-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(11): 1128-1131
doi:10.5923/j.ajmms.20221211.07
Received: Oct. 26, 2022; Accepted: Nov. 9, 2022; Published: Nov. 24, 2022

Сardiovacular Comorbidity in Patients with Chronic Obstructive Pulmonary Disease
Toshov S. S.1, Kamilova U. K.2
1Bukhara State Medical Institute, Bukhara, Uzbekistan
2Republican Specialized Scientific-Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan
Correspondence to: Kamilova U. K., Republican Specialized Scientific-Practical Medical Center of Therapy and Medical Rehabilitation, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

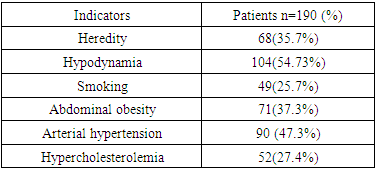
The aim of our study of the is to evaluate cardiovascular comorbidity in patients with сhronic obstructive pulmonary disease (COPD). 190 patients from 35 to 60 years old who were examined. The average age of the patients was 57.81±1.23 years. In determining the presence of cardiovascular risk factors in patients. When analyzing the presence of risk factors in one patient, 77.9% of patients have a risk factor, of which 13.7% of patients with 1st risk factor, 15.8% of patients with 2nd risk factors, 15.8% of patients with 3rd or more risk factors It was 48.4%. Risk factors were not observed in 22.1% of patients. Identifying groups of patients with a high cardiovascular risk in patients with COPD provides an opportunity for early targeted prevention and interventions. Early detection of comorbidity of cardiovascular diseases in patients with COPD makes it possible to predict the clinical course of the disease and choose the correct treatment tactics, and as a result, it is important to reduce morbidity, disability and mortality rates, and improve the patient's quality of life and prognosis.
Keywords: Chronic obstructive pulmonary disease, Cardiovascular diseases, Cardiovascular risk factors
Cite this paper: Toshov S. S., Kamilova U. K., Сardiovacular Comorbidity in Patients with Chronic Obstructive Pulmonary Disease, American Journal of Medicine and Medical Sciences, Vol. 12 No. 11, 2022, pp. 1128-1131. doi: 10.5923/j.ajmms.20221211.07.
1. Introduction
- Chronic obstructive pulmonary disease (COPD) is a common disease characterized by extrapulmonary manifestations and comorbidities [1]. Among them, cardiovascular disease is one of the most common comorbidities in patients with COPD and has a significant impact on disease severity and prognosis [2,3]. Accumulated evidence shows that early targeted prevention and interventions in high cardiovascular risk groups are of great importance in disease prevention [4]. Even in mild-to-moderate COPD patients, detection of subclinical cardiovascular changes in individuals at risk for cardiovascular disease can help increase patient awareness of the disease [5]. The association with a two- or three-fold increase in the risk of ischemic heart disease and other cardiovascular diseases (CVD) is often associated with increased markers of systemic inflammation [6]. Although cardiovascular risk factors (e.g., smoking, hypertension) are more common in patients with COPD, the presence of these cardiovascular risk factors may fully explain the accelerated atherosclerotic process found in COPD through the development of endothelial dysfunction observed in the disease [7]. In recent years, the term comorbidity has entered medicine. This situation indicates the presence of comorbidities that occur in patients with the main disease. Comorbidities are characterized by their influence on the clinical course of the disease in patients, as well as the determination of treatment tactics in patients and the assessment of their impact on the prognosis of the disease. In the literature, there is a number of data on the association of SCI with diseases of the cardiovascular system [8]. However, in the presented data, the influence of these comorbidities on the clinical course of COPD is more illuminated. There is little information on the occurrence of cardiovascular diseases and the importance of cardiovascular factors.The aim of our study of the is to evaluate cardiovascular comorbidity in patients with COPD.
2. Materials and Methods
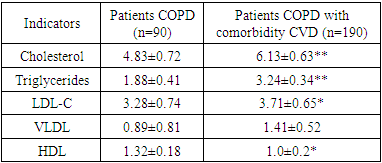
- 190 patients with COPD aged 35 to 60 years, who were in the pulmonology department of the Bukhara Multidisciplinary Medical Center, were examined. The average age of the patients was 57.81±1.23 years. There were 106 (55.8%) women and 84 (44.2%) men with COPD. In determining the presence of cardiovascular risk factors in patients, the frequency of heredity, smoking, hypercholesterolemia, abdominal obesity (AO), arterial hypertension (AH), ischemic heart disease (IHD) was also evaluated. Statistical processing of the results obtained was carried out on a personal computer using the Microsoft Office Excel – 2020 software package, including the use of built-in statistical processing functions, as well as using the STATISTICA-13.3 software package. The methods of variational parametric and nonparametric statistics were used with the calculation of the arithmetic mean of the studied indicator (M), standard deviation (SD), standard error of the mean (m), relative values (frequency, %), the statistical significance of the measurements obtained when comparing the average values was determined by the criterion Student (t) with the calculation of the probability of error (p). Significance level p<0.05 was taken as statistically significant changes.
3. Results
- Analyzing the results of the study patients COPD, according to the severity of the disease, 13 (6.8%) patients had I, 57 (30%) patients - II, 81 (42.6%) - III, and 39 (20.5%) patients - IV (Fig. 1).
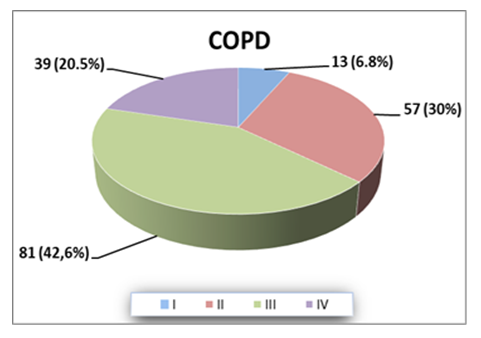 | Figure 1. Severity of patients COPD comorbide with CVD |
|
|
4. Discussion
- CVD are arguably the most important comorbidities in COPD. CVD are common in people with COPD, and their presence is associated with increased risk for hospitalization, longer length of stay and all-cause and CVD-related mortality [9]. The economic burden associated with CVD in this population is considerable and the cumulative cost of treating comorbidities may even exceed that of treating COPD itself. Our understanding of the biological mechanisms that link COPD and various forms of CVD has improved significantly over the past decade [10]. But despite broad acceptance of the prognostic significance of CVDs in COPD, there remains widespread under-recognition and undertreatment of comorbid CVD in this population. The reasons for this are unclear; however institutional barriers and a lack of evidence-based guidelines for the management of CVD in people with COPD may be contributory factors. In this review, we summarize current knowledge relating to the prevalence and incidence of CVD in people with COPD and the mechanisms that underlie their coexistence [11]. Pathophysiological links between COPD and CVD include lung hyperinflation, systemic inflammation and COPD exacerbations. Arterial hypertension is one of the most common risk factors. In our study, comorbidity with hypertension was 90 (47.3%). The PAHIS study showed that the prevalence of hypertension in Serbia is 42.7%. Arterial hypertension is more often diagnosed in women (53.3%) than in men (46.7%). One thousand four hundred and twelve respondents had previously been diagnosed and treated for arterial hypertension [12]. Clearer recommendations are necessary regarding the identification and management of comorbid CVD in patients with COPD in order to facilitate early intervention and appropriate treatment [13]. It is now well established that cardiovascular-related comorbidities contribute to morbidity and mortality in COPD, with approximately 50% of deaths in COPD patients attributed to a cardiovascular event (e.g. myocardial infarction). Cardiovascular disease (CVD) and COPD share various risk factors including hypertension, sedentarism, smoking and poor diet but the underlying mechanisms have not been fully established. However, there is emerging and compelling experimental and clinical evidence to show that increased oxidative stress causes pulmonary inflammation and that the spill over of pro-inflammatory mediators from the lungs into the systemic circulation drives a persistent systemic inflammatory response that alters blood vessel structure, through vascular remodelling and arterial stiffness resulting in atherosclerosis [14].The course of COPD is diverse; it depends on pathologies in the respiratory system and on other organ dysfunctions. The severity and natural course of COPD, as well as quality of the patient's life, are influenced by them. CVDs are frequently the reason for hospitalisation and may lead to death. They are also an important prognostic factor. Comorbidities may prolong exacerbation of COPD. On the other hand, COPD is an independent risk factor of CVD. Careful and proper treatment of all diseases is essential. An interdisciplinary team with good cooperation should prepare a plan of COPD treatment with simultaneous therapy of comorbidities [15].
5. Conclusions
- Identifying groups of patients with a high cardiovascular risk in patients with COPD provides an opportunity for early targeted prevention and interventions. Early detection of comorbidity of cardiovascular diseases in patients with COPD makes it possible to predict the clinical course of the disease and choose the correct treatment tactics, and as a result, it is important to reduce morbidity, disability and mortality rates, and improve the patient's quality of life and prognosis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML