-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(12): 1185-1188
doi:10.5923/j.ajmms.20221212.03
Received: Nov. 16, 2022; Accepted: Nov. 30, 2022; Published: Dec. 9, 2022

Selection Criteria for Hernioallo- and Abdominoplasty Based on the Results of Hernioabdominometry
Akhmadjon Sultanbaevich Babajanov, Saydinjon Botirjon Ugli Makhmudov
Department of Surgical Diseases of the Pediatric Faculty, Samarkand State Medical University, Samarkand, Republic of Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Computer hernioabdomenometry was performed to determine the size of the hernial gate, the volume of the contents of the hernial sac, as well as for preliminary determination of the method of hernioallo- and abdominoplasty. This method was performed in 58 (86.6%) patients with ventral hernias and morbid obesity. The obtained forms of violation of the topography of the anterior abdominal wall made it possible to develop rational preparation of the patient before surgery, as well as to choose the optimal method of hernioplasty individually for each patient.
Keywords: Ventral hernias, Computer hernioabdominometry
Cite this paper: Akhmadjon Sultanbaevich Babajanov, Saydinjon Botirjon Ugli Makhmudov, Selection Criteria for Hernioallo- and Abdominoplasty Based on the Results of Hernioabdominometry, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1185-1188. doi: 10.5923/j.ajmms.20221212.03.
Article Outline
1. Intorduction
- The increase in the number of patients with obesity-related diseases, including ventral hernias, dictates the need to identify the features of surgical treatment of hernias in such patients, develop optimal surgical methods, identify possible complications in the postoperative period, and develop measures to prevent them. The variety of surgical schools and hernioplasty techniques that exist today, sometimes diametrically opposed views of different surgeons on the same problem, dictate the need for systematization and correct assessment of existing knowledge on this problem [2,3,4,6].Thus, it is obvious that so far there is no consensus among surgeons in choosing the method and scope of surgical intervention in overweight and obese patients with ventral and recurrent postoperative hernias [1,5]. In addition to developing a unified concept, the following tasks are relevant: not only to perform hernioplasty in an obese patient without relapse, but also and not to neglect the aesthetic component [7,8]. In this regard, it is necessary to optimize and develop algorithms for surgical treatment for this category of patients.
2. The Purpose of the Research
- To determine the possibilities of computer hernioabdomenometry for determining the method of hernioallo- and abdominoplasty in patients with ventral hernias and morbid obesity.
3. Material and Methods of the Research
- Computer hernioabdominometry (CTHA) was performed in order to determine the size of the hernial gate, the volume of the contents of the hernial sac, to identify additional defects of aponeurosis, to identify concomitant pathology of the abdominal cavity, thickness and uniformity of subcutaneous fat of the anterior abdominal wall, as well as for preliminary determination of the method of hernioallo- and abdominoplasty. This method was performed in 58 (86.6%) patients with ventral hernias and morbid obesity.During the study, the topography of muscle-aponeurotic tissues was described: the location of the defect, the size of the hernial sac, the gate, connective tissue junctions between the wall of the hernial sac and its contents, as well as tissue changes: their structure, density, thickness. When performing CTHA to patients, attention was paid to the patient's position, which plays a significant role. When examining the patient in a horizontal position, the corrected hernial protrusion is corrected and becomes inaccessible for study, therefore, the patient was examined standing with tension of the muscles of the anterior abdominal wall. The thickness and uniformity of the distribution of subcutaneous fat of the anterior abdominal wall were taken into account, while evaluating the possibility of performing abdominoplasty.
4. Results and Discussions
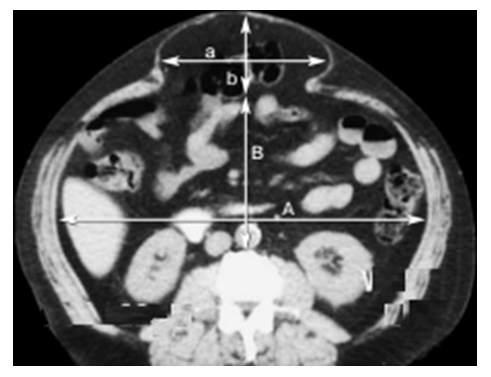
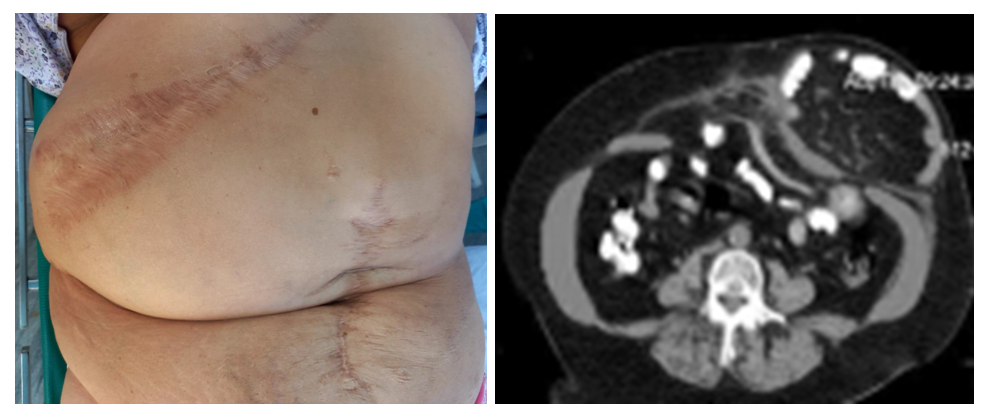
- A defect in the projection of hernial protrusion was reliably visualized in 34 patients. In their length, they were formations from 50 to 250 mm, with a width from 50 to 180 mm. Elements of the omentum, loops of the small intestine, as well as the most mobile parts of the large intestine were identified in the projection of the hernial gate (Fig. 1).
 | Figure 1. View of the anterior abdominal wall and computer hernioabdomenometry of patient P., 56 years old with postoperative ventral hernia (M2W3R0) |
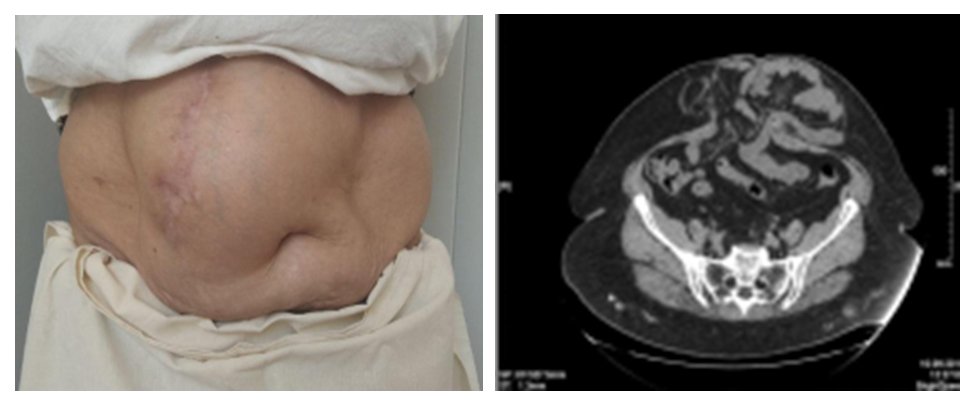
 | Figure 2. View of the anterior abdominal wall and computer hernioabdomenometry of patient K., 52 years old with postoperative ventral hernia (M2W2R0) |
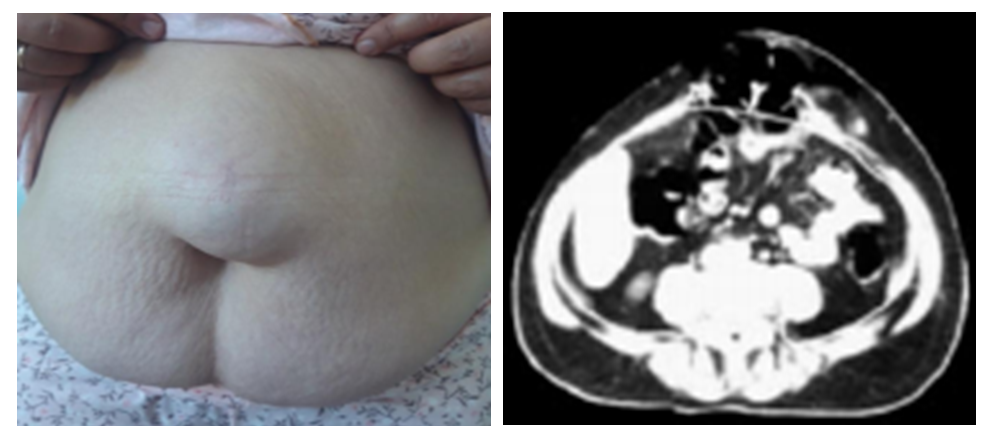
 | Figure 3. View of the anterior abdominal wall and computer hernioabdomenometry of patient S., 62 years old with postoperative ventral hernia (M2W3R0) |
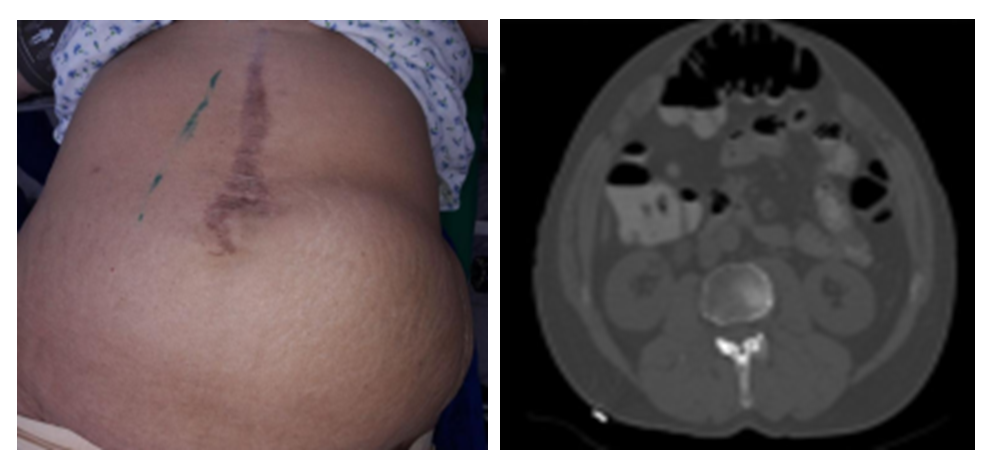
 | Figure 4. View of the anterior abdominal wall and computer hernioabdomenometry of patient G., 54 years old with postoperative ventral hernia (L1W3R2) |
5. Conclusions
- CT hernioabdominometry is informative in diagnosing the condition of the anterior abdominal wall tissues in patients with postoperative ventral hernia. The use of this technique allows us to obtain a more detailed and clear description of the picture that influenced the change in the topography and structure of the elements of the muscular-aponeurotic framework. The resulting forms of topography disorders allowed to develop rational preparation of the patient before surgery, depending on the size of the hernia, as well as to choose the optimal method of hernioplasty individually for each patient.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML