-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1303-1308
doi:10.5923/j.ajmms.20221212.26
Received: Nov. 28, 2022; Accepted: Dec. 19, 2022; Published: Dec. 23, 2022

The Possibilities of Volumetric Computed Tomography in the Study of the State of the Coronary Bed and Myocardium of the Left Ventricle in Patients with Coronary Heart Disease
Adkham Ilkhamovich Ikramov1, Nigora Mukhsumovna Djuraeva2, Muzaffar Fatkhullaevich Maksudov1, Khanum Valentinovna Abdukhalimova2, Lobar Nasirovna Tursunova1
1Center for the Development of Professional Qualifications of Medical Workers, SU “Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V. Vakhidova”, Tashkent, Uzbekistan
2SU “Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V. Vakhidova”, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The visualization of coronary arteries and myocardial conditions plays a central role in the diagnosis, treatment, and risk stratification of patients with coronary heart disease. Currently, the use of hybrid images combining anatomical and functional data has become extremely popular. In this regard, the current research tasks are focused on the study of the structural analysis of atherosclerotic plaque (ASB), as well as the functional state of the coronary bed.The research aimed to determine the diagnostic significance of volumetric computed tomography in the study of the condition of the coronary arteries and myocardium of the left ventricle (LV) in patients with coronary artery disease.Materials and methods. The results of the study of 56 patients (35 men and 11 women) with coronary artery disease, aged from 43 to 74 years (average age was 58.3±6.7 years), examined in the department of MR and CT diagnostics of the State Institution Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V. Vakhidova in the period from 2019 to 2022 The first stage was a native study with the calculation of the coronary calcium index, then CT-coronarography was performed and stenotic changes in the SC were detected with the study of the structure of the ASB, and static CT perfusion of the myocardium was performed according to the stress/rest protocol with the introduction of the stress agent sodium adenosine triphosphate (ATP) to assess the state of the LV myocardium. The radiation load on the patient was 3.5± 1.2 mSv.Results. To analyze the data of perfusion CT of the myocardium, 952 LV segments were studied. Of these, 627 segments showed no signs of impaired myocardial perfusion. Subendocardial perfusion defects were detected in 213 segments, and perfusion disorders were transmural in 112 segments. In patients with CAD-RADS 4A and CAD-RADS 4B categories, hypoperfusion sites with TPR values of 0.91±0.068 were determined. In the group of patients with CAD-RADS 5 category, TPR values were 0.82±0.095. At the same time, LV myocardial hypoperfusion zones were significantly more frequent – in 203 segments (62.5%) corresponded to the areas of CA with the presence of calcified ASB (p=0.024) and less often – 122 segments (37.5%) were observed in the areas of CA with soft-tissue (not calcified) and mixed (partially calcified) ASB (p=0.037).Conclusion. The conducted clinical studies have shown the wide diagnostic capabilities of volumetric computed tomography (with a combination of CT angiography of the spacecraft with CT perfusion of the LV myocardium) in studying the morphological and functional state of the spacecraft with high accuracy within a single method.
Keywords: Volumetric computed tomography, Atherosclerotic plaque structure, Left ventricular myocardium, Perfusion disorder zones, Ischemic heart disease
Cite this paper: Adkham Ilkhamovich Ikramov, Nigora Mukhsumovna Djuraeva, Muzaffar Fatkhullaevich Maksudov, Khanum Valentinovna Abdukhalimova, Lobar Nasirovna Tursunova, The Possibilities of Volumetric Computed Tomography in the Study of the State of the Coronary Bed and Myocardium of the Left Ventricle in Patients with Coronary Heart Disease, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1303-1308. doi: 10.5923/j.ajmms.20221212.26.
1. Introduction
- According to the Global Health Assessments published by the World Health Organization (WHO), cardiovascular diseases (CVD) continue to occupy a leading position in the list of leading causes of death worldwide. Among all CVD, the greatest risk for the adult population is coronary heart disease (CHD). To date, in many countries of the world, CVD treatment and prevention technologies have reached a high level and now people who have suffered these "vascular catastrophes" will be able to live long enough. According to statistics, in the developed countries of the world, there is a tendency to reduce mortality from coronary heart disease due to timely diagnosis by improving methods for detecting diseases at early stages, which makes it possible to increase life expectancy by an average of 10-15 years.As it is known, the main pathophysiological feature of coronary heart disease is an acute or chronic imbalance between the oxygen needs of the myocardium and the capabilities of the coronary blood flow to meet these needs. Atherosclerotic coronary artery disease (CA) is the most common cause of myocardial ischemia. Visualization of the CA and myocardial condition plays a central role in the diagnosis, treatment, and risk stratification in patients with coronary artery disease. Unlike angiographic imaging, which provides anatomical data on the patency of large CA, myocardial perfusion makes it possible to obtain information about the hemodynamic significance of coronary stenoses, as well as about the functional state of coronary microcirculation. The need to assess coronary blood flow is explained by the fact that the narrowing of the lumen, especially in the presence of diffuse narrowing, is not a reliable predictor of the functional severity of the lesion of the coronary bed, because collateral vessels can effectively compensate for tissue blood flow, keeping it at the initial level. Currently, noninvasive examination of patients with suspected coronary artery disease is based on two principles: 1) assessment of the morphological state of the coronary arteries, including the study of the presence of CA stenosis and the structure of atherosclerotic plaque (ASB); 2) assessment of the functional state of the coronary bed (myocardial blood flow) to determine the hemodynamic significance of the lesion. This approach is of fundamental importance since the morphological assessment of coronary stenoses does not reflect the prevalence and severity of left ventricular (LV) myocardial ischemia. To choose the right management tactics for patients with CA obstruction, it is necessary to take into account the nature of the functional effects of stenosis, for example, atheromas that do not cause a decrease in myocardial blood flow should receive maximum conservative treatment, whereas, in cases of ASB affecting myocardial perfusion, the issue of surgical intervention is being resolved. With a combined assessment of morphology and function, the prognosis and monitoring of patients become more reliable and effective. Computed tomography (CT) of the heart is a non-invasive reference model for the assessment of CA and has become the predominant imaging method for the detection of coronary heart disease with high diagnostic accuracy. Technological progress, together with improvements in spatial, temporal, and contrast resolution, have gradually improved the image quality and reliability of this method. The current tasks of CT are now focused on studying the structural analysis of ASB, functional studies, and reducing the radiation dose to the subject.To date, the use of hybrid images combining anatomical and functional data has become extremely popular. However, this is associated with additional costs and time, which often makes the diagnostic process impractical. The above led to the need to perform an analysis of myocardial perfusion using CT itself in the same procedure as the anatomical assessment of the state of the spacecraft. This approach involves using only one piece of equipment, reducing support staff, and reducing the time and cost of research. In various CT study protocols, the assessment of perfusion can be qualitative, quantitative or semi-quantitative. The implementation of this aspect can be a turning point in the clinical routine for better stratification of the patient's risk based on the results obtained.Goal. To determine the diagnostic significance of volumetric computed tomography in the study of the state of LV CA and myocardium in patients with coronary artery disease.
2. Materials and Methods
- The results of the study of 56 patients (35 men and 11 women) with coronary artery disease, aged from 43 to 74 years (average age was 58.3±6.7 years), examined in the department of MR and CT diagnostics of the State Institution "Republican Specialized Scientific and Practical Medical Center of Surgery named after Academician V. Vakhidova" in the period from 2019 to 2022 All patients had the main diagnosis: Multifocal atherosclerosis. Coronary heart disease. Angina of tension. Functional Class III by NYHA. The patients underwent volumetric CT-coronarography and CT-perfusion of the myocardium on a wide-detector 640-slice computed tomograph "Aquillion one" version of Genesis (Canon Medical Systems, Japan). The width of the scanning area was 16 cm (for one revolution of the tube), which made it possible to completely cover the anatomical region of the heart. The first stage was a native study for calculating the coronary calcium index according to the standardized A.S.Agatston method using special software Calcium Score. Then a CT scan of the heart and CA was performed with the introduction of a test bolus contrast agent (Unigexol 350) through a peripheral venous catheter with a diameter of 18-22G into the cubital vein at a rate of 5.0-5.5 ml/sec. At the same time, stenotic changes in the spacecraft were detected, and the structure of the ASB was studied. To assess the state of the LV myocardium, static CT perfusion of the myocardium was performed according to the "stress/rest" protocol with the introduction of the stress agent sodium adenosine triphosphate (ATP) at the rate of 1 mg/kg for 1-3 minutes and rest (without the introduction of a stress agent). The scheme of the CT examination protocol is shown in Figure 1. The radiation load on the patient was 3.5± 1.2 mSv.
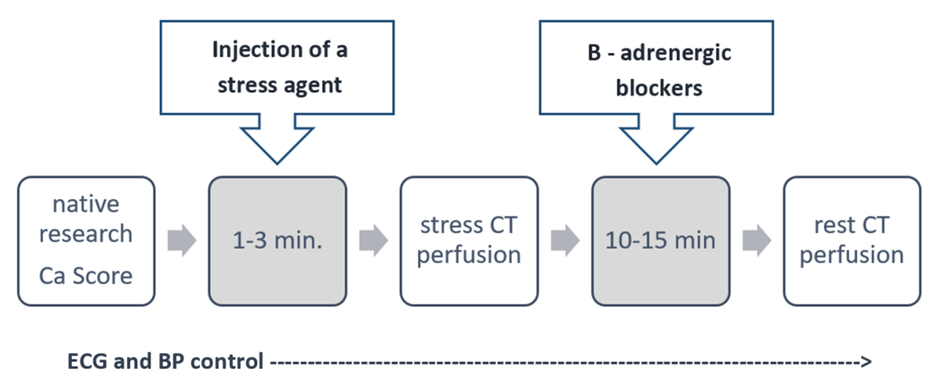 | Figure 1. Diagram of the protocol of CT perfusion examination |
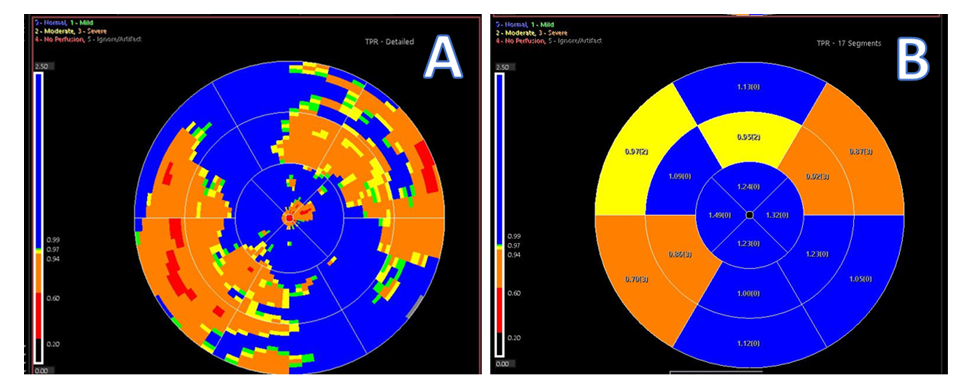 | Figure 2. Polar map showing absolute TPR values for each 2 x 2 mm voxel (A) and TPR values for 17 segments (B) |
3. Results and Discussion
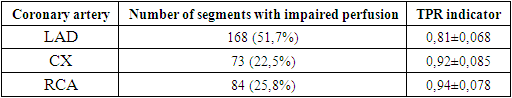
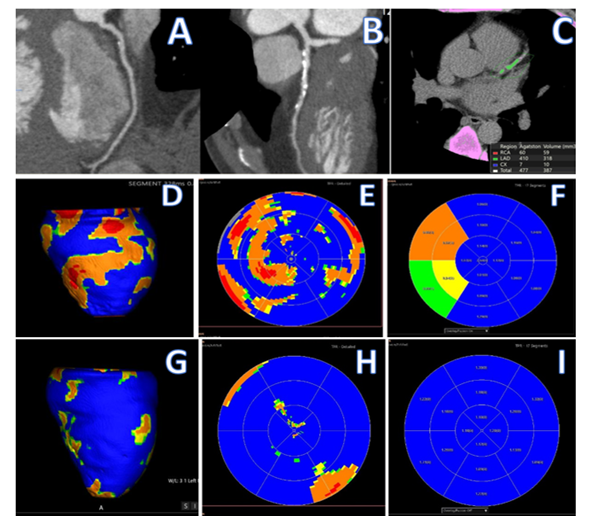
- To analyze the data of perfusion CT of the myocardium, 952 LV segments were studied. Of these, 627 segments showed no signs of impaired myocardial perfusion. Subendocardial perfusion defects were detected in 213 (65.5%) segments, and perfusion disorders were transmural in 112 (34.5%) segments. The average density of the unchanged myocardium during the study in the arterial phase of contrast was +76 ±16.2 Hounsfield units (HU), while the average density of the myocardium in the perfusion defect zone varied within +27±10.4HU. When evaluating the results of volumetric perfusion computed tomography, the largest number of myocardial hypoperfusion sites were detected in the segments belonging to the anterior interventricular branch (LVV) blood supply basin – 168 (51.7%) (p=0.041). The distribution of the identified areas of left ventricular perfusion disorders by segments during the stress phase of the study is shown in Figure 3.
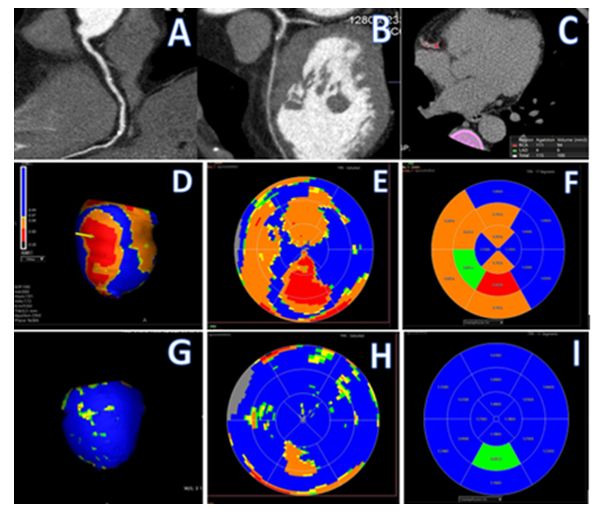
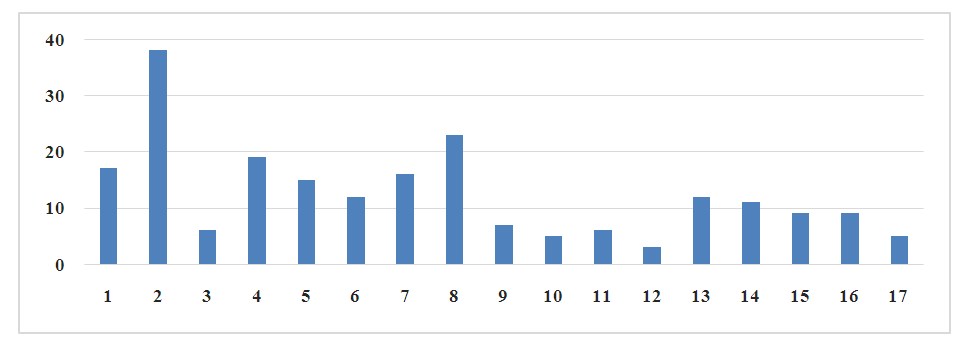 | Figure 3. Distribution of the revealed stress defects of myocardial perfusion of the left ventricle by segments |
|
4. Conclusions
- Clinical studies have shown that the combination of CT angiography of the spacecraft with CT perfusion of the LV myocardium makes it possible to study the morphological and functional state of the spacecraft with high accuracy within the framework of one method. Thus, CT perfusion helps to significantly increase the specificity and prognostic value of a positive CT coronarography result. This approach allows us to reveal the wide diagnostic possibilities of the CT method - from the detection of multivessel lesions to microvascular dysfunction of the coronary bed. A combination of methods is particularly relevant when solving the issue of the need for revascularization. There is a need to conduct large-scale prospective studies with large cohorts of patients to study the effectiveness of the use of CT perfusion of LV myocardium on the clinical outcomes of coronary heart disease compared with a standard examination of such a category of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML