-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1223-1226
doi:10.5923/j.ajmms.20221212.10
Received: Nov. 19, 2022; Accepted: Dec. 5, 2022; Published: Dec. 9, 2022

Effect of Intraoperative Sedation in Women under Spinal Anesthesia on Cognitive Functions in the Postoperative Period
Matlubov Mansur Muratovich, Khudoyberdieva Gulrukh Sobirovna, Mamaradjabov Sobirzhon Ergashevich
Samarkand State Medical University, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

One of the most discussed problems in modern anesthesiology is cognitive dysfunction associated with surgery and anesthesia. Cognitive impairments after surgery are common and undesirable phenomena, and interest in them is accompanied by an increase in the number of scientific papers published recently [1].
Keywords: Postoperative cognitive dysfunction (POCD), Dexmedetomidine, Spinal anesthesia, Sedation, RASS score, MMSE score
Cite this paper: Matlubov Mansur Muratovich, Khudoyberdieva Gulrukh Sobirovna, Mamaradjabov Sobirzhon Ergashevich, Effect of Intraoperative Sedation in Women under Spinal Anesthesia on Cognitive Functions in the Postoperative Period, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1223-1226. doi: 10.5923/j.ajmms.20221212.10.
1. Introduction
- Postoperative cognitive dysfunction (POCD) is a cognitive disorder that develops in the early and persists in the late postoperative period, clinically manifested as memory impairment, difficulty concentrating, and disorders of other higher cortical functions (thinking, speech, etc.) [2,5]. In recent years, there have been reports that there is a certain correlation between the drugs used for anesthesia and POCD, which makes it possible to reduce the risk of cognitive impairment by optimizing anesthesia care. In 2011, the European Medicines Agency conducted a study and approved the use of dexmedetomidine (Quanadex) as a highly selective alpha-2 adrenoceptor agonist, and it is proposed as a sedative, anxiolytic and analgesic drug during general, regional anesthesia and sedation of patients in intensive care units. therapy [3]. At the same time, modern studies prove that maintaining minimal sedation in patients with severe respiratory dysfunction, including those with acute respiratory distress syndrome (ARDS), allows them to achieve earlier activation, reduce the risk of delirium and accelerate recovery [8].Despite a large number of studies on the use of dexmedetomidine, there is currently no consensus and clinical protocols for the prevention and treatment of postoperative cognitive impairment in women after cesarean section.
2. Objective
- To investigate the effect of sedation with dexmedetomidine during spinal anesthesia on the incidence of POCD after abdominal delivery.
3. Materials and Methods of Research
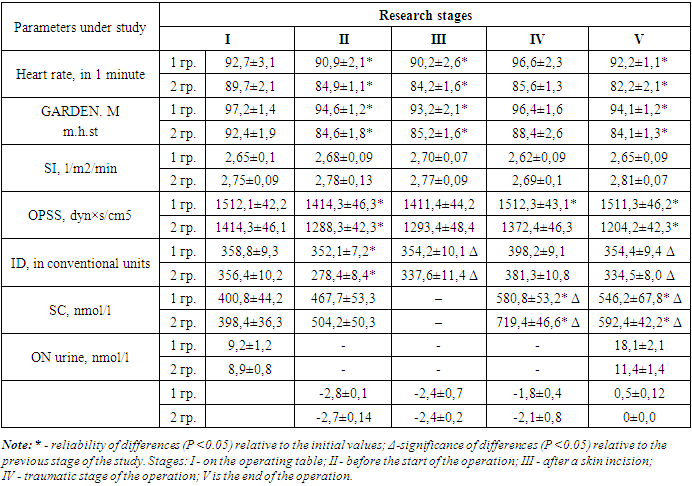
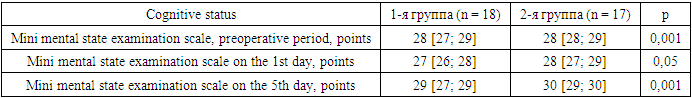
- To fulfill the tasks set based on the regional perinatal center (Samarkand) in the period 2021 to 2022, 35 women were examined and delivered by planned cesarean section with a gestational age of 37-40 weeks. Indications for abdominal delivery were: a scar on the uterus after cesarean section, congenital or acquired pathology of the pelvic bones, preeclampsia, and high myopia. At the same time, the inclusion criteria were the absence of neurological symptoms and brain damage. The exclusion criteria were: massive blood loss (more than 30% of BCC), eclampsia, chronic nonspecific and acute lung diseases, cardiovascular diseases, morbid obesity, the patient's refusal to undergo SA, as well as patients with fluctuations in blood pressure (intraoperative decrease in blood pressure by 30% from baseline or more), hemodynamic instability, and those requiring vasopressor support were excluded from the study. All patients were examined by an anesthetist before surgery and were ASA grade II. All pregnant women gave written informed consent for anesthesia and research. All pregnant women underwent standard preoperative preparation: compression bandaging of the lower extremities, and preliminary infusion of sodium chloride solution 0.9% - 500 ml.The study groups were comparable in terms of baseline variables, including age, weight, ASA physical status (grade II), gestational age, and extragenital pathology. Also, there were no significant differences in the perioperative period (sensory level of anesthesia, duration of surgery, intraoperative infusion, and blood loss), the duration of surgery ranged from 30–40 minutes.All women were divided into groups II. In group, I (n = 18), sedation with ketamine (1 mg/kg) was performed. Puncture of the subarachnoid space was performed at the LII–LIV level with Pencil-Point G 25–26 needles in the lateral position. Slowly (within 2 minutes) a hyperbaric solution of 0.5% bupivacaine solution with a solution density of 1.026 was introduced. The anesthetic dose was calculated according to the suggested dosage [3]. In group II (n = 17), starting from the moment of premedication, 0.5 µg/kg dexmedetomidine (Kvanadex, Yuria Pharm) was intravenously administered as a sedative for 15 minutes, the maintenance dose of which was 0.5–0. 8 mcg/kg / h throughout the operation until its completion. Techniques and preparations for spinal anesthesia were carried out by the forefathers of the 1st group of women.The effectiveness of analgesia was judged by generally accepted clinical signs. The level of sensory block was assessed by the loss of tactile sensitivity (test - "pin prick"). The upper limit of the blockade was evaluated after its stabilization. The R. Bromage scale was used to assess the depth of motor blockade (HMB).The depth of the motor and the sensory block was assessed using the Bromage scale and the verbal rank scale, respectively.According to scale Bromage motor blockade was defined as follows:0 points - the patient can lift and hold the leg straightened in the knee joint;1 point - the patient can lift and hold only the leg bent at the knee joint;2 points - the patient cannot raise the leg, however, flexion in the hip and knee joints is possible;3 points - the patient can move only in the ankle and first metatarsophalangeal joints;4 points - movements in the lower extremities are impossible. [9]. Cortisol is the main representative of the group of glucocorticoids, which directly or indirectly regulate almost all physiological and biochemical processes. The range of application of these steroids is very wide, the main targets are the liver, muscles, lymphoid tissue, cells of the central nervous system, and adipose tissue. Cortisol is synthesized in the adrenal cortex. However, during pregnancy, it is a hormone of the fetoplacental complex, because. its formation is with the participation of the placenta, liver, and adrenal glands of the fetus. Cortisol during pregnancy, in addition to its usual effects in the non-gestational period, also performs several additional functions [10].Central hemodynamics was studied by echocardiography using the SA-600 device from Medison. The stroke index (SI), cardiac index (CI), total peripheral vascular resistance (TPVR), mean dynamic pressure (DPP), heart rate (HR), and blood saturation (SpO2) were monitored using a Schiller monitor. The adequacy of anesthesia was assessed by the stress index (TI), using a mathematical analysis of the heart rate [6], by the level of total cortisol (SC) in the blood plasma (radioimmune method). The study of the effectiveness and depth of spinal anesthesia was carried out in 4 stages: 1 - on the operating table; 2 - before the skin incision; 3 - in the most traumatic stage of the operation (fetal extraction, revision of the abdominal cavity); 4 - after the end of the operation.Cognitive functions were assessed using the Mini-Mental State Examination (MMSE) scale. This scale is a set of 11 tests that assess orientation in time and place, word repetition, counting, auditory memory, naming objects by the display, phrase repetition, command comprehension, reading, writing, and drawing. This is a fairly reliable tool for the primary screening of cognitive impairment, including dementia. The depth of sedation was controlled using the RASS scale and maintained at -2, -3. The severity of psychomotor agitation and the depth of sedation was assessed using the RASS scale (Richmond Agitation-Sedation Scale). Its advantage lies in the fact that it is easy to use, as it takes into account the available parameters based on the assessment of the patient's mental status, and a clear gradation according to the degree of depression of consciousness allows timely adjustment of therapy, avoiding excessive or insufficient sedation. The RASS score is mandatory to verify delirium.Statistical analysis of the obtained data was carried out using the Microsoft Excel 2013 software package (Microsoft Corporation, USA). The significance criterion was the value of the error probability index or the probability of accepting an erroneous hypothesis (p) - no more than 5% (p ≤ 0.05). The results obtained are presented in the table.Results of the study and their discussion: as our studies showed, SA was highly effective in all 35 women. The level of distribution of a complete sensory-motor block corresponded to Th4-S5 dermatomes.During the entire operation, including its most traumatic stages, the patients did not react and did not complain. No signs of depression were observed. SpO2 was 96-98%. Hemodynamic stability was maintained (see Table 1). However, when assessing changes in hemodynamics in the 1st group, in contrast to the 2nd group of women, an increase in heart rate (HR) from 90.2±2.6 beats/min to 96.6±2.3 beats/min was found, an increase in SBP at all stages of observation, a slight decrease in cardiac index (CI) and an increase in TPVR.During gestation, there is an increase in the amount of cortisol, which is physiological for the period of pregnancy, due to an increase in the content of transcortin [11]. This level of this glucocorticosteroid is necessary to meet the increased metabolic needs of the body of a pregnant woman by activating carbohydrate synthesis and lipolysis. Cortisol controls glucose transport across the placenta. In addition, the hormone is important for the formation of enzyme systems of the liver, the epithelium of the small intestine, and fetal lung cells: the development of the alveolar epithelium and the secretion of surfactant, which contribute to the expansion of the lungs during the first breath [12].The activation of the sympathetic link of regulation was also the highest in the 1st group of women when using ketamine, while the tension index (TI) was 398.2±9.1 c.u. at the most traumatic stage of the operation, however, there was a low content of total cortisol (SC) of 580.8 ± 53.2 nmol/l in women of the 1st group, such The phenomenon was regarded by us as a manifestation of the deep sedative effect of ketamine (see Table 1). After fractional administration of ketamine (1 mg/kg) (I group) and a 15-minute intravenous loading dose of quanadex (0.5 μg/kg) (II group), in patients of group I, the degree of sedation was observed - 2.8 ± 0.27, while in the second - 2.5±0.19 points. At the height of anesthesia before the skin incision, RASS in group I increased by 7.4% to moderate, and in group II it decreased, respectively, by 8.2% (P>0.05) to a mild degree. After extraction of the fetus RASS, I gr. increased by 10.4% (P0.05) by the end of the operation and 4 hours after its completion decreased by 8.7 (P>0.05) and 70.8% (P 0.05), respectively, relative to the initial stage. In group II, the degree of sedation at all stages of the study according to RASS remained stable within the limits of –2.1 and –1.8 points (P>0.05) (see Table 1).
|
|
4. Conclusions
- The use of 0.5 μg/kg dexmedetomidine as a sedative against the background of SA provides hemodynamic stability throughout the operation and is quite acceptable for anesthetic management of abdominal delivery. The use of dexmedetomidine leads to a decrease in the frequency of cognitive impairment in the early postoperative period, a decrease in the intensity of the pain syndrome, and a favorable effect on recovery and activation after surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML