-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1269-1272
doi:10.5923/j.ajmms.20221212.21
Received: Nov. 16, 2022; Accepted: Dec. 2, 2022; Published: Dec. 14, 2022

Changes in the Central Hemodynamics in the Surgical Treatment of Glaucoma in Children under the Conditions of Combined Anesthesia
Mamatkulov I. A., Yusupov A. S., Satvaldieva E. A., Tolipov M. G., Omonov S. Kh.
Department of Pediatric Anesthesiology and Intensive Care, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In the surgical treatment of glaucoma in children under anesthesia protection, the maximum reduction in intraocular pressure (IOP) is required. Otherwise, there is a possibility of a dangerous complication - vitreous prolapse. In this article the combined use of inhalation anesthetic sevoflurane in the surgical treatment of glaucoma in children is discussed as a method of improving the anesthetic protection of children.
Keywords: Surgical treatment, Anesthetic sevoflurane, Glaucoma, Intraocular pressure, Ophthalmic operations
Cite this paper: Mamatkulov I. A., Yusupov A. S., Satvaldieva E. A., Tolipov M. G., Omonov S. Kh., Changes in the Central Hemodynamics in the Surgical Treatment of Glaucoma in Children under the Conditions of Combined Anesthesia, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1269-1272. doi: 10.5923/j.ajmms.20221212.21.
Article Outline
1. Introduction
- In the surgical treatment of glaucoma in children under anesthesia protection, the maximum reduction in intraocular pressure (IOP) is required, which minimizes the possibility of a dangerous complication - vitreous prolapse [1,2,9]. In addition, low intraocular pressure is a prerequisite for quite complex manipulations: suturing the iris, implanting an intraocular lens. In this regard, when providing anesthesia for intraocular operations, it is necessary to exclude the use of drugs that increase intraocular pressure. [3,4,8]. In addition, when conducting anesthesia during ophthalmic operations, the anesthesiologist should avoid excessive excitation of the patient, his cough and other actions that could increase intrathoracic, intraocular, systemic arterial pressure. [7,11,12]. Currently, inhalation anesthetics can meet all these requirements in pediatric anesthesia practice. In this regard, the use of inhalation anesthetic sevoflurane in combination with microdoses of fentanyl in glaucoma in children is the most relevant. [5,6,10].The aim of the research: Improving the anesthetic protection of children by the combined use of inhalation anesthetic sevoflurane in the surgical treatment of glaucoma in children.
2. Materials and Methods
- To provide anesthetic protection in 38 sick children during the surgical treatment of glaucoma, the following combinations were used: fentanyl with sevoflurane (Group 1 - 52.63%), fentanyl with propofol (Group 2 - 47.37%). Children aged from 1 to 5 years old accounted for 57.89% of the total number of patients, children from 6 to 10 years old - 26.32% and children from 11 to 15 years old accounted for 15.79%.Patients of the 1st group after premedication, induction was carried out by inhalation of sevoflurane up to 3 vol%. Small doses of fentanyl were administered intravenously - 0.008-0.01 mg/kg. Tracheal intubation was performed against the background of the introduction of arduan at a dose of 0.06 mg/kg. ALV was carried out by the apparatus "Boyle Intemational-2" (USA) in a semi-open or semi-closed circuit. Myorelaxation was maintained by the introduction of 1/3 of the main dose of arduan. Anesthesia was maintained by inhalation of sevoflurane at a dose of 0.8 - 1.5 vol%. Infusion therapy was carried out at a rate of 5-7 ml/kg/h. After the end of the operation, with the advent of adequate spontaneous breathing, the trachea was extubated. After the operation, the patients woke up quite quickly, within 13.8±0.8 minutes.During the induction period, patients of the 2nd group received bolus solutions of propofol at a dose of 3 mg/kg and fentanyl at a dose of 0.008-0.01 mg/kg. The dose of propofol during the maintenance of anesthesia averaged 7.3±0.4 mg/kg/h. Intraoperatively, infusion therapy was performed at a rate of 10 ml/kg/h. The duration of the awakening stage was 35.5±5.6 min.The study of hemodynamics was performed on an Aloka SSD-260 echocardiograph (China) with a 3.5 MHz probe. Echocardiography (EchoCG) parameters were calculated automatically. The following values were determined: stroke index (SI) = SVR /S ml/m2, cardiac index (CI) = MOC/S l (min*m2), specific peripheral resistance (SPR) = SBP/SI in s. units Computer analysis of echocardiography made it possible to calculate indicators of myocardial contractility and diastolic function of the left ventricle.Measurement of intraocular pressure was made according to A.N. Maklakov. Normal IOP is 16-23 mm. rt. Art. Patients had IOP measured before and after surgery. The results of clinical and functional studies were processed by the method of variation statistics Student's T-test.
3. Results of the Study and Their Discussion
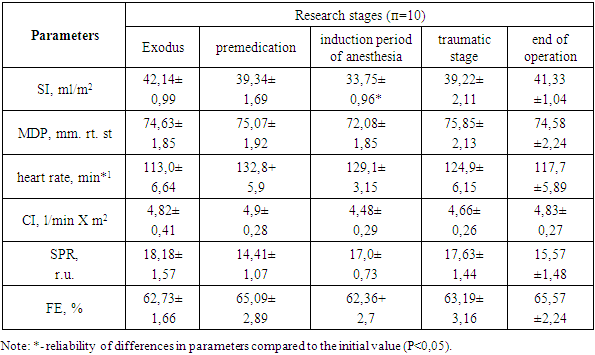
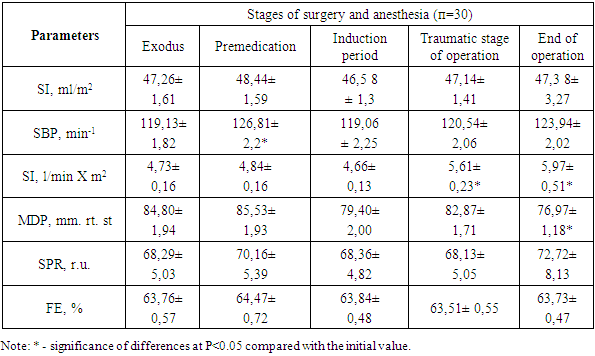
- The results of the study of hemodynamic parameters during combined anesthesia with the use of fentanyl and sevoflurane are presented in table 1.
|
|
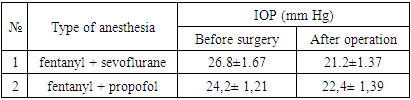
|
4. Conclusions
- 1. A study of the response of the cardiovascular system to various options for general anesthesia and surgery in children with glaucoma revealed minor and compensated changes in the main hemodynamic parameters, which indicated effective anesthetic protection of the child's body from surgical trauma.2. Anesthesia aids with microdoses of central analgesics - fentanyl with sevoflurane and fentanyl with propofol provide adequate pain relief while maintaining low IOP, which is the method of choice for anesthesia in the surgical treatment of glaucoma in children.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML