-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1309-1318
doi:10.5923/j.ajmms.20221212.27
Received: Nov. 30, 2022; Accepted: Dec. 20, 2022; Published: Dec. 23, 2022

New Approaches to the Diagnosis of Vitiligo
Avaz Inoyatov , Nigora Khodjaeva , Shamsiddin Sadiev , Jakhongir Narziev
Republican Specialized Scientific and Practical Medical Center of Dermatovenerology and Cosmetology of the Ministry of Health of the Republic of Uzbekistan, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

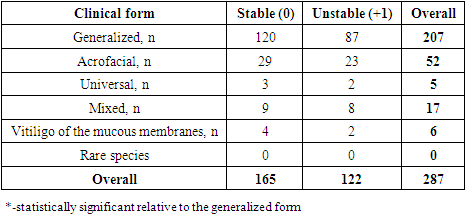
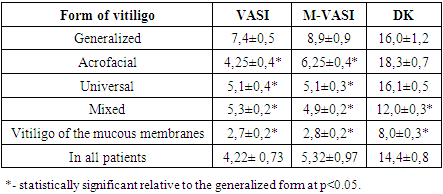
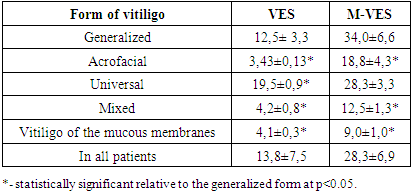
The first mention of vitiligo was noted in the writings of Celsus and Seneca (1st century AD), however, even today, vitiligo cannot be completely cured, it is still a frequent violation of pigmentation, and its impact on the quality of life of patients is very important. According to experts of the British Association of Dermatologists (BAD), psychological distress in vitiligo is subject to screening evaluation. The purpose of the work: based on the use of calculators VAS, VASI and the study of the quality of life in patients to develop a scale for assessing the severity of vitiligo, taking into account the stage of the process, its prevalence, psychological distress of the patient. In addition to determining VES scores, the severity of the disease was judged on the VASI scale. As recommended, according to the VASI scale, the calculation of the affected area is carried out according to the rule of the palms, since the area of the patient's palm is about 1% of the body surface, and the points are calculated as the area of the lesion expressed in the palms multiplied by the intensity of depigmentation (1 = complete depigmentation, 0.5 = 50% depigmentation). Thus, our results showed that vitiligo debuted at a young age up to 30 years, in most cases it was generalized, progressive vitiligo was in 122 (42.5%) patients, the average duration of the disease was 42.6±3.6 months, and the severity of the lesion, estimated by M-VES and M-VASI, taking into account the quality of life, correlated with the VES and VASI scores, respectively, which indicates the validity of our proposed modifications of the scales for assessing the severity of vitiligo.
Keywords: Vitiligo, Pigmentation - mexometry, VAS, NB-UVB
Cite this paper: Avaz Inoyatov , Nigora Khodjaeva , Shamsiddin Sadiev , Jakhongir Narziev , New Approaches to the Diagnosis of Vitiligo, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1309-1318. doi: 10.5923/j.ajmms.20221212.27.
1. Introduction
- The first mention of vitiligo was noted in the writings of Celsus and Seneca (1st century AD), however, even today, vitiligo cannot be completely cured, it is still a frequent violation of pigmentation, and its impact on the quality of life of patients is very important. According to experts of the British Association of Dermatologists (BAD), psychological distress in vitiligo is subject to screening evaluation. A lot of research and scientific papers have been conducted in the CIS countries and abroad on various aspects of the diagnosis and treatment of vitiligo, clinical recommendations on the establishment of clinical forms, stages and severity of vitiligo are constantly updated; recommendations of the European Dermatological Forum (2013), evaluation scales and calculators are proposed: VETF, VES, SA-VES, VASI scales [10,17,25,31], including with an emphasis on quality of life [7], however, there is no consensus on a single classification of vitiligo. To date, there is still insufficient clarity in determining the severity and activity of vitiligo, and evaluating the effectiveness of treatment is difficult due to the different methodological approach to the results obtained. Establishing the severity of the process in vitiligo is a subject of discussion. First of all, visual assessment of lesions is carried out, determination of the level of pigmentation - mexometry, examination in the rays of a Wood lamp, UV photometry [23,24]. Several evaluation scales have been proposed: according to the Point-counting method; the palm method; according to the Vitiligo disease activity score (VIDA SCORE, 1999), the VASI scale (2004) [13], developed by analogy with PASI (Psoriasis area square) [15], EASI [4,5] VETF score (Vitiligo European task force, 2007); assessment of vitiligo severity index (Vitiligo extent tension index (VETI), 2014); VIPs [8,18,19], VIS-22 [11], VDAS [31], VSAS [28], photographing for monitoring, assessment of quality of life in vitiligo by VitiQoL, DLQL [9]. Computer modeling is also used in the programs AutoCAD 2000, PHOTOSHOP, COREL DRAW; spectrophotometry, confocal microscopy (reflectance confocal microscopy), a 3D method for assessing the lesion in vitiligo DIAS (Kawakami, 2011), a VES calculator (vitiligo extent score) [17] expressing the total skin lesion and its modifications – SA-VES (Naja van Geel) [29] and artificial intelligence [10,14,25,26,27]. Each of the proposed scales has its advantages and disadvantages. The VIDA scale has a number of limitations, because it takes into account the subjective opinion of the patient, does not take into account the prevalence of the process [22]. The VETF scale consists of three subscales (% area, staging 0-4, spreading -1-0-+1) and includes an assessment of the prevalence (rule of nines), the stage of the disease (0-3 stages), the degree of progression (-1 - +1). The VETI scale takes into account the assessment of the affected area according to the rule of nines (similar to the assessment of the area of burns) multiplied by a coefficient. The VASI scale provides for the rule of palms to assess the prevalence of the process, since the area of the patient's palm is 1% of the body surface; the assessment of the degree of depigmentation on this scale is expressed in % (0-100%) [13]. At the same time, the degree of depigmentation is expressed as complete depigmentation -100%, single pigmented dots – 90%, depigmented and normal areas alternate with a predominance of depigmented – 75%, when the alternation of areas occurs equally – 50%, the predominance of normal zones over depigmented in one area – 25%, point depigmentation – 10% [12]. Recently, a VES scale, SA-VES, has been proposed, the tools of which allow to estimate the area of the lesion using computer visualization, as well as to take into account the degree of depigmentation. There are works where a correlation has been established between the VES and VASI estimates [3,14], which, according to most researchers, are currently the most optimal. At the same time, these scales do not take into account the patient's quality of life, and the VASI scale does not take into account the head and neck areas [21,30]. At the same time, it is important to emphasize that the presence of depigmentation on the face and neck causes a stronger psychological trauma than localization of the process in other parts of the body [16]. Some authors suggest multiplying the prevalence rate in these zones by 2 [1].Even more difficult is the issue of evaluating the effectiveness of treatment for vitiligo. Thus, according to the results of a systematic review, 25 types of clinical outcomes of vitiligo are given in the literature, in 22% of the works the immediate results from the course of treatment were analyzed and repigmentation was detected in 96% of cases, and repigmentation was measured using 48 (!) different scales. Only 9% of the papers evaluated the quality of life, 13% of the papers contained information about the prevalence of the disease in the studied population, 17% of the papers studied patient satisfaction with treatment. Assessment of the quality of life of patients with vitiligo is important because the disease causes severe psychological trauma, up to depression, these patients feel stigmatized, experience violations of social adaptation [2,6], and psychological distress can aggravate vitiligo, cause the progression of depigmentation and hinder the achievement of a good result of treatment. We believe that creating a universal index for vitiligo, which allows us to judge the prevalence, degree, stage, as well as evaluate the effectiveness of treatment and prognosis of vitiligo, is an important task. By analogy, a very convenient classification of TNM is used in oncology. Unfortunately, in dermatology today none of the methods is so simple and universal.The purpose of the work: based on the use of calculators VAS, VASI and the study of the quality of life in patients to develop a scale for assessing the severity of vitiligo, taking into account the stage of the process, its prevalence, psychological distress of the patient.
2. Materials and Methods
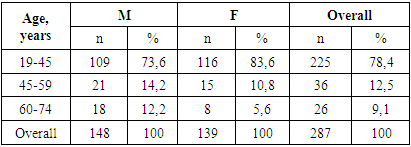
- There were 287 patients with non-segmental vitiligo (148 men and 139 women) aged 19-68 years who applied to the State Institution "RSNPMTSDVIK" in the period from 2018 to 2022. (table.1), the average age was 28.1±1.3 years.
|
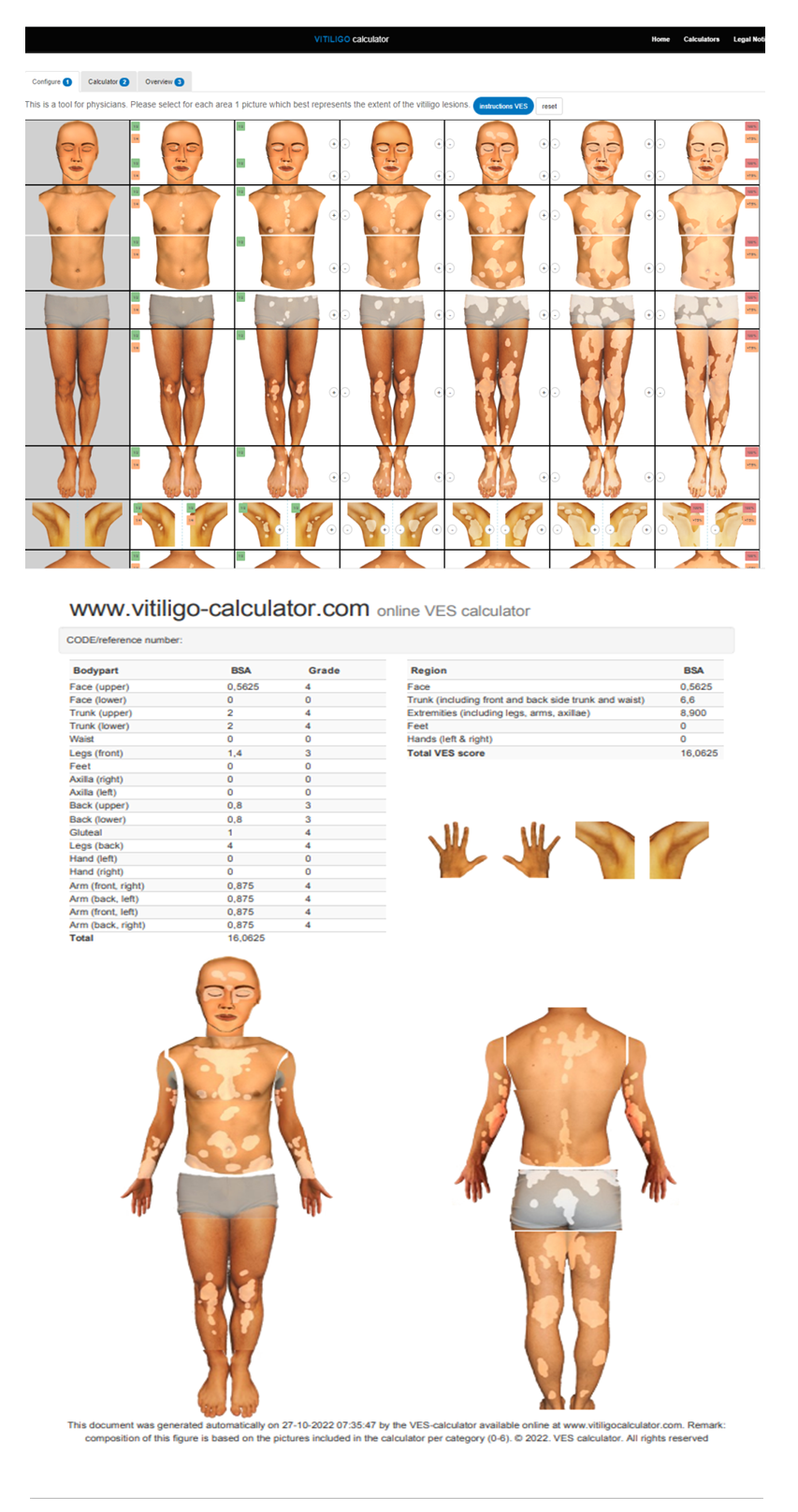 | Figure 1. VES view |
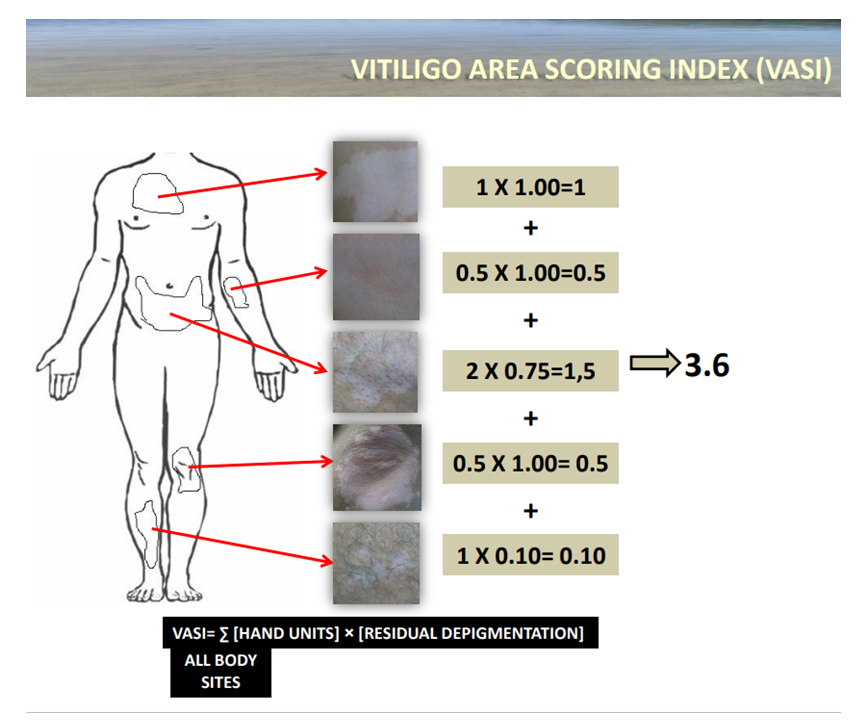 | Figure 2. VASI score |
3. Results and Discussion
- All our patients were with segmental vitiligo. The duration of the disease averaged 42.6±3.6 months, while the onset of vitiligo for less than 1 year before treatment was in 114 patients (40%), the duration up to 2 years – in 53 (18%), from 2 to 5 years – in 54 (18.8%), 5-10 years – 54 (18.8%) (fig. 3).
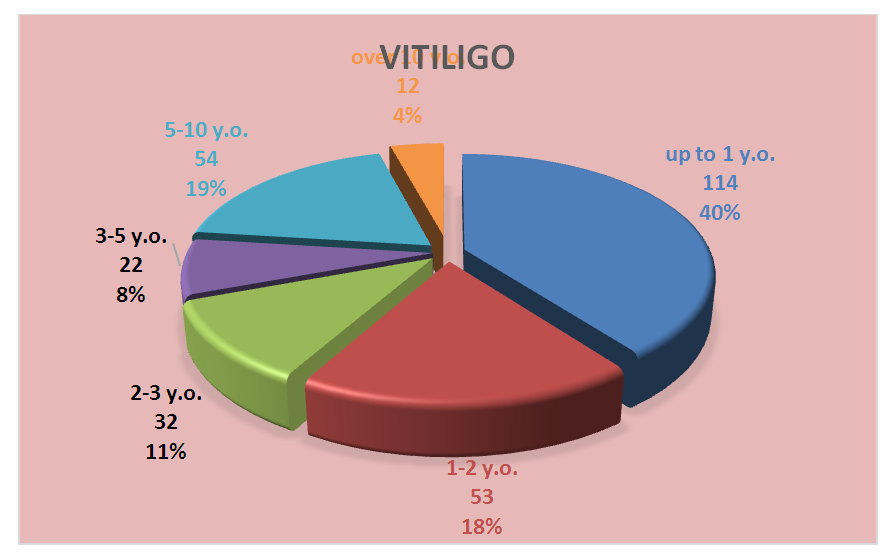 | Figure 3. Distribution of patients depending on the age of vitiligo onset |
 | Figure 4. Signs of unstable course of vitiligo |
|
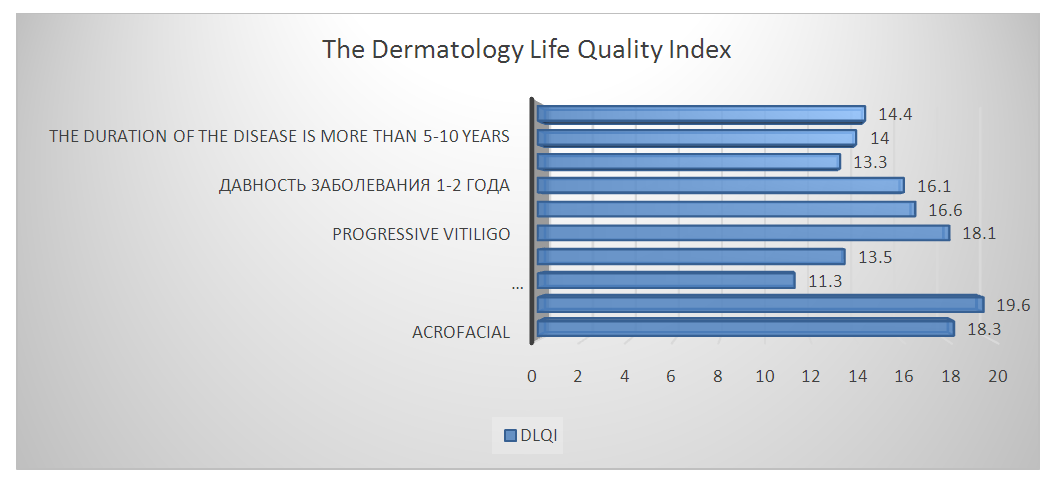 | Figure 5. Quality of life (according to DIKZH) in persons with vitiligo |
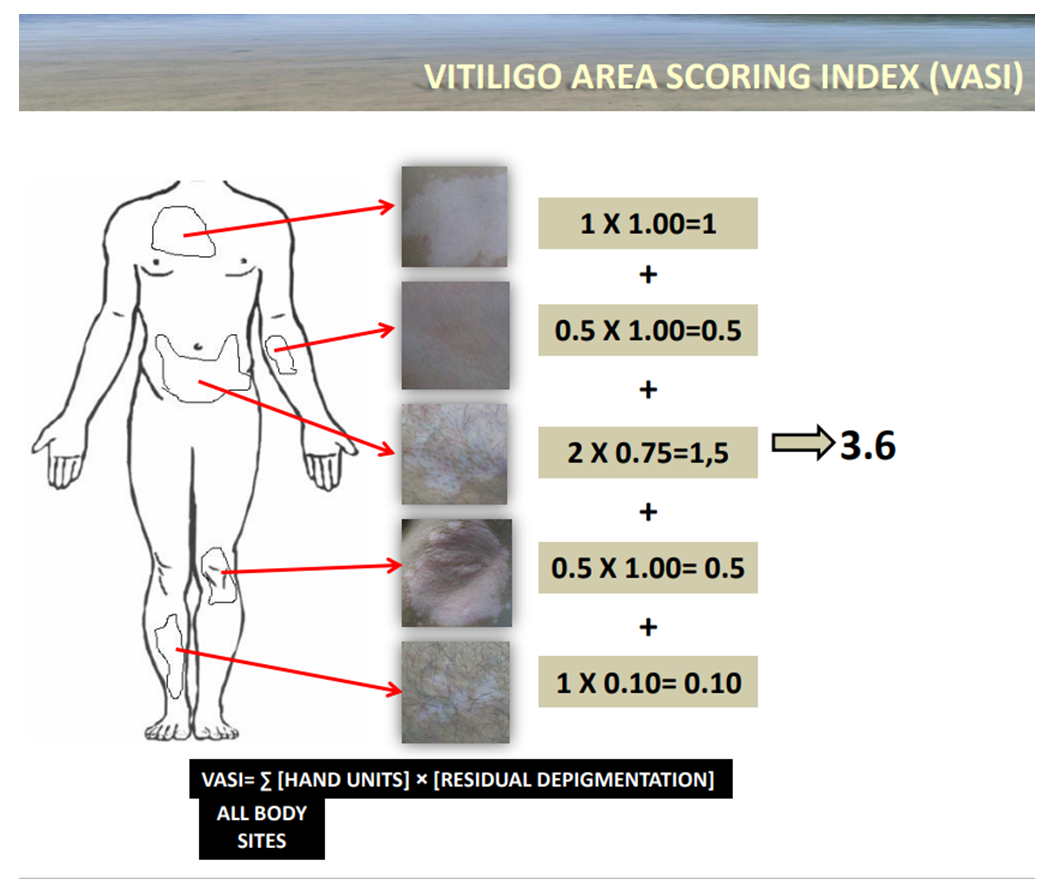 | Figure 6. Calculation of the VASI score |
|
|
4. Conclusions
- 1. The quality of life in patients with vitiligo according to DIKJ was 14.4±0.8 points versus 1.5±0.2 in the control group (p<0.05); there was a significant difference in the DIKJ index depending on the form of the disease, when in persons with localization of the lesion on the face DIKJ was 19.6±0.4 points versus 11.3±0.2 points with generalized form without facial lesion (p<0.05). 2. The indicator on the VES scale correlated weakly and unreliably with the DIC at r=0.231, p=0.219; the VASI indicator correlated with the DIC at r=-0.196, p=0.674, which indicates unreliable weak connections and indicates the absence of a relationship. 3. The modified M-VASI and M-VES scales correlated with the DIC at r=0.455 (p<0.01) and r=0.531 (p<0.01), respectively, which indicates a direct relationship with the average. 4. The modified M-VASI and M-VES scales do not distort the result of the assessment of the area and severity of depigmentation calculated by VASI and VES respectively, as evidenced by the correlation of VASI/M-VASI and VES/M-VES at r= 0.99 (p<0.01) and r=0.95 (p<0.01) accordingly.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML