-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(11): 1132-1135
doi:10.5923/j.ajmms.20221211.08
Received: Oct. 26, 2022; Accepted: Nov. 19, 2022; Published: Nov. 24, 2022

Immunohistochemical Changes of Bcl-2 Protein in Bladder Leukoplakia
Raykhana Rafaelevna Sakhatalieva
Doctor of Philosophy (PhD), Assistant of the Department of Surgery and Urology, Andijan State Medical Institute, Uzbekistan
Correspondence to: Raykhana Rafaelevna Sakhatalieva, Doctor of Philosophy (PhD), Assistant of the Department of Surgery and Urology, Andijan State Medical Institute, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In this work, indicators of the expression level of anti-apoptotic protein Bcl-2 in different stages of bladder leukoplakia were determined. The results showed that this protein was expressed only in the basal layer in the bladder lining epithelium in the control group. During the initial stage I of the development of leukoplakia, during the metaplastic process in the changing epithelium, the expression of Bcl-2 protein was observed to increase to a high level in the cells of the basal layer of the epithelium with acanthosis. In the II-stage of leukoplakia, all layer cells of the epithelium undergo metaplasia and are located vertically, Bcl-2 protein is relatively more expressed in the cells of the basal and intermediate layers, and in the III-stage of the disease, the expression of this protein increases even more.
Keywords: Bladder, Cystitis, Leukoplakia, Immunohistochemistry, Bcl-2 protein
Cite this paper: Raykhana Rafaelevna Sakhatalieva, Immunohistochemical Changes of Bcl-2 Protein in Bladder Leukoplakia, American Journal of Medicine and Medical Sciences, Vol. 12 No. 11, 2022, pp. 1132-1135. doi: 10.5923/j.ajmms.20221211.08.
1. Introduction
- The 6th protein of Bcl-2 domain, which is located on human chromosome 18 and has anti-apoptotic properties out of 16 proteins, is a homologous protein that slows down the process of apoptosis. This protein with a molecular weight of 22 kDa is located in the cell and nuclear membrane, sarcoplasm and mitochondrial membrane [2,4,7]. Hyperexpression of this protein inhibits the release of calcium ions and inhibits antioxidant activity by slowing down lipoperoxidation and NO-synthetase activity. The main function of Bcl-2 is to stop cytochrome S, AIF, ATF, which are anti-apoptotic molecules from mitochondria, from exiting through pores. Bcl-2 binds to the mitochondrial membrane and closes the pores, stops proapoptotic signals and prevents apoptosis [1,3,8].Leukoplakia of the urinary bladder can develop under the influence of various pathological factors, as a result of which the cells of the covering epithelium of the urinary bladder die due to the process of programmed apoptosis. But in most cases, due to chronic diseases, the apoptosis process of cells can slow down and stop. Therefore, in our study, we aimed to investigate the antiapoptosis protein Bcl-2 in the lining epithelial cells in bladder leukoplakia. Increased Bcl-2 activity is observed in a number of bladder diseases, including leukoplakia. Due to the development of inflammatory and disregenerative processes in the submucous connective tissue layer of the bladder leukoplakia, the differentiation of cells in the covering epithelium is disturbed and often lags behind, the proliferative activity of the cells of the basal layer increases, and the anti-apoptotic protein Bcl-2 can be activated in them. [2,5,6]. The expression level was evaluated as the percentage of stained cells (x400) from the field of view. The distribution and intensity of the immunohistochemical reaction in the sample were taken into account, i.e. (absence of expression or staining in a small amount of 10% of cells - 0 points, 10 to -25% - 1 point, 26 to -50% - 2 points, 51 to -75% - 3 points and More than 75% is -4 points.
2. Маtеrials and Methods
- The 6th protein of Bcl-2 domain, which is located on human chromosome 18 and has anti-apoptotic properties out of 16 proteins, is a homologous protein that slows down the process of apoptosis. This protein with a molecular weight of 22 kDa is located in the cell and nuclear membrane, sarcoplasm and mitochondrial membrane [2,4,7]. Hyperexpression of this protein inhibits the release of calcium ions and inhibits antioxidant activity by slowing down lipoperoxidation and NO-synthetase activity. The main function of Bcl-2 is to stop cytochrome S, AIF, ATF, which are anti-apoptotic molecules from mitochondria, from exiting through pores. Bcl-2 binds to the mitochondrial membrane and closes the pores, stops proapoptotic signals and prevents apoptosis [1,3,8].Leukoplakia of the urinary bladder can develop under the influence of various pathological factors, as a result of which the cells of the covering epithelium of the urinary bladder die due to the process of programmed apoptosis. But in most cases, due to chronic diseases, the apoptosis process of cells can slow down and stop. Therefore, in our study, we aimed to investigate the antiapoptosis protein Bcl-2 in the lining epithelial cells in bladder leukoplakia. Increased Bcl-2 activity is observed in a number of bladder diseases, including leukoplakia. Due to the development of inflammatory and disregenerative processes in the submucous connective tissue layer of the bladder leukoplakia, the differentiation of cells in the covering epithelium is disturbed and often lags behind, the proliferative activity of the cells of the basal layer increases, and the anti-apoptotic protein Bcl-2 can be activated in them. [2,5,6]. The expression level was evaluated as the percentage of stained cells (x400) from the field of view. The distribution and intensity of the immunohistochemical reaction in the sample were taken into account, i.e. (absence of expression or staining in a small amount of 10% of cells - 0 points, 10 to -25% - 1 point, 26 to -50% - 2 points, 51 to -75% - 3 points and More than 75% is -4 points.
3. Results and Discussion
- In order to determine the pathomorphological and immunohistochemical changes occurring in the covering epithelium of the bladder, biopsy material obtained from people without any pathology in the bladder was studied as a control group. Then, the pathomorphological and immunohistochemical changes in the mucous membrane and lining epithelium of the urinary bladder were studied in comparison with each other according to the clinical and morphological forms of leukoplakia and development periods.In the control group, it was found that the lining epithelium of the bladder mucous membrane in the patients consists of the usual multi-layered variable epithelium, and its epithelial cells located in the basal layer are relatively large, hyperchromic, arranged in the basement membrane, and most of their nuclei are oval and elongated. In the surface layers of the multi-layered epithelium, it was observed that the cells were relatively sparse, their nuclei were reduced in size, their staining was lighter, and their location was flattened. The results of the immunohistochemical examination for the detection of the anti-apoptosis protein of the epithelial cells showed that in the control group, this protein was expressed at a very low level in the cytoplasm of some cells located in the basement membrane and in the cambial level, and it was not expressed in the cells of the other intermediate and surface layers (Fig. 1).
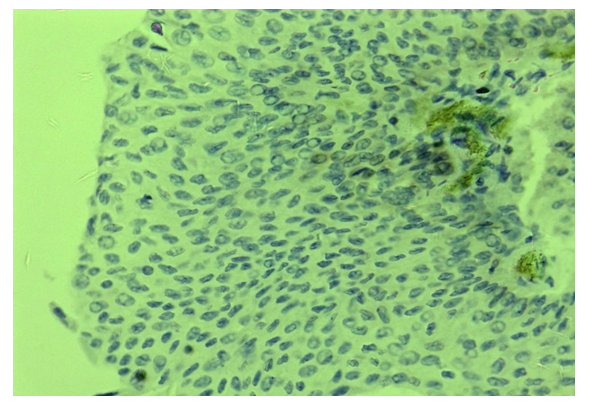 | Figure 1. Bladder, norm, Bcl-2 protein is expressed at a low level in some cells of the basal layer. Stain: immunohistochemical method. 10x40 |
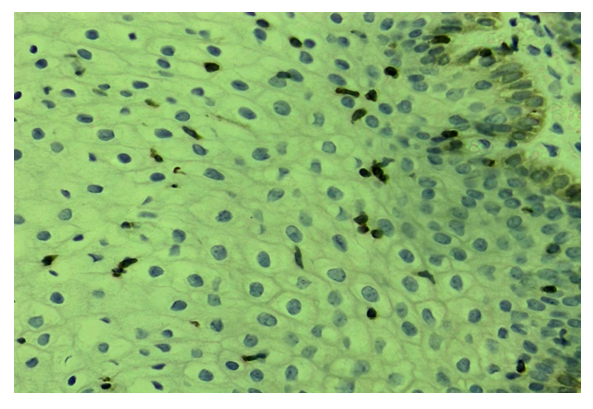 | Figure 2. Bladder, leukoplakia grade I, Bcl-2 protein is expressed in some cells of the basal layer and intermediate layer. Stain: immunohistochemical method. 10x40 |
 | Figure 3. Bladder, leukoplakia grade I, Bcl-2 protein is expressed close to the nucleus of interstitial epithelial cells. Stain: immunohistochemical method. 10x40 |
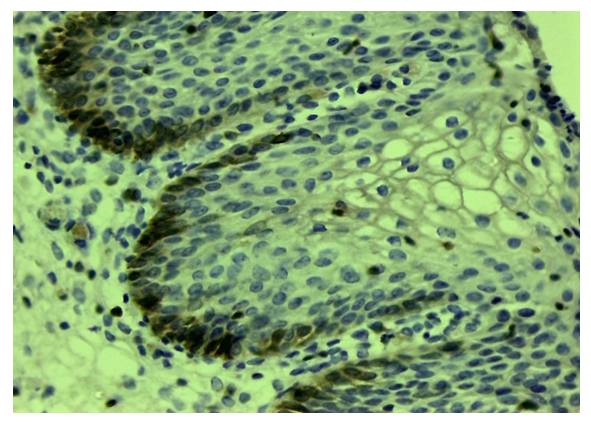 | Figure 4. Urinary bladder, leukoplakia grade II, Bcl-2 is expressed in the basal layer 2-3 rows. Stain: immunohistochemical method. 10x40 |
 | Figure 5. Bladder, leukoplakia grade III, Bcl-2 was expressed in most cells of the basal and intermediate layers. Stain: immunohistochemical method. 10x40 |
4. Conclusions
- Immunohistochemical study of bladder leukoplakia, that is, determining which layers of the covering multi-layered variable epithelium express anti-apoptotic Bcl-2 protein, is an important factor in the diagnosis of this disease.In the control group without any disease in the bladder, Bcl-2 protein is expressed at a low level only in the basal layer, indicating that the apoptosis activity is preserved in them.During the first stage I of leukoplakia development, during the emergence of a metaplastic process in the changing epithelium, the expression of Bcl-2 protein in cells of the basal layer of the epithelium with developed acanthosis indicates the activation of the anti-apoptotic gene.It was found that in the II stage of leukoplakia, all layer cells of the epithelium undergo metaplasia and are located vertically, Bcl-2 protein is expressed at a relatively higher level in the cells of their basal and intermediate layers.In the III-period of leukoplakia, proliferative activity and metaplasia are developed in the cells of all layers of the epithelium, there is inflammation in the private plate, Bcl-2 protein is expressed at a high level in all epithelial cells.Bcl-2 protein expression increased from immunohistochemical markers in different stages of bladder leukoplakia, i.e. increased from 19.3% to 43.7% (3.5 points) as the level of the disease worsened. It is recommended to use these numbers as an indicator for predicting the consequences of the disease.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML