-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(10): 1063-1067
doi:10.5923/j.ajmms.20221210.12
Received: Sep. 8, 2022; Accepted: Oct. 8, 2022; Published: Oct. 21, 2022

A New View on the Problem of Bleeding Acute Gastric Ulcers
Khakimov Murod Shavkatovich, Ashurov Sheroz Ermatovich, Dekhkonov Jamol Kurbonalievich, Karimov Makhmud Rustamovich, Kushiev Jakhongir Khabibjon Ugli
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This article is about gastric and duodenal ulcer disease and its complication of bleeding. Patients applied to the emergency surgery department. In endoscopy, it is divided according to the Forrest classification, and during bleeding, it is shown how to help patients and stop bleeding. The patient's blood tests, hemodynamic indicators, age, gender, and most importantly, the localization of the injury are taken into account. Endoscopic procedures, including endoscopic clipping, endoscopic injection, caulking, and other procedures are performed on patients who are bleeding and at high risk of bleeding. Here we used a new method of stopping blood, such as retrograde hemostasis. This method is used if there is bleeding in the upper part of the stomach, cardiac areas, and makes it possible to perform difficult endoscopic procedures without difficulty using this method.
Keywords: Endoscopic haemostasis, Retrograde endoscopic haemostasis, Injection, Haemoclipping, Argon plasma coagulation, Profuse gastroduodenal peptic ulcer bleeding
Cite this paper: Khakimov Murod Shavkatovich, Ashurov Sheroz Ermatovich, Dekhkonov Jamol Kurbonalievich, Karimov Makhmud Rustamovich, Kushiev Jakhongir Khabibjon Ugli, A New View on the Problem of Bleeding Acute Gastric Ulcers, American Journal of Medicine and Medical Sciences, Vol. 12 No. 10, 2022, pp. 1063-1067. doi: 10.5923/j.ajmms.20221210.12.
Article Outline
1. Relevance
- Bleeding from acute stomach ulcers is a common medical emergency throughout the world. Endoscopic diagnosis and hemostasis are cornerstones in disease management and mortality reduction. The number of urgent open surgical interventions for bleeding acute ulcers continues to decline; in the UK, the rate of surgery has fallen from 8% to 2% between 1993 and 2006 [1]. During the same period in the United States, the use of endoscopic treatment for acute ulcers increased by 58.9%, and the incidence of emergency ulcer surgery decreased by 21.9% [2].Despite these advances, death from this disease remains at about 10% [3]. The disease occurs more often in elderly patients with frequent comorbidities who take antiplatelet agents, non-steroidal anti-inflammatory drugs and anticoagulants [4]. The management of such patients, especially those at high risk of cardiothrombotics who are taking anticoagulants, is a challenge for clinicians.At present, in the diagnosis of acute gastric ulcers, the impact of the anatomical and pathomorphological characteristics of the mucous membrane around the ulcer on the prognosis of the risk of rebleeding and the outcome of the disease is not taken into consideration.The aim of this study was to increase the efficiency of diagnosing acute gastric ulcers and predict the risk of rebleeding by studying the endoscopic, anatomical features and pathomorphological characteristics of tissues in the area of a bleeding gastric ulcer.
2. Material and Methods
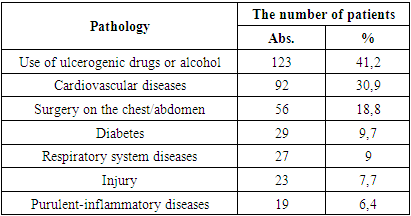
- The material of this study was 298 patients with bleeding from acute gastric ulcers (stress, drug), who were treated in the emergency surgery department of the multidisciplinary clinic of the Tashkent Medical Academy from 2012 to 2022. There were 192 men (64.4%), women - 106 (35.6%). The age of the patients ranged from 18 to 76, averaging 49.6±10.3 years.The majority of patients (227 - 76.17%) were taken to the emergency department by an ambulance team at various times from the onset of the disease: in the first 6 hours - 35 (11.7%) patients, from 7 to 24 hours - 105 (35.2%) patients. In other patients, the period from the onset of the disease to admission to the hospital was more than a day. Directly in the hospital, bleeding occurred in 71 (23.8%) patients (in intensive care units, cardiology, nephrology, elective surgery, neurology, traumatology and orthopedics, neurosurgery, gynecology, rheumatology).Most often, acute bleeding gastric ulcers occurred when taking ulcerogenic drugs (NSAIDs, hormone therapy) or alcohol - 123 (41.2%). Also, acute ulcers were quite common in patients with diseases of the cardiovascular system - 92 (30.9%) and acute ulcers complicated by bleeding after thoracic / abdominal surgical interventions (stress ulcers) - 56 (18.8%) (Table 1).
|
|
3. Results
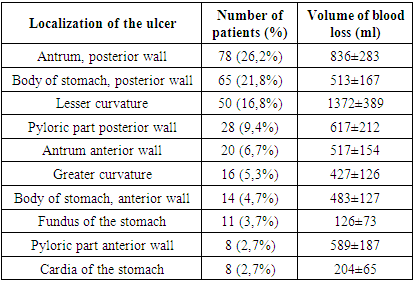
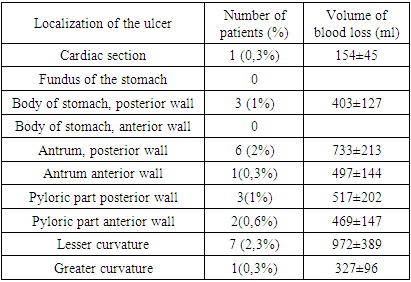
- Upon admission of patients with acute gastric ulcers, endoscopic hemostasis was performed. The choice of hemostasis method depended on the intensity of bleeding.In case of recurrence of bleeding after endoscopic hemostasis, an attempt was made to repeat endoscopic hemostasis. If it was impossible to achieve endoscopic hemostasis or repeated recurrence, the patients underwent surgical treatment - gastrotomy with stitching of a bleeding acute stomach ulcer. Mostly, endoscopic hemostasis is endoscopic clipping of the bleeding ulcer. In total, as a result of the treatment we used, 24 (8%) cases of repeated bleeding from the ulcer were observed. An analysis of cases of recurrent bleeding showed that the most common rebleeding was observed when the ulcer was localized along the lesser curvature of the stomach - 7 (2.3%) patients, as well as along the posterior wall of the antrum - 6 (2%) cases (Table 3). At the same time, we would also like to note that the volume of blood loss during recurrent bleeding from ulcers of the above localization was the highest, amounting to 972±389 ml for ulcers of lesser curvature, and 733±213 ml for ulcers of the posterior wall of the antrum.
|
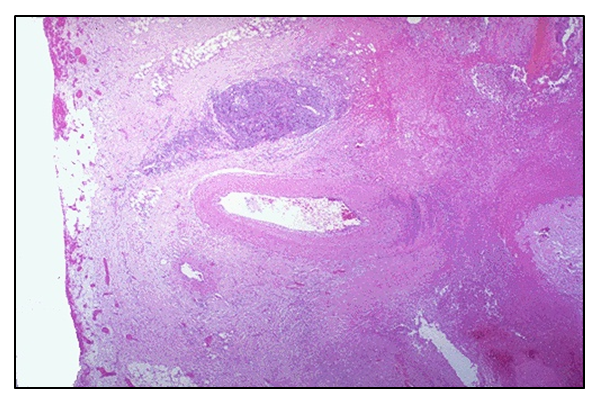
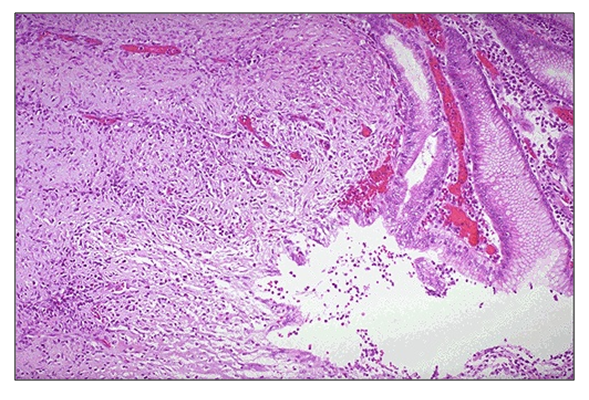 | Figure 1. The wall of the stomach. Biopsy from an ulcer along the anterior wall of the body of the stomach. Hematoxylin-eosin staining. Magnification: eyepiece 10, objective 20 |
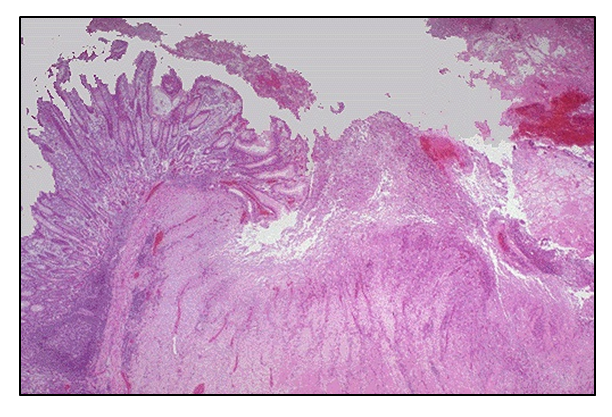
 | Figure 2. The wall of the stomach. Biopsy from an ulcer along the posterior wall of the antrum of the stomach. Hematoxylin-eosin staining. Magnification: eyepiece 10, objective 20 |
 | Figure 3. The wall of the stomach. Biopsy from an ulcer along the lesser curvature of the stomach. Hematoxylin-eosin staining. Magnification: eyepiece 10, objective 20 |
 | Figure 4. Acute ulcers associated H.pylori of the body of the stomach (the ulcer of the posterior wall is covered with a fresh thrombus) |
4. The Discussion of the Results
- Bleeding from an acute gastric ulcer is one of the most common upper gastrointestinal emergencies. The prevalence of acute gastric ulcers is 1.4% in the Western population and can be as high as 4.1% in Asia [5]. According to the UK National Audit in 2017, bleeding acute gastric ulcers accounted for 19% of all causes of acute bleeding from the upper gastrointestinal tract [6]. A systematic review by American authors reported the incidence of bleeding from acute ulcers, which ranged from 4 to 37 per 100,000 population per year [7]. In China, the prevalence of bleeding from acute gastric ulcers is not well understood, although this pathology is common. In hospital endoscopy studies conducted in Wuhan and Beijing, the prevalence of acute gastric ulcers was 5.7%, and the bleeding rate was estimated to be between 3.9% and 5.5% [8]. In an aging population (the number of people over the age of 60 will double in the next two decades) and with increasing urbanization, the prevalence of coronary and cerebrovascular diseases will increase and, consequently, the incidence of acute upper gastrointestinal bleeding associated with the use of aspirin and anticoagulants. When examining patients with acute upper gastrointestinal bleeding associated with aspirin and non-steroidal anti-inflammatory drugs, researchers reported a low level of adherence to gastroprotective drugs.In addition, acute erosions and ulcers of the upper gastrointestinal tract can occur as a result of stress in severe concomitant trauma, respiratory failure, extensive burns, sepsis, and other critical conditions. A distinctive feature of stress lesions of the mucosa is the relationship with physiological stress, the diffuse nature of the lesion and the variety of clinical manifestations. Within a few hours after stress, multiple flat punctate subepithelial bleeding mucosal defects with a diameter of 1-2 mm with a slight perifocal inflammatory reaction appear in the body and fundus of the stomach. Erosions can merge, forming significant defects of the mucous membrane with a diameter of 1-3 cm or more, without clear boundaries [9]. The lesions of the mucosa become deeper, the formation of acute ulcers is possible, in which the wall defect reaches the muscle layer.Acute gastric ulcer is a localized deep necrotic lesion affecting the entire thickness of the mucosa and the muscular layer of the mucosa. It is generally believed that these ulcers develop due to an imbalance between mucosal defense mechanisms and damaging factors on the intraluminal surface of the stomach.Ulcerogenesis begins with the destruction of the protective mucous layer formed by epithelial cells. The damage to the mucosal layer can lead to detachment of the surface epithelium and exposure of capillary endothelial cells in the underlying connective tissue. When the capillaries are damaged, there is a lack of oxygen and nutrients. As a consequence, hypoxic necrosis will occur in deep glandular cells, namely stem or progenitor cells, cervical mucosal cells, zymogen cells, enteroendocrine cells, and parietal cells. In addition, damaged macrophages, mast cells, and endothelial cells secrete vasoactive substances and pro-inflammatory mediators, which impairs mucosal microcirculation [10]. Necrosis of the epithelium and connective tissue eventually leads to the formation of ulcers, followed by the development of such a formidable complication as bleeding from the ulcer. According to various authors, mortality in bleeding from acute stress ulcers can reach 19-64% [11-13].Despite advances in anti-ulcer therapy and modern surgical techniques, the incidence of rebleeding remains high. According to the American Society of Gastroenterology, the frequency of rebleeding in acute gastric ulcers can be 3.7–38.4% [8,11–13].In general, the issues of tactics for the treatment of patients with acute ulcerative-erosive gastroduodenal bleeding are currently insufficiently developed, without taking into account the morphological and anatomical features of bleeding from acute gastric ulcers of various localization, and therefore high mortality rates remain both in our country and throughout the world.In the present study, to determine the ulcerogenesis of acute ulcers and the risk of bleeding, we studied the frequency of localization of acute gastric ulcers complicated by bleeding and the morphological structure of acute ulcers. Morphological studies have shown that acute ulcers located along the lesser curvature are deeper than ulcers located in other parts of the stomach. In addition, the vessels of acute ulcers of lesser curvature are located superficially, in the submucosal layer, while the vessels of acute ulcers of other parts of the stomach are located deeper, which determines not only a higher volume of blood loss, but also an increase in the frequency of recurrence of bleeding from ulcers of this localization. Besides, it is necessary to note the high incidence of recurrence of bleeding from acute ulcers located along the posterior wall of the cardiac section and the body of the stomach, which, in our opinion, is associated with insufficient visualization of the source of bleeding and endoscopic methods of hemostasis, in the presence of active bleeding and the presence of blood clots in the stomach.
5. Conclusions
- 1. Most often, acute stomach ulcers are located along the lesser curvature of the stomach, which is the main “food path” and are more susceptible to trauma.2. Most often, recurrent bleeding occurs from acute gastric ulcers, which are located along the lesser curvature in the area of the angle of the stomach, along the posterior surface of the body and the antrum of the stomach. The reasons for this circumstance are: the insufficiency of endoscopic visualization of the source of bleeding from acute ulcers located on the back wall of the cardiac section and the body of the stomach and the implementation of endoscopic methods of hemostasis, especially with ongoing bleeding and the presence of blood clots in the lumen of the stomach; a deeper spread of acute ulcers of the lesser curvature of the stomach into the underlying layers due to increased trauma.3. A qualitative assessment of the risk of bleeding depending on the location, area and depth of the spread of the ulcer is decisive in choosing the most adequate volume of surgical intervention and an effective method of hemostasis in bleeding from an acute gastric ulcer.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML