-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1218-1222
doi:10.5923/j.ajmms.20221212.09
Received: Nov. 11, 2022; Accepted: Dec. 3, 2022; Published: Dec. 9, 2022

Complex Treatment of Dysplatic Coxarthrosis
Mamatkulov Oybek Khalikovich
Director of the Samarkand Branch of the Republican Scientific Practical Center of Traumatology and Orthopedics, Samarkand, Uzbekistan
Correspondence to: Mamatkulov Oybek Khalikovich, Director of the Samarkand Branch of the Republican Scientific Practical Center of Traumatology and Orthopedics, Samarkand, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Dysplastic coxarthrosis (DKA) accounts for 40-87% of cases of pathology of the hip joint. This disease is common in 7-25% of the adult population in Europe. Pathology develops due to congenital underdevelopment of HJ structures, it is a chronic progressive degenerative-dystrophic process and healthy joints. Material and research methods. In the period 2011-2022, we operated on 397 patients. The method of examining patients with lesions of the hip joint includes a complex of methods: clinical, radiological, functional, laboratory, densitometric, biomechanical and computed tomography. After these comprehensive studies, the goal of our study is determined - determining the stage of DKA, choosing the optimal treatment method, preoperative planning and performance of the operation, followed by restoration of the function of the operated limb. When examining patients, the long-term results of total arthroplasty showed a significant decrease in pain, elimination of a shortened limb, an increase in range of motion and an improvement in gait. 6 months after total arthroplasty, many patients did not notice pain syndromes when walking, moving, or it was of a periodic nature when moving over long distances, or after prolonged physical exertion. Analysis of long-term results showed total hip arthroplasty, which confirms the correct theoretical validity and high efficiency of complex treatment of DKA and positive results of arthroplasty.
Keywords: Dysplasia, Dislocation of the femoral head, Coxarthrosis, Hip joint, Complex treatment, Total arthroplasty, Revision arthroplasty
Cite this paper: Mamatkulov Oybek Khalikovich, Complex Treatment of Dysplatic Coxarthrosis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1218-1222. doi: 10.5923/j.ajmms.20221212.09.
Article Outline
1. The Relevance of Research
- Dysplastic coxarthrosis (DKA) accounts for 40-87% of cases of pathology of the hip joint (HJ) (Zagorodniy N.V., 2012; Khmara A.D., Norkin I.A., Khmara T.G., 2012; Tugizov B.E., 2013; Polulyakh M. V. et al., 2014; Anisimova E. A. et al., 2014; 2015). This disease is common in 7-25% of the adult population in Europe. Pathology develops due to congenital underdevelopment of HJ structures, it is a chronic progressive degenerative-dystrophic process and healthy joints (Akhtyamov I.F., Sokolovsky O.A., 2008; Lebedev V.F., Dmitrieva L.A., Arsentiev L.I. , 2013; Anisimova E.A., et al., 2014).TETBS (TETBS) is the main treatment for the last stages of dysplastic coxarthrosis, when conservative treatment does not help the patient. Therefore, total arthroplasty is a topical issue in the treatment of patients with DKA. Total arthroplasty in a patient with DKA can lead to unsatisfactory long-term results of treatment and a consequence of early revision arthroplasty. Thus, in the treatment of patients with DKA, there is a need for more accurate individual preoperative planning of total arthroplasty and the choice of the shape and size of the femoral component of the endoprosthesis.
2. The Purpose of the Study
- The use of complex treatment and increase in the results of TETBS in patients with DKA.
3. Material and Research Methods
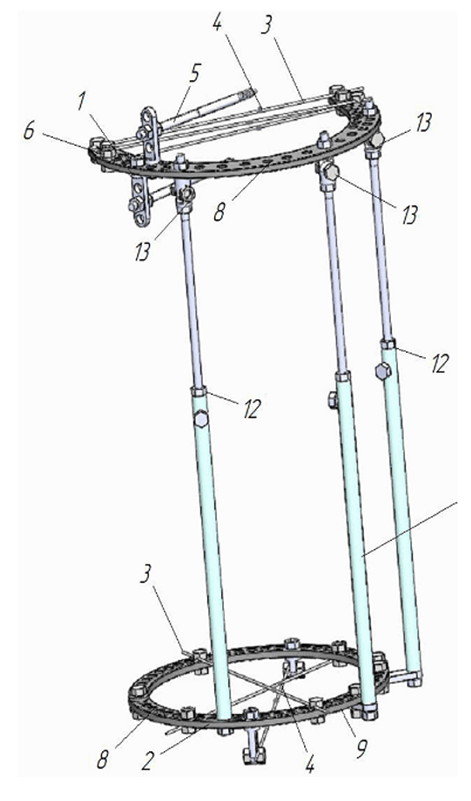
- In the period 2011-2022, we operated on 397 patients.The method of examining patients with lesions of the hip joint includes a complex of methods: clinical, radiological, functional, laboratory, densitometric, biomechanical and computed tomography. After these comprehensive studies, the goal of our study is determined - determining the stage of DKA, choosing the optimal treatment method, preoperative planning and performance of the operation, followed by restoration of the function of the operated limb.In our center, the treatment of DKA with unilateral congenital high dislocation of the hip is carried out in two stages, first, the femoral head was brought down to the level of the acetabulum, and the second stage was TETBS.In TETBS with congenital unilateral high dislocation of the hip, the problem of total arthroplasty arose, since shortening of the limb from 5 to 10 cm was observed, and for this2 treatment patents were developed in our center: 1) A patent for “Device for lowering the femur before endoprosthetics” was developed and received (patent RU 27600081С1. Published: 22.11.2021) (Fig. 1.). 2) Developed and received a patent for “Method for the treatment of dysplastic coxarthrosis” - (patent RU 2763654C1. Published: 12/30/2021). (Fig. 2.).
 | Figure 1. Patent for “Device for lowering the femur before arthroplasty” - (patent RU 27600081С1. Published: 22.11.2021) |
 | Figure 2. Patent for “Method of treating dysplastic coxarthrosis” - (patent RU 2763654С1. Published: 12/30/2021) |
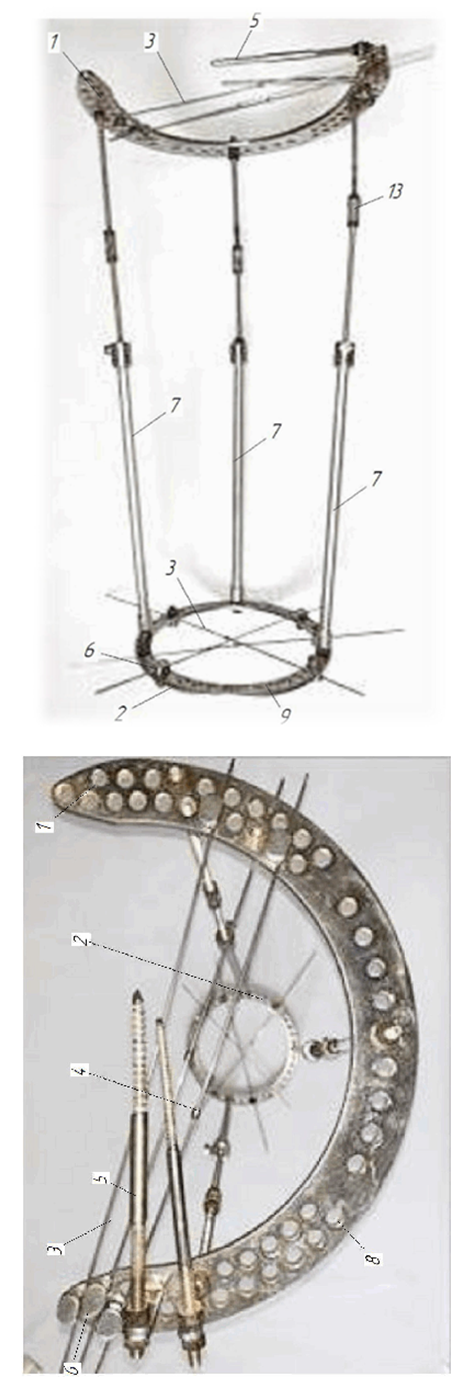 | Figure 3. 1 modification of our invention |
 | Figure 4 |
4. Operation Technique
- 1-stage operation; After spinal anesthesia, the patient is placed on the operating table on his side and three times treatment is performed. operating field with an antiseptic. In the anterior-superior iliac spine the bones were guided by three intersecting wires with soldering in the direction from the anterior-superior iliac spine to the posterior part of the iliac wing. The conductor was drilled on the knitting needles and the rod was passed on the knitting needle, the knitting needles were passed through the rod, the second rod was passed parallel to the first one. The wires and rods passed through the ilium were fixed in the 180*-220* degree arc of the Ilizarov apparatus. In the area of the lower third of the femur, three wires with soldering were inserted, and the wires fixed the 140*-160* degree ring of the Ilizarov apparatus; when the wires were inserted, the knee joint was bent 90*. The arc and ring of the Ilizarov apparatus were connected by three telescopic rods. The hip joint was fixed at 15*-20* degrees of abduction and 5*-10* degrees of flexion. Sterile, alcohol wipes were placed around the needles and rods. After the operation, on the second day, the femur was brought down by 1 mm 2-3 times a day. During distraction, some patients felt pain in the hip joint and lower limb and stopped the distraction process for a couple of days. After the 1st stage of the operation of applying a pin-rod apparatus for lowering the thigh, patients on the second day were allowed to walk on crutches on both legs. Patients were taught distraction on the apparatus and were allowed to go home for 4-5 days and in satisfactory condition. After 2-3 months of distraction, the femoral head reached the level of the acetabulum and 1 week had a break at home. In stationary conditions, the apparatus was removed and aseptic dressings were applied. The second stage was made TETBS. During distraction, some patients felt pain in the hip joint and lower limb and stopped the distraction process for a couple of days. After the 1st stage of the operation of applying a pin-rod apparatus for lowering the thigh, patients on the second day were allowed to walk on crutches on both legs. Patients were taught distraction on the apparatus and were allowed to go home for 4-5 days and in satisfactory condition. After 2-3 months of distraction, the femoral head reached the level of the acetabulum and 1 week had a break at home. In stationary conditions, the apparatus was removed and aseptic dressings were applied. The second stage was made TETBS. During distraction, some patients felt pain in the hip joint and lower limb and stopped the distraction process for a couple of days. After the 1st stage of the operation of applying a pin-rod apparatus for lowering the thigh, patients on the second day were allowed to walk on crutches on both legs. Patients were taught distraction on the apparatus and were allowed to go home for 4-5 days and in satisfactory condition. After 2-3 months of distraction, the femoral head reached the level of the acetabulum and 1 week had a break at home. In stationary conditions, the apparatus was removed and aseptic dressings were applied. The second stage was made TETBS. Patients were taught distraction on the apparatus and were allowed to go home for 4-5 days and in satisfactory condition. After 2-3 months of distraction, the femoral head reached the level of the acetabulum and 1 week had a break at home. In stationary conditions, the apparatus was removed and aseptic dressings were applied. The second stage was made TETBS. Patients were taught distraction on the apparatus and were allowed to go home for 4-5 days and in satisfactory condition. After 2-3 months of distraction, the femoral head reached the level of the acetabulum and 1 week had a break at home. In stationary conditions, the apparatus was removed and aseptic dressings were applied. The second stage was made TETBS.2-stage operation;After spinal anesthesia, the patient is placed on the operating table on his side and the surgical field is treated three times with an antiseptic. In the area of the hip joint, an external-lateral incision was made in the skin and subcutaneous fat. We make a longitudinal incision stretching the fascia lata, a partial incision of the tendons of the gluteus maximus and medius muscles and arthrotomy of the hip joint. After arthrotomy, the femoral head was dislocated, the head was resected at the base of the femoral neck, and the head was removed from the acetabulum with a corkscrew. The head is deformed, underdeveloped and very small in size, 3-4 cm in diameter. The acetabulum is also deformed, flat and small in size, 3-4 cm in diameter. We process the acetabulum with cutters and put probes of the endoprosthesis cup, size-38,40,42,44,46, 48 and after that we put the cup of the endoprosthesis with the insert. In the position of external rotation of the lower limb being operated on, we open the femoral canal with a perforator, expand the femoral canal with small cleavers - 01,0,1,2,3. Insert the stem probe into the femoral canal, insert the neck probe onto the stem probe, and insert the prosthesis head probe onto the neck probe. After that, we set the head into the cup and check the amplitude of movement. The amplitude of movement is; flexion 100*-120*degrees, extension -10*-20*degrees, abduction 40*-60*degrees, adduction 10*20*degrees, external rotation 60*-70*degrees, internal rotation 20*-30*degrees. We remove the probes, insert the stem and head of the endoprosthesis and set the head into the cup of the endoprosthesis. We insert a drain into the wound and sew the wound in layers. On the second day, they were allowed to sit and move on crutches, stepping on both legs, on the 3rd-4th day, the drainage was removed. After two weeks, the sutures were removed from the wound and discharged home without crutches. Control examination after the 1st, 3rd, 6th months, after the 1st, 5th and 10th years.
5. Long-Term Results of Treatment
- We studied the long-term results of total hip arthroplasty in stage 3-4 DKA in the period from 6 months to 10 years. A control study was carried out one month after the operation and then every 3 months. Long-term results after the operation were studied according to the total Harris scale (good, satisfactory and unsatisfactory):1) Long-term good results were obtained in 356 patients (which is 00*), in these patients, after surgery, there is no pain in the hip joint and the range of motion reaches 80-90% of the normative values, the function of the hip joint and the support ability of the limb have recovered.2) Long-term satisfactory results were obtained in? patients (which is 00*), these patients after surgery had moderate pain in the operated joint during walking, the function of the joint was limited (the range of motion was restored by 50-70% of the normative values), the patients used additional support when walking for three to six months.3) Long-term unsatisfactory results were obtained in? patients (which accounted for 1%), in? In these patients, peroneal nerve paresis occurred and, after conservative treatment, the peroneal nerve paresis was eliminated. Do? The patient opened a fistula from the wound, made a revision, necrectomy, drainage, and the fistula was eliminated. Do? After 3 years, the endoprosthesis cup migration was observed in the patient, and after the revision, the endoprosthesis cup was replaced.
6. Conclusions
- When examining patients, the long-term results of total arthroplasty showed a significant decrease in pain, elimination of a shortened limb, an increase in range of motion and an improvement in gait. 6 months after total arthroplasty, many patients did not notice pain syndromes when walking, moving, or it was of a periodic nature when moving over long distances, or after prolonged physical exertion. Analysis of long-term results showed total hip arthroplasty, which confirms the correct theoretical validity and high efficiency of complex treatment of DKA and positive results of arthroplasty.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML