Arzieva Gulnora Borievna
Department of Obstetrics and Gynecology №2, Samarkand State Medical University, Uzbekistan
Correspondence to: Arzieva Gulnora Borievna, Department of Obstetrics and Gynecology №2, Samarkand State Medical University, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Pregnant women are not often exposed to thermal injury and very rarely become the object of study. The urgency of this problem in pregnant women is due to the very high rates of maternal and perinatal morbidity and mortality, as well as the great difficulties in providing assistance to severely burned pregnant women.
Keywords:
Thermal injury, Burn, Pregnancy
Cite this paper: Arzieva Gulnora Borievna, The Effect of Thermal Injury on the Course of Pregnancy, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1227-1231. doi: 10.5923/j.ajmms.20221212.11.
1. Introduction
Burn injury is one of the most frequent and most severe types of pathology in peacetime, and, according to the World Health Organization in 2012, ranked 3rd in the overall structure of injuries. Of all types of burns, thermal lesions of the skin are more common, less often - the oral cavity and thermochemical damage to the respiratory tract [1,3]. This is facilitated by the further industrialization of countries, the development of new energy sources, and the widespread introduction into the everyday life of devices created on their basis [2,4].There are domestic and industrial burns. Pregnant women most often get this kind of injury due to exposure to a source of high temperatures. This happens when a woman pours boiling water (hot tea, boiling water from a pot during cooking). These are household burns, they are not as dangerous as chemical burns or those that are caused by radiation damage. In most cases, burns are associated with careless handling of fire and non-compliance with fire safety rules, which ultimately leads to catastrophic consequences.The temperature threshold for the viability of human tissues is 45–50°C. When tissue overheats, irreversible changes (coagulation) of proteins occur, cellular enzymes are inactivated, and metabolic processes are disturbed. The course of the local wound process and the severity of general disorders depend on the mass of tissues that have undergone necrosis.Trauma during pregnancy is the leading non-obstetric cause of maternal death and the most common cause of fetal death [8,10,12,15]. The most common causes of injury during pregnancy include car accidents, falls from a height, violence, stab wounds, burns, electric shocks, and other accidents [2,11,13]. Treatment of patients with burns is one of the urgent problems of modern surgery [1,2]. Burn disease is distinguished by the severity of the course, the difficulty of treatment, and frequent adverse outcomes.Despite the great advances made in the treatment of thermal injury, in recent years, mortality among severely burned patients remains high [8]. Mortality is especially high in critical (40-50% of the body surface) and supercritical (over 50%) deep burns [5].Various concomitant diseases and environmental factors significantly affect the course of burn disease. In the literature, there are single works that highlight menstrual irregularities and premature birth after thermal injury in women. At the beginning of this century, the number of mass catastrophes, military conflicts, and terrorist acts with the defeat of a large number of people has increased. Those affected include women at various stages of pregnancy [5]. Thermal lesions of the skin and thermal inhalation injuries in pregnant women deserve special attention.To date, the tactics of managing pregnant women in the I-II and III trimesters with severe burn injury and an unfavorable prognosis for the life of the mother have not been studied, and it still remains problematic both from a therapeutic and ethical point of view.Here we will focus on the course of burn lesions in pregnant women. Our data and the data cited in the literature indicate great difficulties in assisting severely burned pregnant women. Thus, it can be noted that the reported cases of burns in pregnant women cannot be interpreted as representative. Most of the reports are extremely brief and do not provide information about water and electrolyte imbalance, and the presence or absence of hypoxia, acidosis, or sepsis in patients. None of the reports provided a detailed description of resuscitation measures and methods of fluid transfusion, and the development of shock in the post-burn period was noted only in one case. The paucity of published data on the specific problems associated with burns in pregnancy makes it difficult to determine the most effective method of treating them.The frequency of thermal injury in pregnant women is 6.8-7.8% [10]. Maternal and fetal outcomes depend on the severity of the burn, the presence or absence of complications, and gestational age. In the presence of burns on 25-50% of the body surface, the mortality rate of the mother and fetus is 63%. Closer to the deadline worn pregnancy, delivery should be recognized as an adequate tactic, especially with extensive burns. At the time of initiation, intensive treatment (including airway control) and obstetric tactics (including early delivery) are optimal to improve the prognosis for maternal and fetal health.The first task in the resuscitation and intensive treatment of a pregnant woman with an injury is to stabilize the mother's condition. Only then should attention be directed to the fetus. Monitoring the condition of the fetus helps to determine obstetric tactics during resuscitation, surgery, and the postoperative period [8,13].In the tactics of managing burned pregnant women, the main and controversial issue is the termination or maintenance of pregnancy. The presented materials on the problem of burns in pregnant women do not make it possible to formulate generalizing conclusions, but they show the tragedy of the problem, and its lack of knowledge and stimulate more in-depth clinical research.
2. Materials and Methods of Research
The object of this clinical study was a retrospective study of the course and the results of the complex treatment of 88 affected women of childbearing age with thermal injury, who were in the combustiology department of the City Clinical Hospital No. to 2022.The patients were divided into 2 groups:1. Main group - 48 pregnant women with burn disease.2. Control group - 40 non-pregnant women of childbearing age with burn disease.The average age of patients was 25.4±5.1 years with a range of 19 to 32 years of working age.
3. Results and Its Discussion
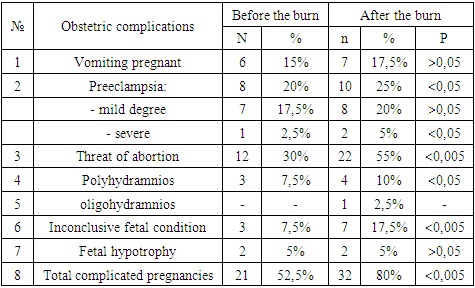
Among the victims of the main group, the first pregnancy was in 7 women, the second - in 38, and the third - in 3 patients. whereas among burnt women of childbearing age (non-pregnant) in history, 25 had one birth, 10 had two, and 3 women had three births.The time of married life in the main group was up to 1 year in 2, from 1 to 2 years in 35, from 2 to 3 years in 3, and more than 3 years in 8 burnt women. In the comparative group, respectively, up to 1 year - in 3, up to 2 years - in 23 and more than 3 years - in 14 victims.The cause of the burn in 57 (64.8%) victims was a flame, of which 27 (47.4%) cases were self-immolation (“living torch”), in 18 (20.5%) cases boiling water and a gas cylinder explosion occurred in 13 (14.7%) pregnant women.According to the area of deep burns, all victims were distributed as follows: there were 3 (3.5%) patients with limited deep burns up to 5% of the body surface. In 45 (51.13%) victims, deep burns spread over an area of more than 30%, of which 8 (9.0%) had severely burned more than 50% of the body surface.Out of 42 (47.7%) patients, 27 (56.3%) of the main group and 15 (37.5%) of the comparative group were diagnosed with TIT of various degrees, mainly in victims who received burns as a result of suicidal attempts.In 32 patients with personality disorders, suicide attempts were more often demonstrative or blackmailing. They took place in the structure of acute affective reactions, during which patients had poor control over their behavior and were vaguely aware of its goals.In most cases, the victims received a severe thermal burn with damage from 45 to 85% of the body surface and the corresponding damage to the respiratory tract (TIT). Due to the great severity of somatic injuries, burn suicides had a high mortality rate - 71.4% (out of 42 - 30 people died).The course of pregnancy before the burn was characterized by some complications in women, the number of which increased sharply after the development of the burn disease. Information about these complications is given in the table.Table 1. The course of pregnancy in patients with burn disease
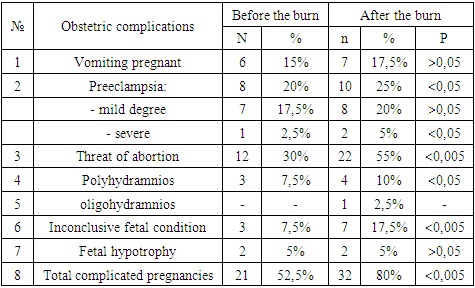 |
| |
|
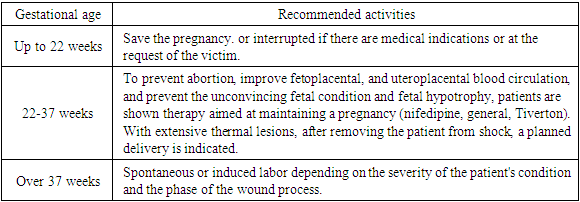
Of the 48 pregnant women with burns, 42 (87.5%) had concomitant somatic diseases: anemia of I-II degree (45.8%), chronic bronchitis (10.4%), chronic pyelonephritis also - 10.4%, hepatosis - 8.3%; others.As you know, the gestational age when receiving a burn is important for the course of OB, as well as the choice of treatment methods and the method of delivery. In 15% of pregnant women, the gestational age was 22 weeks. In 52.5%, the gestation period was up to 37 weeks; the fetus was viable but immature. In 37.5%, the fetus was full-term and morphologically mature. However, it should be noted that some women are delivered later than this date, so the gestational age at delivery has some differences with these data.Burn disease with characteristic symptoms and complications developed in all women with a deep burn area of more than 10% of the body surface. Its severity and outcome depended mainly on the area of deep damage and TIT. The development of burn shock was noted in 40 (83.3%) victims. Burn shock in pregnant women undoubtedly proceeded with more pronounced symptoms. Significant tachycardia, blood pressure lability, impaired diuresis (anuria for 6-9 hours, later oliguria), persistent nausea, and vomiting. The slow exit of patients from a state of shock is characteristic, as a rule, by the end of 3 days. Acute burn toxemia (early psychosis, hyperthermia) was observed in 34 (70.8%) and septic tox mia (sepsis, pneumonia, pyelonephritis) in 27 (77.2%) pregnant women.Almost all pregnant women with thermal injuries had changes in the urine (proteinuria, leukocyturia, microhematuria and cylindric, the appearance of acetone and sugar), anemia and hypoproteinemia developed.An important issue is the assessment of the outcome of trauma for the mother and fetus. As our data show, three pregnant women with II-IIIA degree burns were transferred with a progressive pregnancy to specialized obstetric hospitals. All births were on time. In 5 pregnant women with IIIA-B degree burns, 10-15% b.t. also there was an urgent delivery, which was complicated by the secondary weakness of labor activity. Of the women admitted with deep burns of more than 20% of the body surface, the first half of pregnancy ended in spontaneous miscarriage 1-3 days after the injury in 4 women, on the 4-5th day in 9. Premature birth on the 15-20th day after the injury occurred in 11 women and term delivery in 3 women. In 3 women with a deep burn area of more than 30% of the body surface, who died during the period of septic tox mia, pregnancy 38-39 was not resolved.Based on our experience, the tactics of introducing pregnant women, depending on the duration of pregnancy and the severity of the burn, were as follows.1. With burns of II-IIIA degree of 10-15% and deep burns - 3-5% of the body surface in the I-II trimester of pregnancy, pregnancy should not be interrupted; in the third trimester, with complicated births, they should be carried out in the burn department (with an intensive care and obstetric team) or transferred to an obstetric hospital (depending on its condition, severity, and phase of the burn wound).2. In case of II-IIIA-B degree burns of 10-15% of the body surface in the I-II trimester of pregnancy, an attempt to save the pregnancy, an operation of choice in the first trimester - an artificial abortion after removing the patient from shock, in the III trimester, induction of labor to remove the patient from shock in burn department.3. In case of burns of IIIB-IV degree, 10-15% of the body surface in the I-II trimester of pregnancy should not be interrupted; in the III trimester, delivery of a patient with spontaneous labor; artificial delivery after removing the patient from shock with a live fetus.The most careful attention is required by a woman in the last month of pregnancy; childbirth should be pre-planned for the morning and carried out by a reinforced team in the presence of a pediatrician, neonatologist, and resuscitator. It must be taken into account that the loss of a child can lead a woman to severe depression, which can “negate” all the efforts of doctors, therefore, in the postpartum period, it is necessary to involve a psychiatrist.We want to give an example of a case from practice. We present the following clinical observations.Observation 1st. Severe burn with a favorable outcome for the mother and fetus.Patient P., 27 years old, was admitted to the combustology department of the SFRNCEMMP at 15:30 on January 29, 2019, and transferred from sub-branch institutions, a day after the injury (house fire). Diagnosis: The flame burn of the face, neck, back, arms, and legs is 50% I-III A degree. Severe shock. TIT II degree. Pregnancy II. 32 weeks. Threatening premature birth. Chronic anemia of moderate severity. After 3 hours, she was examined by an obstetrician-gynecologist: from the anamnesis, this pregnancy is the second. The first birth was in 2015 (macrosomia, weakness of the birth forces). This pregnancy proceeds on the background of anemia. Objectively: the abdomen is enlarged due to the pregnant uterus. Palpation determines the longitudinal position of the fetus, head presentation, and presenting part - the head is above in course in the small pelvis, the fetal heart rate is 140 beats per minute, and the uterus is in good shape. Vaginal discharge is mucous. Pregnancy-preserving therapy was prescribed: no-shpa, nifidipine according to the scheme, and indomethacin suppositories. With the development of labor activity, a transfer to a maternity hospital is recommended. Considering the severe state of shock of the pregnant woman, hemotransfusion and plasma transfusion were started. Wound dressings were performed under inhalation anesthesia (Trilene, nitrous oxide, halothane). On the 6th day after the injury, the condition of the pregnant woman improved, the uterus was in a normal tone, and the fetal heart rate was 145 beats per minute. Despite the pregnancy-preserving therapy, on the 13th day after the injury, labor began, and therefore she was transferred to 17 hours 45 minutes. 02/11/2019 to the maternity hospital. 12.02.2019 at 00.15 minutes, premature birth occurred with an immature male fetus weighing 2700 g, 46 cm tall, with an Apgar score of 7-8 points. The total duration of labor was 5 hours 25 minutes, blood loss was 200 ml, and there were no complications during labor. the puerperal was transferred to the burn department: her condition was grave, her body temperature was 38.3°C, her pulse was 110-115 beats per minute, her respiratory rate was 27-28 per minute, and her blood pressure was 130/90 mm Hg.The course of the burn disease was complicated by left-sided focal pneumonia, an abscess of the left lung. Conducted antibiotic therapy with a positive effect. Autodermoplasty was performed three times: 700,150 and 40 cm2 of skin. The patient was discharged home on April 29, 2019, in satisfactory condition. Bed days amounted to 91 days.Observation 2nd. Patient S., 30 years old, was admitted to the clinic on December 4, 2019, at 11:00 am with a diagnosis of Flame burn II-IIIAB degree 40%, face, head, neck, trunk, and extremities. Burns of the upper respiratory tract (TIT II-degree). Severe burn shock. Pregnancy 31-32 weeks. It took 8 hours from the moment of injury to hospitalization. It is noteworthy that the patient was initially taken by ambulance to the clinic of the Department of Obstetrics and Gynecology of the Samarkand Medical Institute, where hospitalization was denied due to a burn injury. BP 115/100 mm Hg, pulse -126 beats per minute, respiratory rate - 20 per minute. Immediately upon admission to the clinic, anti-shock measures were started: intravenous glucose solutions, Ringer-Locke, reopoliglyukin, mannitol, soda solution, and albumin. The volume of infusion was 2500 ml, 800 ml of water and 1500 ml of soda-salt solution were drunk. Diuresis was 1450 ml. On the 2nd day, plasmapheresis was performed - 1200 ml of plasma, 600 ml of Ringer's solution, 500 ml of plasma, and 100 ml of 10% albumin were injected intravenously. Examined by a gynecologist: from the anamnesis of pregnancies - 3, childbirth - 2 and 1 honey. abortion. Objectively: the uterus is in good shape, the position of the fetus is longitudinal, the presenting part - the head is located above the entrance to the small pelvis, and the fetal heartbeat on the right below the navel is 130 beats per minute. Pregnancy-preserving therapy was prescribed: no-shpa, nifidipine, indomethacin suppositories, and valerian infusion. In the cytology of the vaginal smear, signs of a threatened abortion by the type of hyperestrogenism were found. On the 2nd day after the injury, the pregnant woman was transferred to the maternity hospital for delivery. On December 7, 2019, at 22:10, a premature birth occurred, a boy weighing 2800 g, and a height of 47 cm was born. The total duration of labor was 7 hours 30 minutes, blood loss-350 ml. There were no complications during childbirth.An analysis of our observations allows us to state that the determining factor in the outcome of the injury for the mother and fetus is the severity of the burn injury, which is mainly due to the area of the deep (III B-IV stage) burn. Superficial burns do not affect the course of pregnancy and fetal development. There were no superficial burns of a large area (more than 10%) in this study. Deep burns of more than 10% of the body adversely affect the mother and fetus. Any infection is dangerous for a pregnant woman, therefore, when receiving such an injury, it is necessary to provide emergency assistance correctly and carefully care for damaged skin. Based on the analysis of the clinical data of the course and outcome of pregnancy with thermal injury, the following tactics for managing these patients are proposed, depending on the gestational age at the time of the burn.Table 2. Tactics of managing pregnant women with burns depending on the duration of pregnancy
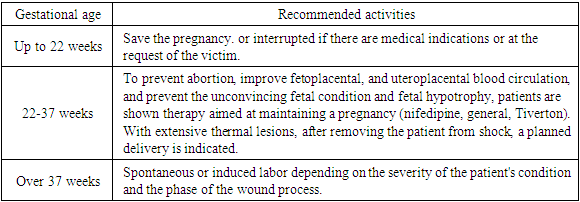 |
| |
|
4. Conclusions
Thus, the introduction of standards into the practice of emergency medicine action based on the principles of evidence-based medicine is appropriate to help those burned. Diagnostic and treatment standards for this category of victims are especially important at the stage of resuscitation and intensive care. It should be noted that much attention is paid to standards in modern literature, but there are practically no standards for patients with burn injuries.
References
| [1] | Арзиева Г.Б., Карабаев Х.К., Негмаджанов Б.Б. и др. Беременность и ожоговая травма. // «Медицина и качество жизни» Москва. 2012., №3, с.14-15. |
| [2] | Арзиева Г.Б., Карабаев Х.К., Негмаджанов Б.Б. и др. Оптимизация ведения беременных женщин в остром периоде ожоговой болезни. Методические рекомендации. Самарканд. 2012., 16 с. |
| [3] | Алексеев А.А., Бобровников А.Э. «Эрозивно-язвенные поражения желудочно-кишечного тракта и кровотечения из них у пострадавших с ожогами». Мат. Всероссийская конференция с международным участием. «Актуальные вопросы комбустиологии». Сочи 1-5 октября 2019. с 3-5. |
| [4] | Крылов К.М., Крылов П.К. Скорая медицинская помощь при термической травме. // Мат. 18-го Всероссийского конгресса посвященного 120-летию скорой медицинской помощи в России //. Санкт-Петербург, 30-31 мая 2019 г. - с. 71. |
| [5] | Парамонов Б.А., Порембский Я.О., Яблонский В.Т. Ожоги. Руководство для врачей. Санкт-Петербург, Спец Лит, 2016 -170 с. |
| [6] | Чурилов А.В., Кушнир С.В., Фисталь Н.Н.и др. Тактика ведения беременных с термическими поражениями. // Скорая медицинская помощь,Российский научно-прак. журнал. 2006. Т.7. -№3 -с.100-101. |
| [7] | Хаджибаев А.М., Фаязов А.Д., Уразметова М.Д. и др. Клинико-иммунологическая эффективность применения культивированных аллофибробластов в лечении обожженных с комбинированными поражениями. Вести экстренной медицины. 2014; 1: 40-44. |
| [8] | Chang J., Berg C.J., Saltzman L.E., Hern-don J. Homecide: A leading cause of injury deaths among pregnant and postpartum wonen in the United States 1991-1999 // Am. J. Public. Health. 2015; 95: 471-477. |
| [9] | Driscoll P., Wardrope J. ATLS: Past, present, and future // Emerg. Med. J. 2015; 22: 2-3. |
| [10] | Grady K., Howell C, Cox C. Managing Obstetric Emergencies and Trauma // London, Royal College of Obstetricians and Gynaecologists Press, 2017. |
| [11] | Howell P. trauma. In Chestnut D.H. (ed). Obstetric Anesthesia: Principles and practice. Fourth Edition, Mosby. 2009; 1149-1163. |
| [12] | Lewis G., editor. The Confidential Enquir into Maternal and Child Health (CEMACH): Saving Mother՚s Lives: Reviewing Maternal Deaths to MakeMotherhood Safer – 2013-2015. The Seventh Report Confdential Enquiry into Maternal Deaths in the United Kingdom. London, CEMACH, 2017. |
| [13] | Metz T.D., Abbott J.T. Uterine trauma in pregnancy after motor vehicle crashes with airbag deployment: A 30-case series // J. Traume. 2006; 61: 658-661. |
| [14] | Nolan J.P. Advanced trauma life support in the United Kingdom: Time to move on // Emerg. Med. J. 2005; 22: 3-4. |
| [15] | Patteson S.K., Snider C.C., Meyer D.C. The consequences of high-risk behaviors: Trauma during pregnancy // J. Trauma. 2007; 62: 1015-1025. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML