-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 994-996
doi:10.5923/j.ajmms.20221209.30
Received: Sep. 5, 2022; Accepted: Sep. 25, 2022; Published: Sep. 29, 2022

Special Pathomorphological Changes in Children with Lymphocytic Leukemia
Zulfiya Salayeva
Assistant of Department of Hospital and Outpatient Pediatrics of Urgench Branch of Tashkent Medical Academy, Uzbekistan
Correspondence to: Zulfiya Salayeva, Assistant of Department of Hospital and Outpatient Pediatrics of Urgench Branch of Tashkent Medical Academy, Uzbekistan.
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

First of all, leukemia cells appear in the organ stroma, then infiltrate the parenchyma. Acute lymphblastic leukemia in children is the most common cancer in children aged 2-5 years. The main clinical and morphological sign is the large production of lymphocytic cells from the bone marrow. The disease is very severe and often leads to death. It is therefore important to identify and recognize the initial signs of the disease. Every year, 50 out of a million children are infected with the disease. Blood and lymph tissue tumours account for half of all malignant tumours, of which between 38 and 40% are leukemia. Of the 100,000 children under the age of 15,4.1 ± 0.4 suffer from acute lymphocytosis, with boys and girls at a ratio of 1.3 to 1, and 2 to 5 years at most. Modern diagnosis of acute lymphocytosis is based on the FAB classification, whose main criterion is morphological and cytological confirmation of blood vessels. In the sample of bone marrow from 25 to 30% of blasts were diagnosed with acute leukemia, with 3 types of cells identified: L1, L2, L3. 85% of acute lymphblasts were L1, 14% L2, and 1% L3. The main diagnostic method is cytomorphology. Trepan biopsy should be obtained from the iliac bones, and the diagnosis is confirmed by the presence of poorly differentiated blast cells in the histological preparation.
Keywords: Path morphological, Lympholecosis, Tissue tumours, Cytomorphology, Lymphocytic, Polyclinic
Cite this paper: Zulfiya Salayeva, Special Pathomorphological Changes in Children with Lymphocytic Leukemia, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 994-996. doi: 10.5923/j.ajmms.20221209.30.
Article Outline
1. Introduction
- The aim was to study the path morphological changes in lympholecosis in children. Lympholecosis in children is manifested by the appearance of focal leukemic infiltrates in the bone marrow and all lymphatic organs. Depending on the origin of lympholecosis from T, or from B lymphocytes, leukemic infiltrates are localized in T or B zones.
2. Materials and Methods
- To achieve this goal, over the past 10 years (2009-2018) the National Institute of Hematology and Blood Transfusion has been studying the material for the autopsy of children who died of lymphocytosis. During this time, the Institute's polyclinic treated 2568 sick children with lymphocytic leukemia, 84 of whom died. Of these, 37 were girls and 47 were boys. By age: 12 died before the age of 2 years, 28 died before the age of 4 years, 26 died before the age of 6 years and 18 died before the age of 10 years. The deceased's medical history, laboratory data, autopsy report and internal organ fragments were analyzed, their histological preparations were examined under a microscope, and photographs and details were taken.
3. Results of Research
- The bone mass study, which was based on the study of bone mass, revealed that, depending on the level of leukemia, the blanket leukemia cells, if lightly shaped, were concentrated in foci and in severe form infiltrated almost all bone burial sites. Hypoplasia of blood vessels, necrosis and other bone marrow cells are often found.Thymus. A feature of lymphocytic leukemia in children is that in almost all cases, the thymus has grown to some extent, and in some cases weighs about 30 grams. The slices appeared to be almost the same size, in a soft grayish-gray colour, in some cases the pieces were bound together and small blood vessels appeared on the surface. When examined under a microscope, thymus slices were of different sizes, with enlarged tissue and leukemia cells appeared around the blood vessels. It was noted that the thymus parenchyma was infiltrated by leukemia cells only in T-lymphocytes. At the same time, the slice lining was slightly enlarged, which revealed diffuse leukemia cells (Fig. 1). The mucous membrane is concentrated only around the blood vessels, Gassal's bodies were enlarged and the number of necrosis in the body was increased.
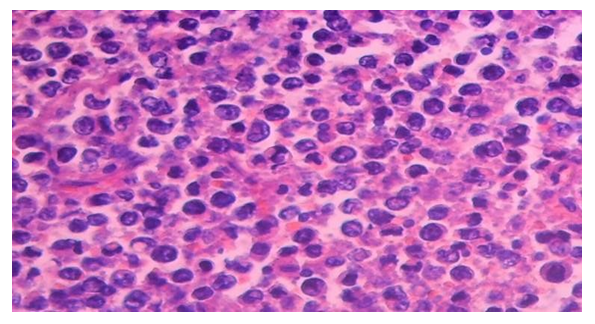 | Figure 1. Timus. Lymphoblastic leukemic infiltration. paint: G-E. X: 10 x 40 |
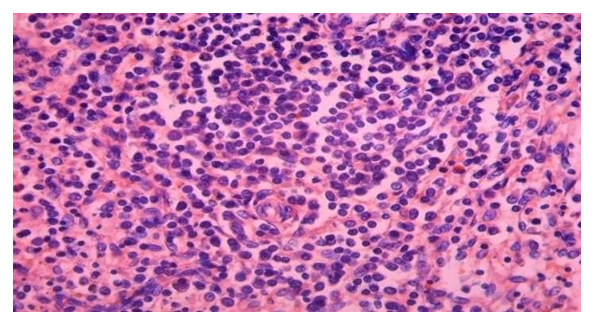 | Figure 2. Leukemic infiltration in the periarterial area. paint: G-E. X: 10 x 20 |
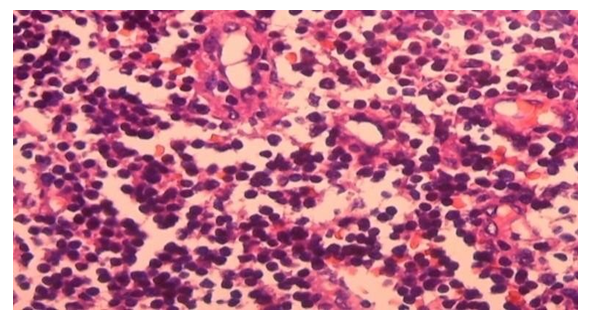 | Figure 3. Lymph node Leukemic infiltration of paracortical industry. paint: G-E. X: 10 x 40 |
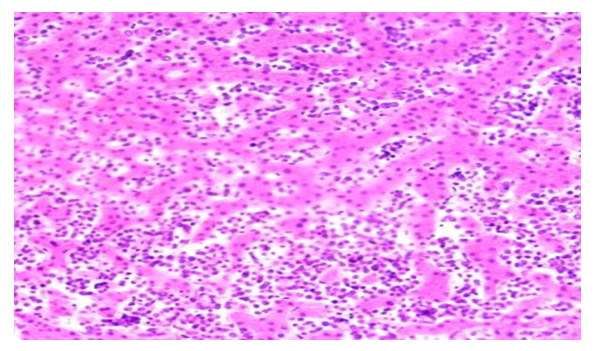 | Figure 4. Liver Leukemic infiltration of the disein space. paint: G-E. X: 10 x 20 |
4. Discussion
- It should be noted that pathomorphologically specific signs of lymphocytic leukemia in children are bone marrow, thymus, spleen, lymph nodes and even liver [1,4,7]. In the bone marrow, the disease is most often manifested by fistula leukemia infiltration, which is different from other types of leukemia. In the thymus, the data are clear: leukemia infiltration, mainly in T-lymphocytic leukemia, begins with intermediate thymus tissue and then spreads to parenchyma, often leukemia infiltration of the cortex. Specific pathomorphological changes in the spleen are that, depending on the type of lymphocytic leukemia, T-lymphocytic leukemia is predominantly a marginal area, and in the periarticular area subjected to leukemic infiltration, changes in B-lymphocytic leukemia are followed by complete lymph follicles. Depending on the type of leukemia in lymph nodes, leukemic infiltration in T-lymphocytes predominates in the paracortical region, whereas in B- lymphocytosis most of the lining is covered by leukemic infiltration of the cortical follicles. In both types of lympholecosis, small changes are observed in the liver, mainly with perisinusoidal mission and central venous leukemia infiltration.
5. Conclusions
- 1. Child lymphocytic leukemia is pathomorphologically characterized by bone burial and leukemia infiltration in almost all lymphatic organs at the beginning of the disease.2. Lymphocytic leukemia is characterized by leukaemic infiltration in certain areas of the lymphatic organs, depending on whether T or B develops from lymphocytes.3. Pathomorphological changes in lymphocytic leukemia first appear in the stroma vascular structures of the organs, and then extend to the parenchyma.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML