-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1256-1260
doi:10.5923/j.ajmms.20221212.18
Received: Nov. 22, 2022; Accepted: Dec. 9, 2022; Published: Dec. 14, 2022

Сlinical Efficiency of Prehospital Thrombolysis in ST-Segment Elevation Myocardial Infarction
A. L. Alyavi, S. R. Kenjaev
Bukhara State Medical Institute Named after Abu Ali Ibn Sina, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the research was to study the clinical efficiency of prehospital thrombolytic therapy in acute ST-segment elevation myocardial infarction. Material and methods. 108 acute myocardial infarction patients with ST segment elevation aged from 35 to 67 years were examined. Patients were randomized into two groups: (group A) included 50 patients who received prehospital thrombolytic therapy and standard therapy. Group 2 (group B) included 58 patients who were performed thrombolytic therapy in a hospital setting. Results. In the prehospital thrombolysis group, Q-wave myocardial infarction was developed much less frequently than in the control group (39.7% versus 44%; p <0.05). There were significantly fewer life-threatening heart rhythm disturbances in the form of ventricular tachycardia, ventricular fibrillation, as well as severe classes of acute left ventricular failure in the first group. Lethal outcome was observed in 1 patient from group 2 due to progressive cardiogenic shock. Severe chronic heart failure classes according to NYHA were developed less often among the patients of the 1st group one month later. Conclusion. Thus, the transformation of ST-segment elevation myocardial infarction –acute coronary syndrome - into various acute forms of coronary artery disease and the development of complications is determined by the degree and speed of the onset of reperfusion in the infarct-associated artery. Prehospital thrombolysis in STeACS, accelerating the symptom-reperfusion time, had a positive effect on the clinical course of the disease, promoted the development of abortive myocardial infarction, preventing the development of life-threatening complications.
Keywords: Prehospital thrombolysis, ST-segment elevation myocardial infarction, Reperfusion, Acute left ventricular failure, Acute coronary syndrome
Cite this paper: A. L. Alyavi, S. R. Kenjaev, Сlinical Efficiency of Prehospital Thrombolysis in ST-Segment Elevation Myocardial Infarction, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1256-1260. doi: 10.5923/j.ajmms.20221212.18.
1. Introduction
- Acute ST-segment elevation myocardial infarction (STEMI) is the leading cause of death in most countries of the world, including Uzbekistan. High rates of morbidity and mortality from acute myocardial infarction (AMI) make the problem of AMI treatment not only medical, but also socially significant. Currently, the diagnosis and treatment of AMI is developing. New drugs and interventional approaches have appeared. The percentage of coronary blood flow restoration with percutaneous coronary intervention using stent implantation has significantly increased. It led to a significant improvement in the results of treatment. There has been a decrease in mortality from coronary heart disease in Europe, North America and other developed countries for the last decades. At the same time, various forms of coronary heart disease still occupy leading positions in the structure of morbidity and mortality with a significant spread of indicators in different countries of the world [1-3]. Mortality from STEMI is decreasing against the background of the widespread introduction of invasive treatment of patients. According to national registers in Europe, hospital mortality ranges from 6 to 14%. In 2016, 187240 cases of AMI (including repeated one) were recorded in the Russian Federation, 33185 (17.7%) of them died during hospitalization. The same indicator in 2015 was 18.6% (with 18,8511 registered cases of AMI) [3]. The main factor determining the final size of a myocardial infarction (MI) is the time to myocardial reperfusion. The expansion of the necrosis zone in acute myocardial infarction grows like an avalanche and, in this regard, the main task of organizational and therapeutic tactics is to achieve early, effective and stable reperfusion of the occluded vessel. The use of thrombolytic therapy in such patients as soon as possible after the onset of pain syndrome is an important factor affecting the further prognosis and disability of patients. Myocardial infarction caused by complete occlusion of the coronary artery is developed after 15-30 minutes of severe ischemia, and with a duration of occlusion of more than 30 minutes’ irreversible injury of the myocardium occurs [4-6].It has been proved that the rate of restoration of blood flow during occlusion of an infarct-related artery is the main factor determining the final size of a myocardial infarction and the development of complications. The development of collateral blood flow significantly less affects these indicators. It determines the therapeutic tactics for complete occlusion of the coronary artery — achieving early and persistent reperfusion of the occluded vessel, which will preserve the myocardium or reduce the spread of the necrosis zone and prevent the development of heart failure and electrical instability of the myocardium [7-8].According to the European Society of Cardiology (ESC), in a meta-analysis of six randomized trials (n=6434), prehospital thrombolysis (PHTL) was associated with a 17% reduction in mortality compared to nosocomial thrombolysis, especially in the case of initiation in the first 2 hours from the onset of symptoms. The presented data, as well as data from recent studies, support the prehospital initiation of thrombolytic therapy when choosing this reperfusion strategy [9]. If the medical and paramedic staff can interpret the ECG on the spot or remotely transfer the registered ECG to the hospital for interpretation, it is recommended to conduct thrombolytic therapy at the pre-hospital stage. The aim is to start thrombolytic therapy within 10 minutes after the diagnosis of STEMI [9-10].Angioplasty and stenting require significant technical equipment and professional training. This method is possible to be performed only in specialized centers. There are data that allow us to state that if, under equal conditions in time, primary percutaneous coronary interventions (PPCI) have advantages over TLT, then every 10 minutes postponements of PPCI reduce survival benefits by 1%. Thus, survival after late PPCI is compared with survival after early TLT. Reducing the time of TLT initiation by 1 hour is accompanied by a decrease in 30-day mortality by 17%. Pharmacological reperfusion (the use of thrombolytic drugs) is the easiest and fastest way to restore blood flow in myocardial infarction. the possibility of its use at the pre-hospital stage gives the additional value to this method [4-5,9-11]. A large American NRMI registry has reflected the effect of time delay on mortality in various categories of patients: only 40 min. delay in reperfusion in patients younger than 65 years with anterior myocardial infarction and the appearance of symptoms less than 2 hours ago increases the risk of death. It is considered that every 10 min. PCI delay reduces survival by 1%, and reperfusion delay by 60 min. increases the risk of death by 17% [12].The aim of the research was to study the clinical efficiency of prehospital thrombolytic therapy in acute ST-segment elevation myocardial infarction.
2. Material and Methods
- 108 acute myocardial infarction patients with ST segment elevation aged from 35 to 67 years from 2019 to 2020 were examined. The mean age was 44.2±1.3 years. The patients were taken by cardio-brigades of the ambulance service to the Bukhara branch of the republican Research Center of Emergency Medicine and hospitalized to the cardiac ICU with a diagnosis of STEMI. ECG revealed elevation of the ST segment in the anterior thoracic leads from 2 to 12 mm in all examined patients. All patients were performed standard therapy (anticoagulants, antiplatelet agents, statins, beta-blockers, nitrates, ACE inhibitors), as well as successful myocardial reperfusion: thrombolytic therapy (TLT) was performed prehospitally in 46.3% of TLT patients, at hospital stage - in 53.7% of patients. Patients were randomized into two groups: group I included 50 patients who received prehospital (PHTLT) and standard therapy. Group II included 58 patients who were performed TLT in the hospital conditions.
3. Results
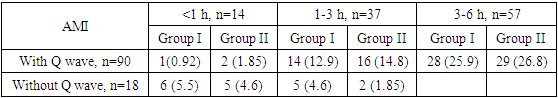
- In 108 patients with acute coronary syndrome with ST elevation (STEMI), the transformation of the diagnosis into a myocardial infarction with a Q wave was observed in 91 (84.2%) cases, without Q myocardial infarction - in 17 (15.8%) patients (Fig. 1).
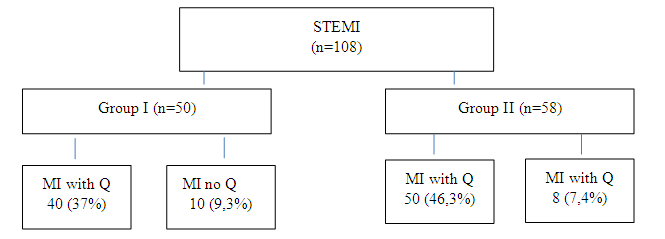 | Figure 1. Analysis of the STEMI diagnosis transformation |
|
|
4. Discussion
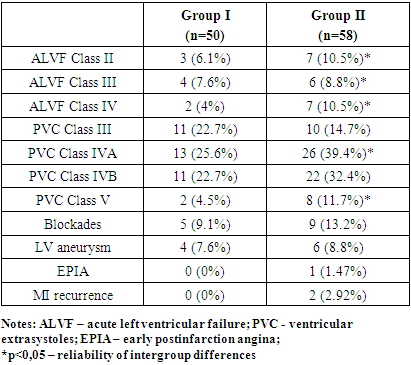
- According to the Eurasian Clinical Guidelines for the Diagnosis and Treatment of acute coronary syndrome with ST segment elevation (2019), when providing maximum care to patients, if possible, it is necessary to deliver the patient within a short time to the PCI-center for performing primary PCI. Data from the RECORD-3 registry, which analyzed data from 21 regions of Russia, showed that primary PCI was conducted in 39% of cases of STEMI, thrombolysis was performed in 32% and a pharmaco-invasive approach was performed in 52% of patients. The register shows that the technical ability to perform PCI on the first day of STEMI, among the centers included in the register, was available in 51% of cases. Almost a third of the patients did not have reperfusion therapy [6].If the estimated time for "ambulance service diagnosis - conduit to the infarct-associated artery (IAA)" exceeds 120 minutes, prehospital TLT (PHTLT) should be performed. At the same time, the optimal/target time " ambulance service diagnosis - conduit to the IAA" should be no more than 90 minutes. In the absence of angiography laboratory and trained personnel and the inability to transfer the patient to a specialized hospital with these capabilities in a short time, TLT is performed. Pre-hospital TLT has an obvious advantage over in-hospital TLT, which reduces the time to start TLT by about an hour, while significantly improving the prognosis. The maximum time from the moment of diagnosis of STEMI to the start of thrombolytic infusion in patients who are not suitable in time for performing primary PCI is up to 10 minutes. This target interval was chosen based on the median of a similar time (9 minutes) recorded in the STREAM study. If the patient is initially hospitalized in a non-invasive center, the time delay for PCI should also not exceed 120 minutes. After TLT all patients should be admitted to the center with angiography. Life-saving PCI is indicated to patients in whom thrombolysis was ineffective (ST segment reduction of less than 50% of the baseline level for 60-90 minutes after the start of TLT) or there are ischemic phenomena, hemodynamic disorders, severe arrhythmias, recurrent anginal pains. Routine PCI should be performed within 2-24 hours after successful thrombolysis. Obviously, if for some reason it was not possible to perform PCI after TLT in these terms, there is every reason to perform PCI at a later period during hospitalization. If the patient is hospitalized in a non-invasive center, the maximum time from the diagnosis of STEMI to transfer to the PCI-center should not exceed 30 minutes [9].When administered in the first two hours from the onset of acute myocardial infarction, thrombolysis has proven to be the best method of early restoration of blood flow to the infarct-responsible artery. The possibility of using thrombolytic therapy at the prehospital stage in the first 60-90 minutes from the onset of acute myocardial infarction is an advantage of pharmacological reperfusion. The drug is administered by an ambulance team or directly by a doctor on the basis of a hospital [2]. According to MINAP data, which included 34,722 patients, prehospital thrombolysis is the most important survival factor. It is worth remembering that the elimination of the occlusion substrate does not cancel the occurrence of residual hemodynamically significant stenosis [11]. Thus, according to D.G. Ioseliani (2004), such stenosis after thrombolytic therapy is observed in 70% of patients. It was also found that even with the restoration of blood flow to the infarct-responsible artery in 8-24% of patients, hemodynamics was significantly impaired. The cause of this phenomenon is probably distal embolization. According to the results of our work, cases of interrupted myocardial infarction (abortive myocardial infarction), a faster decrease in the ST segment on the ECG, which is a sign of restoration of blood circulation at the tissue level were more often observed in the group of patients with prehospital thrombolysis. The rapid destruction of the thrombus and the restoration of coronary circulation with the help of prehospital thrombolysis led to a rapid improvement in the clinical condition of patients, a decrease in the symptoms of acute left ventricular failure. This was due to an improvement in the global function of the left ventricular myocardium after reperfusion. Life-threatening cardiac arrhythmias were significantly less frequently recorded in the group of patients with prehospital thrombolysis. In the group of patients with prehospital thrombolysis, life-threatening cardiac arrhythmias in the form of VT were observed in 2 patients, VF - in 2 patients, and in the control group, VT was observed in 3 patients, VF - in 4 patients. A recurrence of myocardial infarction was developed in 2 patients of the control group; in the group of prehospital thrombolysis they we did not observe myocardial infarction relapses. Early postinfarction angina was observed in one patient of the control group. Hospital mortality in the group of patients with hospital thrombolysis was 1.7%, there were no lethal outcomes in the group of prehospital thrombolysis.
5. Conclusions
- Thus, the transformation of STEMI into various acute forms of coronary artery disease and the development of complications are determined by the degree and speed of the onset of reperfusion in the infarct-associated artery basin. Prehospital thrombolysis in STEMI, accelerating the "symptom-reperfusion" time, positively influenced the clinical course of the disease, contributed to the development of abortive MI, preventing the development of life-threatening complications.The authors declare no conflict of interest. This study does not include the involvement of any budgetary, grant or other funds. The article is published for the first time and is part of a scientific work.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML