Ashurova Maksuda Zhamshedovna, Garifulina Lilya Maratovna
Samarkand State Medical University, Samarkand City, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
106 children with overweight and obese, as well as 30 children with normal body weight were examined. The level of vitamin D in the blood of children was determined. A low supply of vitamin D among school-age children was established, regardless of body weight, the severity of obesity, and gender. It was found that the average level of vitamin D in children with overweight and obese was significantly lower compared to children with normal body weight. It was found that obese children at puberty had a lower level of 25(OH)D. The data obtained require the implementation of special individual therapeutic and prophylactic measures in children with obesity.
Keywords:
Obesity, Overweight, Children, Vitamin D deficiency, Vitamin D deficiency
Cite this paper: Ashurova Maksuda Zhamshedovna, Garifulina Lilya Maratovna, Bone Metabolism and Vitamin D Supply in Children with Obesity, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1201-1205. doi: 10.5923/j.ajmms.20221212.06.
1. Relevance of the Problem
In the last decade, the problem of obesity in children has become one of the most urgent problems of world pediatrics, due to a large complex of concomitant diseases that occur against the background of this pathology. At the moment, there is no doubt that obesity in children concerns the possibility of developing disorders of bone tissue metabolism, followed by the formation of osteoporosis and disabling complications that significantly reduce the quality of life of the child [1,2,3]. The relationship between adipose tissue adipocytes and bone tissue is presented as a homeostatic feedback system, in which adipokines and substances produced by bone tissues serve to form the bone-adipose tissue axis [3,4,5].The biological and clinical effects of vitamin D are closely related to bone metabolism [3,5,6,7]. The lack of vitamin D in the body is necessarily associated with the pathology of bone mineral density [1,3,5,12]. Obesity and vitamin D deficiency, which are widespread in the pediatric population, can be considered potentiating factors with a negative effect on bone metabolism [14].In this regard, we set the goal of the work: to study the status of vitamin D and other indicators of bone metabolism in children with various degrees of obesity.
2. Material and Methods
Our studies were carried out in the family polyclinics No. 1 and 2 of the city of Samarkand, as well as in the regional endocrinological dispensary of the Samarkand region (Uzbekistan). The study involved 106 overweight and obese children with no chronic pathology that can adversely affect calcium-phosphorus metabolism and bone metabolism, aged 7 to 17 years (the average age of children was 11.56±0.23 years) that made up the general group. The control group included 30 practically healthy children, without pathology of the musculoskeletal system with normal body weight.Anthropometric studies were carried out using standard measuring instruments (floor stadiometer and medical scales). Anthropometric measurements included: measurements of height, body weight, and waist and hip circumferences. A comparison of the obtained data and assessment of physical development was carried out according to the summary centile tables of the distribution of height and body weight depending on the age and sex of the WHO for children aged 5–19 years [9]. Based on the measurements performed, the body mass index (BMI) was calculated. The results were evaluated using BMI standard deviations (SDS) according to WHO recommendations.Obesity in children and adolescents should be defined as +2.0 SDS BMI, overweight from +1.0 to +2.0 SDS BMI, and underweight from −1.0 to −2.0 SDS BMI [10].The study of the main indicators of mineral metabolism was carried out based on a single study in the blood serum of the concentrations of total calcium, and phosphorus. As a marker of bone formation in blood serum, we studied the level of alkaline phosphatase (AP) activity using a spectrophotometric method. As a marker of bone resorption, we determined the level of morning calcium in the urine.The determination of 25(OH)D was carried out by the chemiluminescent method using kits and calibrators from Roche Diagnostics (Germany) on an Abbott Architect 8000 analyzer (USA). The evaluation of the results was carried out under the recommendations of the European Society of Endocrinologists (2011) [2]: vitamin D deficiency - 25(OH)D less than 20 ng/ml (less than 50 nmol/l); vitamin D deficiency - 25(OH)D 20-29 ng/ml (51-75 nmol/l); the normal content of vitamin D is 25 (OH) D 30-100 ng / ml (76 - 250 nmol / l).The obtained data were processed using the STATISTICA for Windows software system (version 7, StatSoft, Inc.) and in the environment of the Excel 2016 for Windows package.
3. Research Results
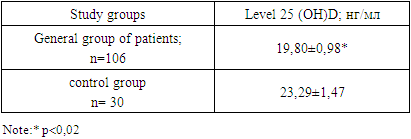
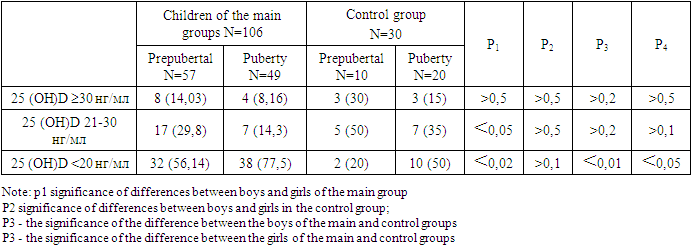
Based on anthropometric data and determination of body mass index (BMI, kg/m²) according to gender and age, it was possible to distribute children into 3 groups: Group I - 39 overweight children (SDS +1.0 to +2.0), Group II 41 children with I-II degree obesity (SDS from +2.0 to +3.0), Group III children with BMI within SDS from +3.0 above, which characterized children with obesity degree 3 and above. The control group consisted of 30 children with BMI SDS -1.0 to +1.0. All children included in the study were residents of the Samarkand region.Following the purpose of our study, we first assessed the vitamin D status of obese children.When carrying out a comparative characteristic of data on the level of vitamin D in the study and control groups, a wide distribution of its insufficiency and deficiency among children of all ages was revealed, while the frequency of these pathological conditions depended on body weight.Thus, in the groups of children of the main groups with overweight and obesity (106 patients), the content of 25(OH)D in serum was 19.80±0.98 ng/ml, which characterized the upper limits corresponding to vitamin D deficiency, and in the control group slightly more than 23.29±1.47 ng/ml, which was the lower limit of 25(OH)D deficiency, but the difference was statistically significant (p<0.02) (Table 1).Table 1. Average vitamin D levels in study groups
 |
| |
|
The distribution according to the degree of vitamin D sufficiency within the main groups and the control group was also almost the same and revealed only a small number of children and adolescents with normal vitamin D sufficiency, both overweight and obese, and with a normal body weight according to age and gender (Table 2).Table 2. Vitamin D sufficiency in overweight and obese children and children with normal body weight
 |
| |
|
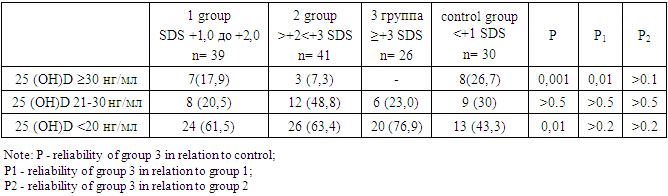
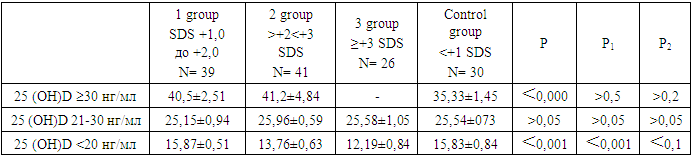
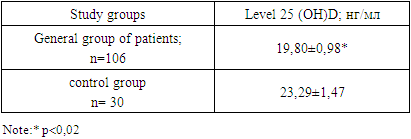
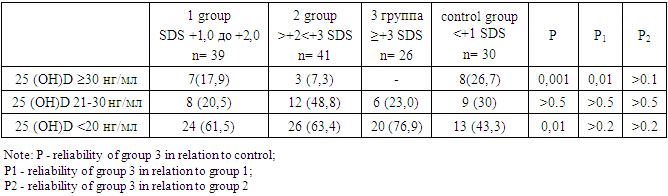
When conducting a comparative analysis, it was revealed that in groups of children with overweight and obesity of varying severity, there was a predominance of patients with vitamin D deficiency. Thus, in the group of children with BMI ≥+ 3 SDS, vitamin D deficiency amounted to ¾ 20 children (76,9%) had 25(OH)D <20 ng/mL, then the remaining ¼ were children with vitamin D deficiency (25(OH)D 21-30 ng/mL) 6 children 23.%, with cases of vitamin D deficiency D within the normal range (25 (OH) D ≥ 30 ng/ml) was not observed.In the second group of children with BMI >+2<+3 SDS, the state of vitamin D deficiency was 2/3 of the number of observations (25 children -61%), while in children of this group there were cases of vitamin D levels within the reference values, which was only 7.3% (3 children), with the incidence of deficiency in 12 children (48,8%).In the first observation group in children with overweight (BMI +1.0 to +2.0 SDS), the distribution of the frequency of occurrence of different levels of vitamin D was similar to that in group 2: 24 children – 61,5% (25 (OH)D < 20 ng/ml), 8 children – 20,5%; (25 (OH) D 21-30 ng / ml), but the frequency of observations of normal vitamin D levels was significantly higher compared with the group of children with grade 3 obesity: 7 children – 17,9% (25 (OH) D ≥ 30 ng /ml) p1<0.01.In the control group, the frequency of children with vitamin deficiency was 1/3 (13 children 43.3%), while only with indicators of children with grade 3 obesity, healthy children showed a significant difference in frequency (p<0.01), and with indicators of the frequency of children in group 2 (p<0.05), while no confidence limits were found in the group of overweight children (p>0.1).The frequency of deficiency and normal levels of vitamin D was distributed almost equally, accounting for 1/3 of the total number of healthy children: 9 children 30% with 25 (OH) D 21-30 ng / ml, and 8 children with 26.7% with 25 (OH) D ≥30 ng/ml. It should be noted that the indicator of the frequency of vitamin D deficiency differed significantly only from the frequency of manifestations of vitamin D deficiency in group 3 (p<0.01), while it did not differ significantly from other groups (p>0.2).This fact suggests that in the group of children with normal body weight, who are also in the 1st and 2nd health groups, there is also a fairly high level of vitamin D deficiency and insufficiency, which requires the adoption of therapeutic and preventive measures even in the group of conditionally healthy children.Thus, comparing the results obtained, it was revealed that the predominant number of examined children living in the Samarkand region had deficiency and vitamin D deficiency. However, in the group of children with vitamin D deficiency and grade 3 obesity (BMI ≥+ 3 SDS), the quantitative values of the median 25(OH) D were statistically significantly lower (12.19±0.84 ng/ml) than in the group of children with deficiency and overweight (15.87±0.51 ng/ml; p<0.001), and in the group of children with vitamin D deficiency and normal body weight (15.83±0.84 ng/ml; p<0.001) (Table 3).Table 3. The values of 25(OH)D in the study groups depending on the degree of its provision
 |
| |
|
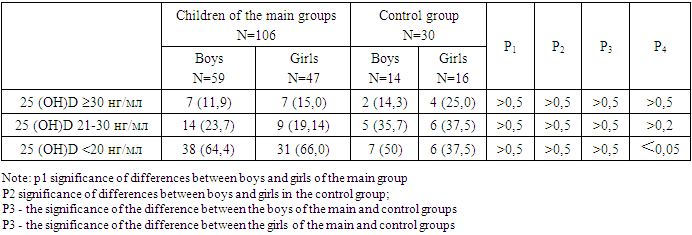
A comparative analysis of the average level of vitamin D in the group with deficiency of this indicator showed a statistically insignificant level in all groups with different body weights.Thus, the average level of 25(OH)D in case of its deficiency in the group of children with BMI ≥+2<+3 SDS was 25.96±0.59 ng/ml, in the group of children with more severe obesity (BMI ≥+3 SDS) 25.58±1.05 ng/ml and almost the same value in the overweight group 25.15±0.94 ng/ml (p>0.05).In children with a normal supply of vitamin D, the average values of vitamin D also did not differ statistically (Table 3).The next step was to analyze the relationship between vitamin D levels and various clinical characteristics of a group of children.When analyzing the content of vitamin D, we obtained gender differences depending on body weight. Thus, 38 (64.4%) boys and 31 (66.0%) girls in the main group had vitamin D deficiency, and 7 (5%) boys and 6 (37.5%) girls in the control group, vitamin D deficiency was observed in 14 (23.7%) boys and 9 (19.14%) girls of the main group of overweight and obese children and 5 (35.7%) boys and 6 (37.5%) girls of the control group, normal content of vitamin D - had 7 (11.9%) boys and 7 (15%) girls from the main group, while it should be noted that among them there were no children from group 3, in which the normal level of vitamin D was not observed (Table 4).Table 4. The frequency of occurrence of varying degrees of vitamin D sufficiency in overweight and obese children of the main groups and controls depending on gender
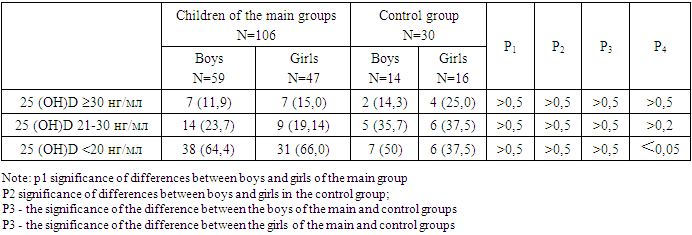 |
| |
|
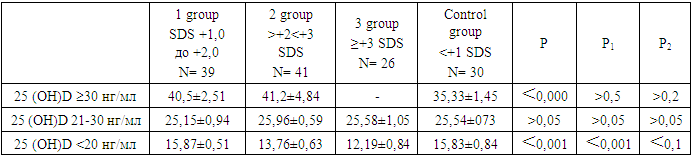
It should be noted that all differences regarding boys to girls, and boys to boys and girls to girls from the main and control groups were not statistically different.When determining the quantitative values of the content of vitamin D in groups with different availability of this vitamin in children from the main and control groups, its level, similar to the above data, also did not statistically differ depending on gender.Since most of the children were in the prepubertal or pubertal stage, we were interested in studying the content of vitamin D levels from the stage of sexual development. It was found that the number of children with different variants of provision with this vitamin differed statistically significantly in the group of children and adolescents with obesity and overweight and prepubertal development (Tanner 0-1), and in the group of children with the same weight pathology who started puberty (Tanner 2 -5).Table 5. The frequency of occurrence of varying degrees of vitamin D sufficiency in children and adolescents with overweight and obesity and control depending on the stage of pubertal development
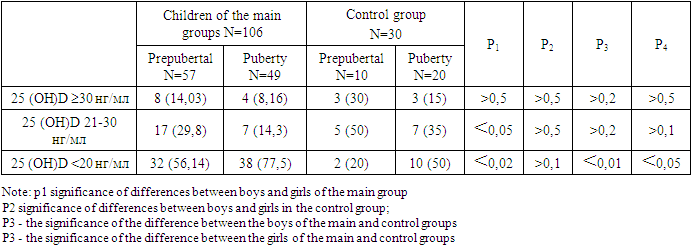 |
| |
|
It was revealed that vitamin D deficiency was predominantly in pubertal children 38 children (77.5%) and only 32 (56.14%) children and adolescents before puberty, which was statistically significant (p<0.05); vitamin D deficiency was detected, statistically significantly more often in the group of children in prepubertal age in 17 children (29.8%) and 7 adolescents (14.3%), respectively, in children in puberty and before puberty (p<0.05), and normal provision with vitamin D occurred in 8 (14.3%) children, mainly in the prepubertal period (4 adolescents 8.16%; p>0.05).According to the difference in the frequency of vitamin D supply depending on the stage of sexual development, the average level of 25(OH)D differed statistically significantly in the main group, where the average level of vitamin D was statistically lower during the period of sexual development (16.7±1.34 ng/ml according to compared with 22.47±1.34 ng/ml, p<0.002). In other cases, namely in comparison in the control group, there was no statistical difference between the prepuberty of the main group and the prepuberty of the control group, puberty in the main and control groups had no statistical differences.Similar data were obtained in other studies when the level of 25(OH)D decreased with the onset and progression of puberty, and this did not depend on body weight [3]. In other studies, data were obtained characterizing differences in vitamin D sufficiency depending on the stage of prepubertal sexual development (Tanner II-IV) in relation to puberty (Tanner I stage) in the group of children with increased body weight, and no differences were found in vitamin D sufficiency. among children with normal body weight in different stages of puberty [1,12].So in our work, in children of the main group with overweight and obesity and the onset of puberty, the lowest values of vitamin D were determined, and in the control group, values close to the norm prevailed in children before the onset of puberty, which suggests that the onset of puberty carries special risks of reducing vitamin D sufficiency.
4. Discussion
Exogenous constitutional obesity, and low vitamin D status are predictors of the development of metabolic risks. In this regard, it is of scientific interest to understand the nature of their mutual influence on the development of metabolic disorders, including disorders in the metabolism of bone formation. In modern literature, there is an ongoing discussion about the causal interaction of these conditions. Thus, an excess of adipose tissue can affect the increase in deposition, catabolism, as a result, an increase in the number of biologically inactive forms of vitamin D, while liver steatosis inevitably associated with obesity, expectedly reduces the activity of enzymes involved in the stages of hydroxylation of precursor forms of this vitamin [6,7,8]. The foundations laid in childhood are realized in the adult period in the form of various chronic pathologies, in this regard, we studied the status of vitamin D, namely in childhood.The results obtained showed that vitamin D deficiency and insufficiency are widely present in children, regardless of body mass index and gender. At the same time, there was a dependence on more severe cases of vitamin D deficiency in the group of children with 3 degrees of obesity, and the average level of vitamin D was statistically different from control indicators. The average level of vitamin D in the comparison groups, depending on the degree of vitamin D deficiency, was associated with the severity of obesity, while quantitatively vitamin D deficiency was statistically different depending on the degree of obesity in children.A low supply of vitamin D to puberty children was established, regardless of body mass index, and gender. At the same time, children with obesity and the onset of sexual development had the lowest vitamin D supply.
5. Conclusions
Thus, a low vitamin D supply was established among school-age children, regardless of body weight, the severity of obesity, and gender. At the same time, the average level of vitamin D in children with overweight and obese was significantly lower compared to children with normal body weight.It was found that obese children at puberty had a lower level of 25(OH)D when it was deficient.The statistically high level of children with vitamin D deficiency and a significant decrease in the average level of 25(OH)D in children with various degrees of obesity contribute to the inclusion of these children in the risk group for the development of bone mineralization pathology and require special individual therapeutic and preventive measures.
References
| [1] | Obesity and bone health: A complex link / J. Hou, C. He, W. He [et al.] // Front Cell Dev Biol. – 2020. – Vol.8. – P.60-81. |
| [2] | Национальная программа «Недостаточность витамина D у детей и подростков российской федерации: современные подходы к коррекции» / Союз педиатров России [и др.]. – М.: Педиатръ, 2018. – 96 с. |
| [3] | Недостаточность витамина D и ожирение у детей и подростков: насколько взаимосвязаны две глобальные пандемии. Роль витамина D в патогенезе ожирения и инсулинорезистентности (часть 1) / Л.Я. Климов, И.Н. Захарова, В.А. Курьянинова [и др.] // Медицинский совет. – 2017. – №. 19. – С. 214-220. |
| [4] | Каладзе Н.Н. Показатели костного метаболизма и жирового обмена у детей с избыточной массой тела / Н.Н. Каладзе, Н.Н. Скоромная // ТМБВ. - 2016. - №1. - С.45-50. |
| [5] | Ларионова М.А. Костный метаболизм у детей и подростков с ожирением / М.А. Ларионова, Т.В. Коваленко // Сахарный диабет – пандемия XXI. Сборник тезисов VIII(XXV) Всероссийского диабетологического конгресса с международным участием. – 2018. – С. 514-515. |
| [6] | Крутикова Н.Ю. Современные представления о влиянии жировой ткани на регуляцию костного метаболизма / Н.Ю. Крутикова, А.С. Ефременкова // Практическая медицина. – 2020. – Т.18. - №6. – С.69-72 |
| [7] | Майлян Э.А. Регуляция витамином D метаболизма костной ткани / Э.А. Майлян, Н.А. Резниченко, Д.Э. Майлян // Медицинский вестник юга России. – 2017. – № 8. – Т.1. – С. 12-20. |
| [8] | Мальцев С.В. Витамин D, кальций и фосфаты у здоровых детей и при патологии / С.В. Мальцев, Н.Н. Архипова, Э.М. Шакирова. – Казань, 2012. – 120 с. |
| [9] | Ожирение и избыточный вес. Информационный бюллетень.: сайт. - Октябрь, 2017 г. – URL: http://www.who.int/mediacentre/factsheets/fs311/ru/ (дата обращения: 16.03.2022). |
| [10] | Федеральные клинические рекомендации Диагностика и лечение ожирения у детей и подростков / Под ред. В.А. Петерковой. – Общественная организация «Российская ассоциация эндокринологов», 2020. – 58 с. |
| [11] | Adiposity is not beneficial to bone mineral density in 0–5 year old Chinese children: The Jiangsu bone health study / Y. Zhao, R. Qin, X. Ma [et al.] // Obesity Research and Clinical Practice. – 2020. – Vol.14. - №1. – P.39-46 |
| [12] | Associations among osteocalcin, leptin and metabolic health in children ages 9– 13 years in the United States / K.V. Giudici, J.M. Kindler, B.R. Martin [et al.] // NutrMetab (Lond). – 2017. – Vol.14. – P.25-34. |
| [13] | Гойибова Н. С., Гарифулина Л. М. Состояние почек у детей с экзогенно-конституциональным ожирением // Журнал гепато-гастроэнтерологических исследований. – 2022. – Т. 3. – №. 2. |
| [14] | Chen X.X. Roles of leptin in bone metabolism and bone diseases / X.X. Chen, T. Yang // J Bone Miner Metab. – 2015. – Vol.33. - №5. – P.474-485. |
| [15] | Холмурадова З. Э., Гарифулина Л. М. Semizligi bor osmirlarda yurak-qon tomir tizimining holati //журнал гепато-гастроэнтерологических исследований. – 2022. – Т. 3. – №. 3. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML