-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(10): 1022-1025
doi:10.5923/j.ajmms.20221210.02
Received: Sep. 15, 2022; Accepted: Sep. 28, 2022; Published: Oct. 12, 2022

Calcidiol (25-OH-D) Level in Serum of Patients with Chronic Pancreatitis
Aripova N. N. , Khamraev A. A. , Inoyatova F. Kh.
Tashkent Medical Academy, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic pancreatitis (CP) remains one of the most urgent problems in modern gastroenterology. In developed countries, the incidence of CP is 100 cases per 4000-8000 people per year. At the same time, the primary disability of patients reaches 15% and covers the population of working age. In specialized gastroenterology hospitals, patients with CP account for approximately 10% of hospital admissions.
Keywords: Chronic pancreatitis, Pancreatic insufficiency, Immunoenzyme, Vitamin D
Cite this paper: Aripova N. N. , Khamraev A. A. , Inoyatova F. Kh. , Calcidiol (25-OH-D) Level in Serum of Patients with Chronic Pancreatitis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 10, 2022, pp. 1022-1025. doi: 10.5923/j.ajmms.20221210.02.
Article Outline
1. Introduction
- It is mentioned in the scientific literature that CP is common among diseases of the digestive system and causes severe complications and death in most cases [1,4]. Absorption of dietary fats and fat-soluble vitamins is impaired and causes nutrient deficiencies in patients with chronic pancreatitis due to pancreatic insufficiency (PI). In patients with CP, the risk of vitamin D deficiency is on average 60%, and this condition, in turn, increases the risk of osteoporosis, muscle weakness, depression, and cardiovascular diseases [7].In recent years, cases of vitamin D deficiency have been observed to increase significantly in all regions of the globe, and this situation is associated with an increase in the incidence of chronic diseases, which necessitates the need to reconsider the approach to this issue. The widespread prevalence of conditions associated with vitamin D deficiency makes it necessary for scientists to carry out extensive research and research of patients [8]. To date, the role of some therapeutic diseases in the development of vitamin D deficiency has been shown [4]. This condition may be associated with reduced intestinal absorption of fats and fat-soluble vitamins, gluten enteropathy, and chronic pancreatitis or liver cirrhosis [4,6]. At the same time, increased catabolism or decreased synthesis of vitamin D and its metabolites can also lead to its deficiency. The purpose of the study: to determine the amount of vitamin D in chronic pancreatitis and to determine its effect on the course of the disease.
2. Materials and Methods of Research
- Researches were conducted in 94 (31 men and 63 women) patients aged 31 to 83 years (mean age 58.40±1.29 years) and 15 healthy subjects (mean age 39.73± 39.73) who were treated at the gastroenterology department of the multidisciplinary clinic of the Tashkent Medical Academy. 4.92 years) was conducted in humans. Patients were divided into the following groups according to the amount of calcidiol (25-OH-D), a metabolite of vitamin D in blood serum: group 1 those with 25-OH-D 30 ng/ml and above (normal), group 2 those with 25-OH-D 20- 30 ng/ml (deficiency), 3rd group - 10-20 ng/ml (deficiency), 4th group consisted of patients with 25-OH-D 10 ng/ml (obvious deficiency) and control group. According to the etiological factor of patients CP, biliary in 73 (77.7%), idiopathic in 8 (5.2%) and mixed etiology in 13 (13.8%) patients. Patients were subjected to clinical and anamnestic, instrumental, coprological and biochemical examinations. In order to determine the state of PI, UT examination was carried out on the "MINDRAY DC-60" device (manufactured in China). Osteopenia and osteoporosis are detected by ultrasound densitometer SONOST-3000 OsteoSys (South Korea). Deficiency of pancreatic exocrine secretory function was assessed by elastase 1 activity in feces, and the amount of 25-OH-D in blood serum was determined by immunoenzyme method in "ELIZA" immunoenzyme analyzer with special reagents of this company. The amount of calcium in the blood serum was determined in a biochemical analyzer using special biotests. Statistical analysis of the obtained results was performed using Microsoft Office Excel 2010 (Microsoft Corp., USA) and Portable Statistica 8 (StatSoft, Inc., USA). The description of categorical data was carried out in the form of degree indicators expressed in percentages. Given that most of the analyzed characteristics have a non-normal distribution, non-parametric statistical tests were used for statistical analysis of the obtained results. Correlation between the studied characteristics was evaluated using Spearman's rank correlation method (r – correlation coefficient). A significance level of 0.05 was assumed for statistical hypothesis testing.
3. Research Results and Discussion
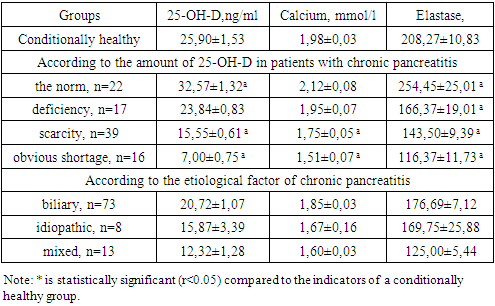
- The conducted studies showed that the amount of 25-OH-D in 22 (23.4%) patients was within normal values (32.57±1.32 ng/ml), 17 (18.1%) - partial deficiency (23.84±0.83 ng/ml), 39 (41.5%) - deficiency (15.55±0.61 ng/ml) and 16 (17%) - severe deficiency (7.00±0.75 ng/ml) were observed (1 see the table). In healthy people, the average amount of 25-OH-D was 25.90±1.53 ng/ml. When we analyzed the changes in the amount of 25-OH-D in the blood serum according to the etiological factor of SP, a tendency to decrease (20.72±1.07 ng/ml) was observed in the biliary form compared to the indicators of the conditionally healthy group, while in the idiopathic and mixed forms it was statistically reliable 1.63 (P <0.01) and 2.18 (P<0.001) were low and were 15.87±3.39 and 12.32±1.28 ng/ml. The obtained results showed that 19.4% of patients with CP biliary had normal 25-OH-D, 25% - partial deficiency, 44.4% - deficiency and 11.2% - obvious deficiency; in the idiopathic form, 75% of patients have a deficiency, and 25% have a severe deficiency; In the mixed form, 50% of patients have deficiency and 50% - severe deficiency. The obtained results substantiated that the strongest changes are observed in the mixed form of CP.It is worth mentioning that the amount of calcium in the blood serum of patients with CP also changed in parallel with the amount of 25-OH-D: in patients with a normal amount of 25-OH-D, its amount tended to increase compared to the indicators of a conditionally healthy group, while a deficiency of 25-OH-D was observed. and in patients with a tendency to decrease, in the groups of patients with deficiency and extreme deficiency, statistically significant 1.13 (P<0.05) and 1.31 (P<0.05) times decrease was observed. When we analyzed the changes in the amount of calcium in blood serum according to the etiological factor of SP, a tendency to decrease (1.85±0.03 mmol/l) was observed in the biliary form compared to the parameters of the conditionally healthy group, while in the idiopathic and mixed forms it was statistically reliable 1.19 (P<0.05) and 1.24 (P<0.05) times lower and amounted to 1.67±0.16 and 1.60±0.03 mmol/l. The obtained results showed that the changes in calcium metabolism are more specific in the mixed form of CP.At the same time, we performed ultrasound densitometry in patients suffering from CP. The obtained results showed that osteopenia and osteoporosis developed monad to 25-OH-D and calcium levels. Osteopenia symptoms were observed in 26.7% of the conditionally healthy group of tubular bone ultrasound examinations. 50 (53.2%) and 18 (19.1%) patients with CP showed osteopenia and osteoporosis. Among them, 9.1 and 9.1% of 25-OH-D were normal, 35.3 and 23.5% were deficient, 25.6 and 66.7% were deficient, and 25 and 75% of patients with severe deficiency. osteopenia and osteoporosis were observed. When we analyzed the results of ultrasound examinations according to the etiological factor of SP, 46.6% of osteopenia and 19.2% of osteoporosis were observed in the biliary form, 25 and 50% of these indicators were observed in the idiopathic form, and osteopenia was observed in all patients of the mixed form group (100%).It is known that the extrinsic secretory function of PI decreases in CP, and elastase activity in feces is considered as a criterion for its detection. Studies have shown that when serum vitamin D levels of patients with CP were normal, elastase activity in feces was 1.22 (P<0.05) times higher than that of the healthy group, while its activity was 1.25 (P<0.05) in patients with deficiency, deficiency, and marked deficiency 0.05); 1.45 (P<0.01) and 1.79 (P<0.001) times lower (Table 1). The obtained results proved that 25-OH-D deficiency in CP patients can be caused by the external secretory function of MOB. When we analyze the activity of elastase in feces by etiological factor, it is statistically reliable 1.18 (P<0.05) in biliary, idiopathic and mixed forms of CP; We observed a decrease of 1.23 (P<0.05) and 1.67 (P<0.01) times. The obtained results showed a sharp decrease in the external secretory function of PI in the mixed form of CP.
|
|
|
4. Conclusions
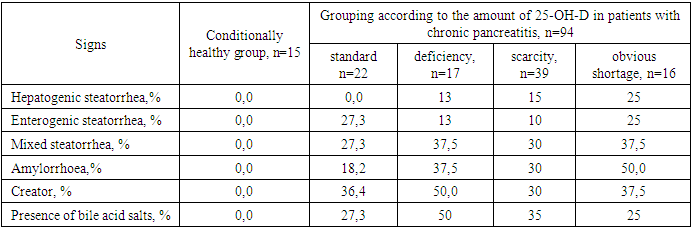
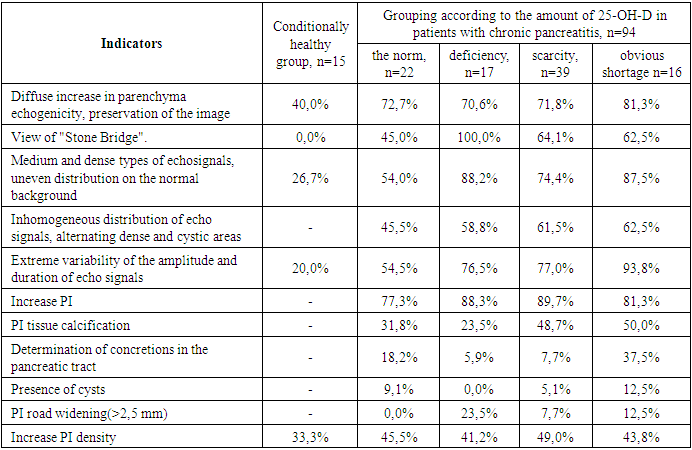
- Based on the obtained results, we can make the following conclusions:1. In the majority of patients with chronic pancreatitis, a deficiency of 25-OH-D, as well as a pronounced deficiency, was found, which led to a decrease in the amount of calcium in these patients, which led to the development of osteopenia and osteoporosis.2. The degree of 25-OH-D deficiency coincided with a decrease in the exocrine secretory function of the pancreas.3. In patients with 25-OH-D deficiency, ultrasound examinations reveal fibrosis and calcification of the pancreas parenchyma, and stool examinations record hepatogenic steatorrhea and malabsorption of fat-soluble vitamins.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML