the connection of cardiotonic support was reduced from 48% to 38%. The frequency of increasing the diameters of the sinus of Valsalva was decreased from 11% to 0%, the reoperation rate from 8% to 2% and the mortality rate from 15% to 4%. Conclusion. Exoprosthetic ascending aortic repair will improve the results of surgical treatment in patients with aortic valve disease by reducing complications, the length of stay of patients in the intensive care unit, and reduce the cost of surgical treatment (by narrowing the indications for the use of expensive consumables).
Keywords: Aortic valve disease, Aortic valve replacement, Supracoronary ascending aortic replacement exoprosthetic ascending aortic repair, Outcomes
Cite this paper: Aliev Sherzod Makhmudovich, Kayumov Arabbek Ravshanovich, Outcomes of Surgical Treatment of Patients with Aortic Valve Diseases and Post-Stenotic Expansion of the Ascending Aorta, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1341-1345. doi: 10.5923/j.ajmms.20221212.34.
1. Introduction
- Despite the use of screening programs, continuous improvement, and the widespread introduction of imaging diagnostic methods and surgical aids, aortic valve (AV) malformations and aortic aneurysms remain among the most common causes of sudden cardiac death [1,2,3]. According to the world literature, the prevalence of thoracic aortic aneurysm is 5-10 cases per 100,000 population per year. The five-year survival rate is 64%. Based on anatomical location, the disease is classified into aortic root or aneurysm of ascending part of the aorta (APA), which is the most common (≈60%), followed by descending aortic aneurysm (≈35%) and aortic arch (<10%) [1,4,5].Treatment of thoracic aortic aneurysm is one of the most challenging and topical issues of modern cardiology and cardiovascular surgery. According to world literature, surgery for aortic valve (AV) and APA aneurysm accounts for 8-12% of all acquired heart defects. The active development of reconstructive surgery for AV pathology and aortic aneurysms has led to significant success in treating this pathology [2,4,6].However, among the unresolved issues, the choice of the method of surgical intervention seems to be the most important [2,5,6]. For reasonable health care, the development of a unified approach to the surgical correction of aortic stenosis and post-stenotic expansion of the APA, as well as the improvement of technical aspects, providing for a reduction in the volume and traumatization of surgical intervention, while maintaining the radicalness of the operation, are essential.The study aimed to compare the results of supracoronary prosthesis and APA endoprosthesis with AV replacement.
2. Material and Methods
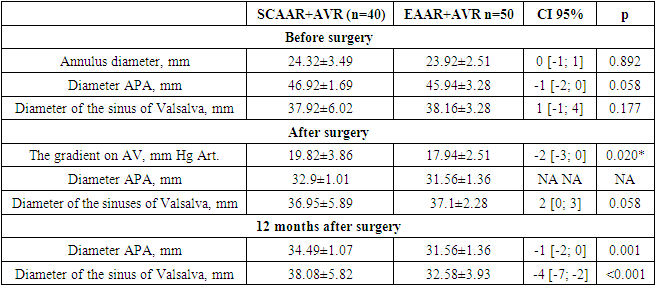
- The object of the study was 90 patients operated on at the State Institution "Republican Specialized Scientific and Practical Medical Center for Surgery, named after academician V.Vakhidov" (Tashkent) for AV defects for the period from 2017 to 2019, who had a concomitant expansion of the APA with a diameter of 40 up to 55 mm.The initial examination included an assessment of clinical status with NYHA heart failure class, standard laboratory tests, echocardiography, coronary angiography, and aortic CT. Clinical and laboratory evaluation of patients was performed through hospitalization and 12 months from the start of the study.Echocardiography was performed using echocardiographic equipment (VIVID 7D, GE Vingmed Ultrasound, "Philips iE33" Philips Healthcare, USA). Global heart function was assessed by measuring LV end-diastolic volume, LV end-systolic volume, and Simpson's LV ejection fraction. Hemodynamic changes in the AV (pressure gradient, severity of regurgitation) and linear parameters of the aorta were assessed: the diameter of the fibrous ring and the size of the aorta at the level of the sinuses of Valsalva and APA. The aorta was measured from the parasternal position along the long axis. In the postoperative period, transthoracic echocardiography was mandatorily at the time of discharge and 12 months after release.Aortic dilatation was established by contrast-enhanced CT angiography and APA transthoracic echocardiography.Ninety patients with AV malformations and post-stenotic expansion of the APA were examined. The patients of the first group (n=40) underwent standard AV replacement and supracoronary ascending aortic replacement (SCAAR+AVR group); the second group (n=50) patients underwent AV replacement in combination with exoprosthetic ascending aortic repair (EAAR+AVR).- in the SCAAR+AVR comparison group, in 82.5% of cases (33 out of 40), a mechanical AV prosthesis was used; in the remaining 17.5% (7 out of 40), points biological valve was used.- in the leading group EAAR+AVR also in most (76.0%; 38 out of 50) cases, a mechanical valve prosthesis was used (p=0.604).Preoperative EchoCG parameters were comparable between the groups.According to the etiology of AV defect, the patients were distributed as follows:- degenerative defect was detected in 27.5% (11 out of 40) of cases in the SCAAR+AVR group and 36% (18 out of 50) in the EAAR+AVR group (p=0.746).- Bicuspid AK was diagnosed in the SCAAR+AVR group in 52.5% (21 out of 40) cases, in the EAAR+AVR group - in 52% (26 out of 50).- in other cases, rheumatic AV malformation was diagnosed: 20% (21 out of 40) in the SCAAR+AVR group and 12% (6 out of 50) in the EAAR+AVR group (p=0.746).As the primary mechanism for the development of pathology, AV stenosis was identified in the majority of 60% (24 of 40) cases in the SCAAR+AVR group and 64% (32 of 50) in the EAAR+AVR group (p=0.827). AA deficiency was noted in the remaining 40% (16 of 40) of cases in the SCAAR+AVR group and 36% (18 of 50) in the EAAR+AVR group.Thus, the groups were comparable in terms of aetiology (p=0.517), the types of valve prostheses used (p=0.604) and the incidence of stenosis (p=0.807) or AV insufficiency (p=0.508).When comparing preoperative EchoCG parameters from Fig. Table 1 shows that the end-diastolic volume of the left ventricle (LV EDV) in the SCAAR+AVR group averaged 152.72±49.4 (values varied from 119 to 176 ml) and in the EAAR+AVR group it was 153.12±42.98 ml (from 120 up to 176 ml) without a significant intergroup difference (p=0.962).The mean left ventricular ejection fraction (LVEF) was 55.85±7.06% (ranging from 53.75% to 61.25%) in the SCAAR+AVR group and 53.72±4.58% (from 50.25% to 56%) in the EAAR+AVR group (p=0.030).In the same way, the mean values of the end-diastolic size of the left ventricle (LV EDD) had no intergroup statistical difference. Thus, the mean LV EDR in the SCAAR+AVR group was 53.61±10.4 mm (indicators varied from 47.5 mm to 62 mm), and in the EAAR+AVR group, it was 54.2±10.66 mm (from 47 to 62.75 mm) (p>0.999).On the side of the AC on the preoperative EchoCG, the following average values of linear parameters were obtained: the diameter of the fibrous ring of the AC was 24.32±3.49 mm (from 22 to 25.5) and 23.92±2.51 mm (from 22 to 25) in the SCAAR+AVR and EAAR+ group AVR, respectively (p=0.892).The mean diameters of the sinuses of Valsalva were 37.92±6.02 mm in the SCAAR+AVR group (range 34 to 39.5 mm) and 38.16±3.28 mm (range 36 to 40 mm) in the EAAR+AVR group, with no statistical difference between groups (p=0.177). The mean ascending aortic diameter in the EAAR+AVR group was 45.94±3.28 mm (range 44 to 48 mm), while in the SCAAR+AVR group, it was 46.92±1.69 mm (range 45 to 48), also without a significant difference (p=0.058).
3. Results
- The following additional surgical procedures were performed intraoperatively, as shown in Fig. 1. Thus, mitral valve repair (MVP) was performed in 18% (7 out of 40) cases in the SCAAR+AVR comparison group and 26% (13 out of 50) in the EAAR+AVR group (p=0.446). Coronary artery bypass grafts were performed with equal frequency in both the SCAAR+AVR group (10%; 4 of 40) and the EAAR+AVR group (10%; 5 of 50).
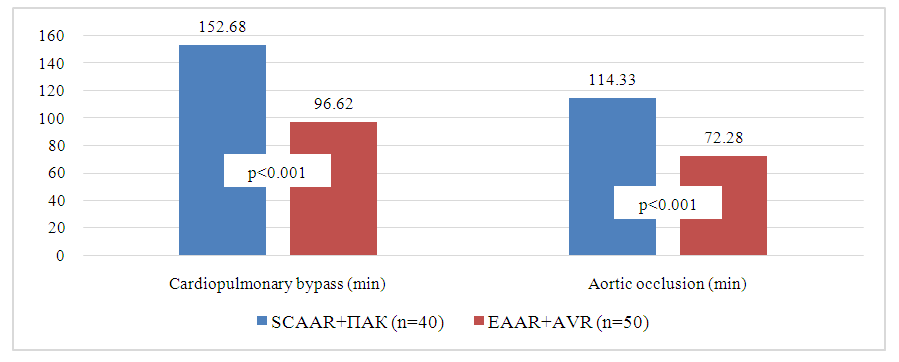 | Figure 1. Comparison of cardiopulmonary bypass and aortic occlusion duration between SCAAR+AVR and EAAR+AVR groups |
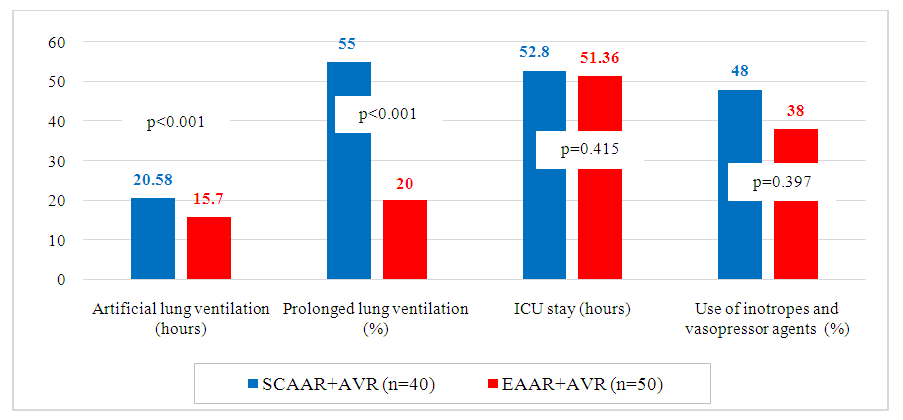 | Figure 2. Comparison of some ICU parameters between the SCAAR+AVR and EAAR+AVR groups |
|
4. Conclusions
- Aortic valve replacement, combined with the exoprosthetic ascending aortic repair, is accompanied by relatively better postoperative parameters and a decreased frequency of reoperations and mortality.As expected, a change in the approach to the treatment of this group of patients will improve the results of treatment by reducing complications, the length of stay of patients in the intensive care unit, and reduce the cost of surgical treatment (by narrowing the indications for the use of expensive consumables).SCAAR – supracoronary ascending aortic replacement,AVR – aortic valve replacement,EAAR - exoprosthetic ascending aortic repairAPA – ascending portion of the aorta
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML