-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1206-1210
doi:10.5923/j.ajmms.20221212.07
Received: Nov. 11, 2022; Accepted: Nov. 28, 2022; Published: Dec. 9, 2022

Sociological Assessment of the Organization of Orthopedic Dental Care for Patients with Excessive Facial Defects
Rizaev Jasur Alimdjanovich, Kubaev Aziz Saidolimovich, Axrorova Malika Shavkatovna
Samarkand State Medical University, Samarkand City, Republic of Uzbekistan
Correspondence to: Kubaev Aziz Saidolimovich, Samarkand State Medical University, Samarkand City, Republic of Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the improvement of clinical and organizational aspects of orthopedic dental care for patients with maxillofacial defects only when there is certain information about the activity of dental institutions in this department. For the first time, statistical data on this type of activity are presented. A sociological survey was conducted among orthopedic dentists working in the Samarkand region.
Keywords: Organization of dental care, Statistics, Social status, Orthopedic treatment
Cite this paper: Rizaev Jasur Alimdjanovich, Kubaev Aziz Saidolimovich, Axrorova Malika Shavkatovna, Sociological Assessment of the Organization of Orthopedic Dental Care for Patients with Excessive Facial Defects, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1206-1210. doi: 10.5923/j.ajmms.20221212.07.
Article Outline
1. Introduction
- Improvement of clinical and organizational aspects of orthopedic dental care for patients with maxillofacial defects can be done only if there is some information about the activity of dental institutions in this department. The analysis shows that there are almost no statistics on this type of activity.Today, orthopedic rehabilitation of this category of patients is the most urgent issue. Defects in the face-jaw area occur with different frequencies and have different development. Usually, they are accompanied by obvious aesthetic and functional disorders. In this case, the orthopedist-dentist is faced with the situation of solving a complex clinical and psychological problem, i.e. restoring the lost functions and an appearance close to the natural appearance.
2. The Purpose of the Study
- The variety of data created the necessary conditions for conducting a sociological survey among orthopedic dentists at the initial stage of the research to identify the most important problems in the organization of their activities in the treatment of patients with acquired maxillofacial defects (OMD).
3. Research Materials and Methods
- In this regard, the first question of the questionnaire was as follows: "Have you come across the orthopedic treatment of patients with maxillofacial defects in your practice?". 83% of respondents answered yes to this question. It was found that 17% of the respondents had no experience with the category of OYuJN patients. The structure of the answers to this question is determined by the clear connection between the experience of treating patients with OYuJN and the experience of dentists-orthopaedists. As work experience increases, the frequency of positive answers to this question increases. This pattern may be due to the fact that the treatment of patients with OYuJN is a complex activity that requires appropriate training, skills, and clinical experience in orthopedic dentistry. In addition, as confirmed by our statistical studies, patients with this pathology are extremely rare. This, in turn, explains that doctors with little work experience do not have the opportunity to face such patients in practice.A psychogenic factor, emotional-stressful situations, anxiety-depressive, dysmorphophobic disorders - this is a typical list of disorders in the emotional-voluntary field in patients with maxillofacial pathology with unsuccessful results of reconstructive surgery, bruxism, etc., during the rehabilitation period after complex dental and orthopedic interventions.In addition, psycho-emotional disorders are involved in the formation of psychosomatic vegetodysfunction syndrome and support the mechanisms of parafunctional disorders of chewing and facial muscles. Among RT methods, needle therapy takes one of the leading places as a physiological correction of disturbances in the psycho-emotional sphere. However, it has been noted that basic methods are not always effective.It is customary to distinguish the following main types of treatment: isotropic - aimed at eliminating etiological factors; pathogenetic - affecting the mechanisms of disease development; symptomatic - eliminating the symptoms of the disease. All of them together form a solid basis for a set of treatment and rehabilitation measures.The basis of the reflexotherapy mechanism is the formation of differential afferent currents from receptors of different modalities located on the skin projection of acupuncture points. These afferent currents change the functional state of various parts of the central nervous system, resulting in changes in sensory thresholds, excitability, psychoemotional and autonomic reactivity, muscle mobility, vascular tone, immunological state, and tissue tropism.An enhanced method of scalpoauricular electroneuroreflexotherapy (SAENRT) was developed.The aim of the study was to substantiate the practical application of the potential SAENRT method for the correction of psycho-emotional disorders in patients with maxillofacial pathology and dental problems.
4. Research Object and Methods
- In the structure of the central nervous system, the limbic system and the limbic-reticular complex control the affective sphere, and emotional reactions. 213 SAENRT method was used to correct anxiety-depressive disorders for reflex activation of the limbic-reticular system of the brain. The effect is on the projection area of the limbic-reticular system of the brain (line MS5 of scalp puncture microsystem) and areas of anxiety, and depression (the first and third quadrants of the auricle according to P. Noj'e cartogram) as well as 28, 25, 34, 26a, 55, 100 auricular points (ms5 scalpopuncture microsystem line) transferred to SAENRT was performed on the "Kadr-16A" device, the electrodes were acupuncture needles, with a pulsed bipolar current with a neurotropic form of "spike-wave" impulse at resonance frequencies of 6, 3, 10, 25, 125, 146Hz with 2 minutes of exposure for each frequency was impressed.Treatment was carried out in 12 patients with the psychosomatic syndrome (bruxism - 4, complicated neuralgia of the trigeminal nerve - 5, post-traumatic neuropathy of the facial nerve with cosmetic defects - 3).Initially, anxiety, internal tension, lack of sleep, fear, low mood, general fatigue, reluctance to communicate with others, and crying were detected in all patients.
5. Results
- Anxiety and depression levels decreased by an average of 25% after 4-5 treatments of SAENRT during psychological testing. No side effects were observed, all patients took the treatment enthusiastically, felt "inner peace" during the treatment, and some even fell asleep. After 8-10 treatments of SAENRT, the positive dynamics stabilized.The duration of sleep increased in the patients, the mood improved, there was no crying, and there was a desire to communicate with other people. It is worth noting that the SAENRT method is performed outside the maxillofacial region, which expands the possibilities of treatment in the presence of operative sutures, orthopedic structures, and apparatus. Thus, the developed SAENRT method is an effective method of treating anxiety-depressive disorders in psychosomatic diseases in dentistry, maxillofacial orthopedics, and surgery.This method is one of the best ways to correct the functional state of the body of patients with maxillofacial injuries. This is because, through the multilevel and multifactorial response of the skin's surface to stimuli, it can produce immune-enhancing, desensitizing, and/or numbing, pain-relieving effects.Has it and regulates the tone of the autonomic nervous system. At the same time, SAENRT not only helps to maintain homeostasis but also stimulates various forms of adaptive activity of the body, it can be considered a promising tool to prevent the development of an immunodepressive state.In the next question of the survey, it was necessary to determine the number of cases of treatment of patients with OJU per year by doctors who answered positively to the previous question. The value of this information depends not only on the experience, age, and place of work of the respondents but also on the establishment of certain relationships. This information, taking into account the representative size and composition of the respondents, makes it possible to make approximate calculations of the cases of orthopedic dental treatment of patients with OYuJN who are not officially registered.As can be seen from the graphic data presented in Figure 1, the largest share (59%) of doctors was obtained with the answer indicating 2 cases of orthopedic treatment of patients with OA per year. In second place was the answer "no more than 1 case per year", which is 37%, and in third place - "3-4 cases". An insignificant share (4%) was obtained with the answer of the respondents indicating 3-4 cases of orthopedic treatment of patients with OA. This distribution clearly shows that patients with such pathology are rare. It should be noted that treatment in dental institutions for orthopedic rehabilitation is rarely available. Based on this, it can be assumed that the redistribution of patients between specialists is carried out following the specialization of these patients by orthopedic dentists in a certain institution.
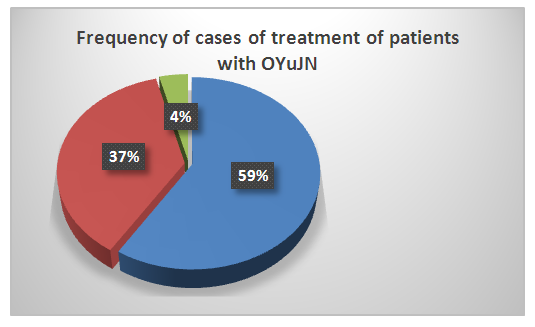 | Figure 1. The structure of answers to the question about the frequency of cases of treatment of patients with OyuJN (59% - 2 cases in 1 year, 37% No more than 1 case in 1 year, 4% 3-4 cases per year |
6. Conclusions
- Thus, the conducted sociological research revealed several problems in the state of medical care for patients with OYuJN existing at the modern stage.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML