Akhmadjon Sultanbaevich Babajanov1, Jurabek Ibodulloevich Alimov1, Alisher Faridunovich Zayniev2, Jamshed Qodirqulovich Tuxtaev1
1Department of Surgical Diseases of the Pediatric Faculty, Samarkand State Medical University, Samarkand, Republic of Uzbekistan
2Department of Surgical Diseases №1, Samarkand State Medical University, Samarkand, Republic of Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Rationale. Currently, the problem of surgical treatment of patients with nodular goiter remains one of the most urgent. This is primarily due to the development of relapses in the postoperative period. The lack of a unified point of view on the factors determining the risk of postoperative relapses in nodular goiter served as the basis for the study. The purpose. Determination of factors affecting the frequency of recurrence of thyroid nodules. Material. Long-term results of surgical treatment were studied in 368 patients with nodular goiter operated in the surgical department of the multidisciplinary clinic of Samarkand State Medical University. All operated patients are residents of the Samarkand region, which is an iodine-deficient region. The age of the patients at the time of the operation was from 14 to 72 years, the average age was 35.4 ± 6.9 years. Among them there are 291 women (79.1%), 77 men (20.9%). Results. Based on the study of the long-term results of surgical treatment of nodular goiter in residents living in an iodine-deficient region, it was found that the frequency of relapses in this category of patients depends on the duration of follow-up in the postoperative period, the morphological structure of nodular formations and the volume of surgical intervention.
Keywords:
Nodular goiter, Thyroidectomy, Relapse, Iodine deficiency
Cite this paper: Akhmadjon Sultanbaevich Babajanov, Jurabek Ibodulloevich Alimov, Alisher Faridunovich Zayniev, Jamshed Qodirqulovich Tuxtaev, Results of Surgical Treatment of Thyroid Nodules, American Journal of Medicine and Medical Sciences, Vol. 12 No. 12, 2022, pp. 1175-1179. doi: 10.5923/j.ajmms.20221212.01.
1. Introduction
Currently, the problem of surgical treatment of patients with nodular goiter remains one of the most urgent. This is primarily due to the development of relapses in the postoperative period. There are supporters of radical and organ-preserving operations. When performing organ-preserving operations, researchers point to the need to preserve part of the gland tissue to prevent postoperative hypothyroidism, which will avoid taking thyroid medications [1]. Proponents of radical operations consider organ-preserving operations to be unjustified, since this increases the risk of relapse of the disease to 25-40% [2,3]. A number of authors note the occurrence of relapse of nodular nontoxic goiter in 5.8% of cases [4]. In 68% of cases, relapse occurred after primary surgery, where the volume of surgery did not exceed resection of one or both lobes of the thyroid gland; in 16% of cases, relapse was detected after performing radical operations, but was subsequently associated with a different morphological form goiter, coarser than originally [5]. Some authors argue that the main role in the pathogenesis of relapse development is played not by the volume of the operation performed, but by the etiology and morphological structure of the nodular formation [6]. The lack of a unified point of view on the factors determining the risk of postoperative relapses in nodular goiter served as the basis for the study.
2. The Purpose of the Research
Determination of factors affecting the frequency of recurrence of thyroid nodules.
3. Materials and Methods of the Research
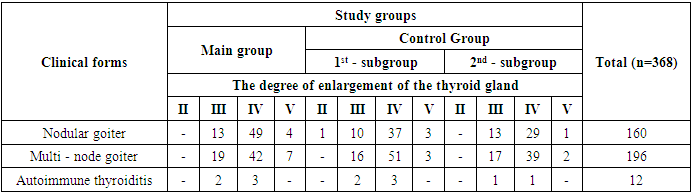
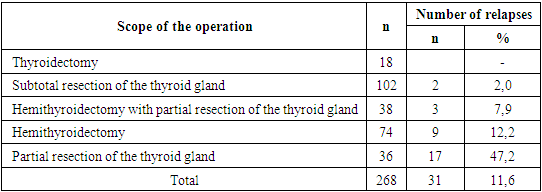
Long-term results of surgical treatment were studied in 368 patients with nodular goiter operated in the surgical department of the multidisciplinary clinic of the Samarkand State Medical University. All operated patients are residents of the Samarkand region, which is an iodine-deficient region. The age of the patients at the time of the operation was from 14 to 72 years, the average age was 35.4 ± 6.9 years. Among them there are 291 women (79.1%), 77 men (20.9%). The euthyroid state was noted in 329 patients (89.4%), functional thyroid autonomy was detected in 39 (10.6%). During the operation and after it, all patients underwent histological examination.In most cases, multi–nodular colloidal goiter was verified in 196 patients (52.3%) and nodular colloidal goiter in 160 patients (43.5%), autoimmune thyroiditis was observed in 12 patients (3.2%) (Table 1).Table 1. Clinical form and degree of enlargement of the thyroid gland according to O.V. Nikolaev
 |
| |
|
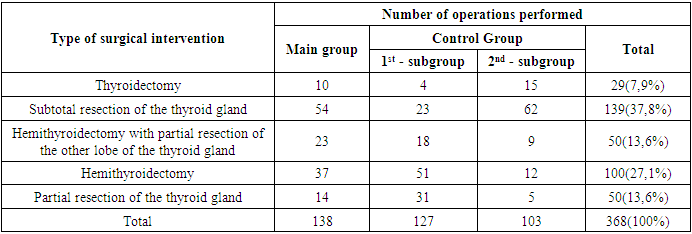
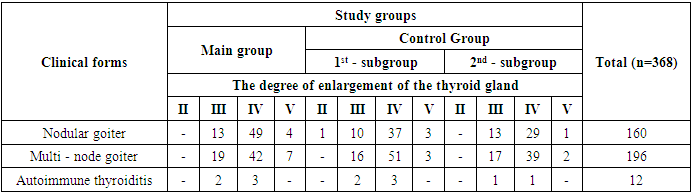
The volume of surgery most often corresponded to subtotal resection of the thyroid gland - 37.8%. Hemithyroidectomy was performed in 27.1% of patients, hemithyroidectomy with partial resection of another thyroid lobe in 13.6% of patients and partial resection of the thyroid gland in 13.6% of patients. Thyroidectomy was performed in 7.9% of cases (Table 2).Table 2. Distribution of patients with nodular goiter depending on the volume of surgery
 |
| |
|
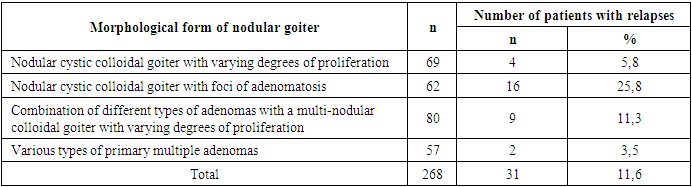
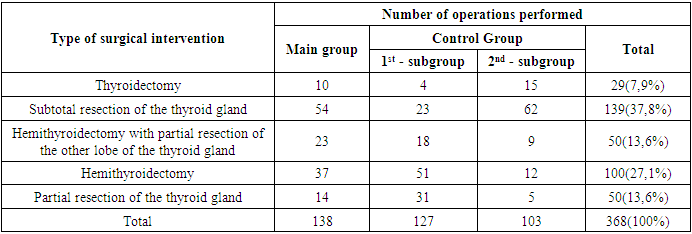
The long-term results were analyzed in 268 (72.8%) of 368 operated patients for nodular goiter. Special attention was paid to the duration of the disease, medical treatment with thyroid hormone preparations after surgery. Such indicators as the volume of the operation, clinical and morphological features of the disease, immediate and long–term results of surgical treatment were studied.Long-term results of surgical treatment of patients with nodular goiter were studied in terms from 1 to 12 years. At the same time, the fate of 202 (75.4%) patients was traced for more than 2 years, sufficient for the final formation of a clinically significant relapse of the disease or hypothyroidism. 66 patients (24.6%) were observed for less than 2 years. Relapses of nodular goiter were diagnosed in 31 patients (11.6%). In the first 2 years after the operation, no relapses of the disease were detected. After 2-5 years, out of 202 patients, relapse was established in 9 patients (4.4%). At follow–up, after 5-7 years, out of 142 patients, relapse was detected in 13 (9.1%), after 7-12 years out of 60 - in 9 (15.0%).Thus, there is a clear pattern that with an increase in the period of observation of patients in the iodine-deficient region, the number of relapses increases. The highest recurrence rate was established after 10 years, the lowest after 5 years, and there were no relapses in the first 2 years after surgery.In order to identify the influence of morphological form on the frequency of recurrence of nodular goiter, an analysis of histological studies of primary interventions was carried out (Table 3).Table 3. Distribution of patients with relapses depending on the morphological form of nodular goiter
 |
| |
|
4. Results
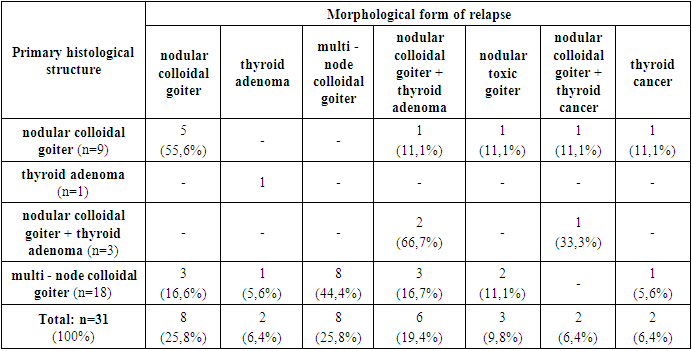
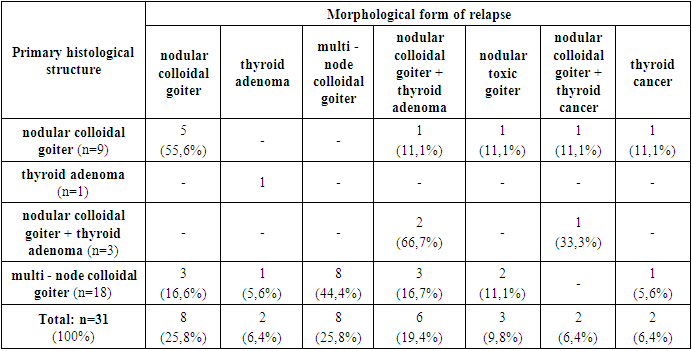
69 cases of nodular cystic colloidal goiter with varying degrees of proliferation, relapses were detected in 4 patients (5.8%). When combining different types of adenomas with a multi-nodular colloidal goiter with varying degrees of proliferation, relapse was found in 9 out of 80 patients (11.3%). The greatest number of relapses was found in nodular cystic colloidal goiter with foci of adenomatosis in 16 of 62 patients (25.8%). The lowest recurrence rate in various types of primary multiple adenomas - 2 patients out of 57 (3.5%). Of the 31 patients with relapse of the disease, the majority of 26 (83.9%) were operated again. The remaining 5 patients (16.1%) had no indications for repeated surgery. Ultrasound examination of the thyroid gland revealed nodes up to 1.5 cm in diameter, and cytological examination after a targeted fine needle aspiration biopsy verified nodular colloidal goiter. All 5 patients had previously been operated on for nodular colloidal goiter.When studying the morphogenesis of recurrent goiter, a comparative analysis of the morphological form of recurrent goiter with the histological structure of nodular formations after primary operations was carried out (Table 4).Table 4. Distribution of patients depending on the primary histological structure and morphological form of relapse
 |
| |
|
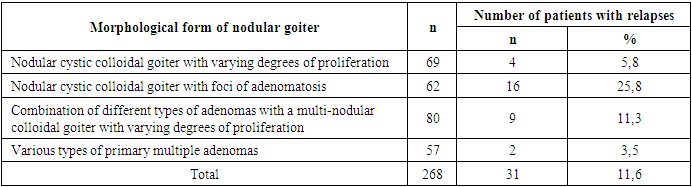
Of the 9 patients operated on for nodular colloidal goiter, in most cases 5 (55.6%) had a morphological structure of recurrence corresponding to nodular colloidal goiter, in 1 case (11.1%) nodular colloidal goiter was combined with thyroid adenoma, in 1 (11.1%) thyrotoxic adenoma was detected and 1 patient (11.1%) were papillary thyroid cancer and a combination of nodular colloidal goiter and papillary thyroid cancer. The size of malignant neoplasms did not exceed 1 cm in diameter. Thyroid cancer in both cases was localized in the thyroid stump after subtotal resection. In 3 patients with a combination of nodular colloidal goiter and thyroid adenoma, the histological structure in 2 cases coincided with the results of the primary histological examination. A combination of nodular colloidal goiter and papillary thyroid cancer was detected in 1 patient. The size of the tumor node was 0.5 cm in diameter and was diagnosed after subtotal resection. Of 18 patients with multi-nodular colloidal goiter, 8 patients (44.4%) had the same morphological structure of relapse as during the initial operation, and 3 patients (16.6%) had nodular colloidal goiter, 1 patient (5.6%) had thyroid adenoma, 3 (16.6%) had nodular colloidal goiter combined with thyroid adenoma, thyrotoxic adenoma was detected in 2 cases (11.1%). 1 patient with a multi-node colloidal goiter was diagnosed with thyroid cancer during repeated surgery.The results obtained indicate that in 25.8% of cases the morphological structure of recurrent goiter corresponds to nodular colloidal goiter and in 25.8% of cases to multi-nodular colloidal goiter, in 19.4% of cases nodular colloidal goiter was combined with thyroid adenoma. Nodular toxic goiter was detected in 9.8% of cases, 6.4% of patients had thyroid adenoma, 6.4% of patients with relapse were diagnosed with thyroid cancer and 6.4% had a combination of thyroid cancer and nodular colloidal goiter.Thus, the morphological structure of relapse coincided with the results of the primary histological examination in 16 cases (51.6%). In the remaining 15 patients (48.4%), a different morphological structure of nodular formations was revealed. This fact indicates that the left thyroid tissue potentiates the appearance of both a relapse of the disease and the development of a new disease of the thyroid residue. At the same time, 12.8% of patients are likely to develop thyroid cancer after organ-preserving operations.The choice of the optimal volume of surgery for nodular goiter is still the most controversial and unresolved issue. The results of the study of the effect of the volume of surgical interventions in patients with nodular goiter on the frequency of recurrence are presented in Table 5.Table 5. Distribution of patients with recurrent nodular goiter depending on the volume of surgery
 |
| |
|
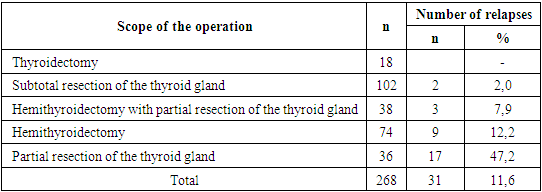
During the entire observation period, there was no recurrence of the disease in patients operated on in the volume of thyroidectomy. Relapse after subtotal resection performed in 102 patients developed in 2 patients (2.0%). Of 38 patients after hemithyroidectomy with partial resection of the other lobe in 3 cases (7.9%). Of 74 patients after hemithyroidectomy, relapses were found in 9 cases (12.2%), of 36 patients after partial resection – in 17 cases (47.2%). Thus, performing thyroidectomy provided the patient with a relapse-free course of the disease. In a minimal number of cases – 2.0% of patients had a relapse after subtotal resection. The highest recurrence rate was found after partial resection of the thyroid gland in 47.2% of cases.Recurrences of subtotal resection after 5 years were not detected in 27 patients, after 7 years relapses developed in 1 patient out of 40 patients (2.5%), after 10 years out of 31 – in 1 (3.2%). In these two patients, the volume of the left tissue according to the postoperative ultrasound of the thyroid gland was about 3 ml. After hemithyroidectomy with partial resection of the thyroid gland, relapses developed after 7 years out of 22 patients in 1 patient (4.5%) and after 10 years out of 16 patients in 2 patients (12.5%). After hemithyroidectomy, relapses developed after 5 years out of 27 patients in 1 patient (3.7%), after 7 years out of 21 patients in 3 patients (14.3%) and after 10 years out of 26 patients in 5 patients (19.2%). After performing partial resection of the thyroid gland, relapses developed after 5 years out of 12 patients in 3 patients (25.0%), after 7 years out of 8 patients in 3 patients (37.5%) and after 10 years out of 16 patients in 11 patients (68.7%). The maximum number of relapses was established after 10 years, and the minimum frequency of relapses was observed after 2 years. So, with an increase in the follow-up period, the total number of relapses increases (Fig. 1), and with an increase in the volume of surgery, the frequency of relapses decreases in all follow-up periods. With radical operations of thyroidectomy and subtotal resection, relapse develops rarely and at a late date. With organ-preserving interventions: hemithyroidectomy and partial resection, the recurrence rate is significantly higher compared to radical operations, and the number of relapses increases with increasing follow-up periods.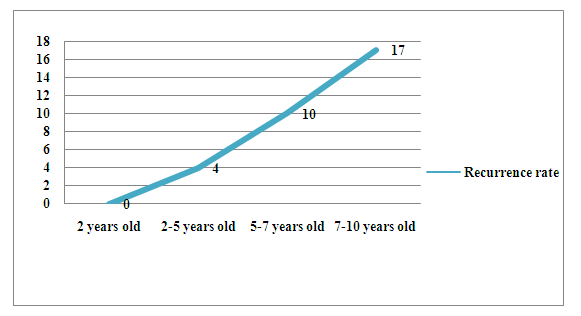 | Figure 1. Dynamics of relapses of nodular goiter depending on the period of observation |
Thus, the highest recurrence rate was established after 10 years. The lowest recurrence rate was found after 2 years. The absence of relapses up to 2 years of follow-up with all volumes of surgery indicates that relapses, obviously, have not yet developed.
5. Conclusions
1. Based on the study of the long-term results of surgical treatment of nodular goiter in residents living in an iodine-deficient region, it was found that the frequency of relapses in this category of patients depends on the duration of follow-up in the postoperative period, the morphological structure of nodular formations and the volume of surgical intervention.2. Nodular colloidal goiter in patients living in the iodine-deficient region is a disease of the entire thyroid gland, since the tissue located near the nodular formations is completely affected by the so-called goiter changes. That is why the maximum recurrence rate was established in patients with multi-node colloidal goiter operated 10 years ago in the volume of hemithiroidectomy or partial resection.3. Organ-preserving resections should be recognized as non-radical operations that lead to the development of relapse. Therefore, performing thyroidectomy and extreme subtotal resection in patients with nodular colloidal goiter living in an iodine-deficient region is an adequate and radical intervention.
References
| [1] | Babajanov Akhmadjon Sulatanbaevich, Abdurakhmanov Diyor Shukurullaevich, Yusupalieva Dilnora Bakhodir Qizi, & Tilavova Yulduz Muhammadshukur Qizi (2019). Analysis of the results of surgical treatment of patients with thyroid nodules. Вопросы науки и образования, (4 (49)), 186-192. |
| [2] | Babajanov Akhmadjon Sultanbaevich, Akhmedov Adham Ibadullaevich, Toirov Abdukhamid Suvonkulovich, Akhmedov Gayrat Keldibekovich, & Hudoynazarov Utkir Rabbimovich (2018). The states of the thyroid residue in the postoperative period in patients with multinodal nontoxic goiter. European science review, (9-10-2), 33-35. |
| [3] | Babajanov Ahmadjan Sultanbayevich, Toirov Abdukhamid Suvonkulovich, & Akhmedov Adkham Ibodullayevich (2020). Tactics of treatment of thyroid nodules based on the grading scale. Academy, (4 (55)), 100-104. |
| [4] | Pescatori, L. C., Torcia, P., Nicosia, L., Mauri, G., Rossi, U. G., & Cariati, M. (2018). Which needle in the treatment of thyroid nodules?. Gland surgery, 7(2), 111. |
| [5] | Cho, S. J., Baek, J. H., Chung, S. R., Choi, Y. J., & Lee, J. H. (2020). Long-term results of thermal ablation of benign thyroid nodules: a systematic review and meta-analysis. Endocrinology and Metabolism, 35(2), 339-350. |
| [6] | Papini, E., Monpeyssen, H., Frasoldati, A., & Hegedüs, L. (2020). 2020 European thyroid association clinical practice guideline for the use of image-guided ablation in benign thyroid nodules. European thyroid journal, 9(4), 172-185. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML