-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 991-993
doi:10.5923/j.ajmms.20221209.29
Received: Aug. 22, 2022; Accepted: Sep. 10, 2022; Published: Sep. 29, 2022

Comparative Study of Calprotectin in Feces and Interleukin-6 in the Blood of Patients with Covid-19
M. I. Ismoilova1, A. G. Gadayev2
1Fergana Medical Institute of Public Health, Fergana, Uzbekistan
2Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

100 patients were observed, of whom 60 were relatively recovered from Covid-19 and 40 haven’t had the infection. In patients who have had coronavirus infection, the levels of calprotectin in feces and interleukin-6 in the blood were significantly higher. This confirms that Covid-19 patients need rehabilitation measures.
Keywords: COVID-19, Calprotectin, Interleukin-6
Cite this paper: M. I. Ismoilova, A. G. Gadayev, Comparative Study of Calprotectin in Feces and Interleukin-6 in the Blood of Patients with Covid-19, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 991-993. doi: 10.5923/j.ajmms.20221209.29.
1. Introduction
- It has been stated by some researchers, that the first wave of Covid-19 infection affected mainly the respiratory system, and in the second wave, the symptoms of the gastrointestinal system were more characteristic [5,8].In 2019, RNA of the coronavirus was isolated for the first time in the USA from the stool of a 35-year-old patient who came with complaints of nausea, vomiting, and diarrhea on the 7th day of the disease [2].According to a number of studies, the RNA of Covid-19 is detected from the 5th day of the disease, and its peak corresponds to the 11th day. In the feces of some patients, RNA is preserved even after the respiratory symptoms disappear and the appropriate tests from the respiratory organs are negative [1,6,7,9,10,11,12].Moreover, although there are opinions that the detection of Covid-19 RNA in feces is not a sign of long-term retention of the infection in the gastrointestinal system [7], there are other data contradictory to that. It is known that the coronavirus enters the body through angiotensin-converting enzyme (ACE 2) receptors. Their high expression is observed not only in alveolar lung cells, but also in gastric, duodenal, and rectal glandular epithelial cells [3,4,13] and this in turn may cause gastrointestinal symptoms in this infection [9].As it is known that the evaluation of inflammatory processes and permeability in the intestines of patients with Covid-19 is of great practical importance. In recent years, the use of calprotectin has been recommended for this purpose. Calprotectin is a small calcium-binding protein with a molecular weight of 36 kDa and consisting of two heavy and two light polypeptide chains. The protein contains calcium and zinc and has an in vitro bacteriostatic and fungicidal effect. Calprotectin is found in neutrophils in abundance and makes up 60 percent of its cytosol fraction. It is also present in the cytoplasm of monocytes and macrophages. This protein is a product of neutrophilic granulocytes and its detection in feces indicates the existence of an inflammatory process in the intestinal walls. Since calprotectin is considered a stable protein that is degraded very slowly by microorganism proteases, it can be detected in feces. Therefore, it is a reliable marker of "fecal inflammation."In the literature we studied, there is limited information on the changes observed in patients "relatively recovered" from Covid-19 with comorbid diseases of various internal organs, including gastrointestinal system. However, their timely detection and secondary prevention procedures are of great practical importance. Therefore, we aimed to study the state of digestive organs in this group of patients using calprotectin in feces and interleukin-6 in blood.
2. Materials and Methods of the Study
- In accordance with the aim of the study, 100 patients with gastrointestinal symptoms were observed. 42 of them (42%) were men and 58 (58%) were women. Patients were divided into 2 groups. The first group consisted of patients "relatively recovered" from Covid-19 with no detected immunoglobulin M but with of gastrointestinal symptoms (27 men and 33 women; average age 55.06 ± 2.1 years). The second, i.e. control group, consisted of patients, who did not have Covid-19 but had gastrointestinal symptoms (15 men and 25 women; average age 63.4 ± 1.5 years).The levels of calprotectin in feces and interleukin-6 in the blood of patients involved in the study were measured:Calprotectin was in feces evaluated in mgs by "sandwich" method (ELISA) using diagnostic kit RIDASCREEN Calprotectin immunoenzymatic test (R-Biopharm, Germany).In order to evaluate serum interleukin-6 (IL-6) levels, a package of 96 tests of by the company "VECTOR-BEST АО " (Russia) was used. This kit is based on the quantitative determination of the above-mentioned cytokine in human blood serum using an immunoenzymatic assay. For data processing MS Excel (2016) computer program was used. Arithmetic mean and standard deviation (M±m) of all data in following tables were calculated. To determine significance of difference between groups Student’s paired and unpaired t-tests for quantitative indices. Correlation analysis was done using Pearson’s correlation coefficient and confidence tables. Differences were considered to be statistically significant when р<0.05.
3. Analysis of the Study Results
- It is of great practical importance to evaluate inflammatory processes and permeability in the intestine of patients with Covid-19 and to restore it. For this purpose, we conducted a series of special biochemical examinations in our patients before the treatment procedures and studied the correlations between them.The increase of cytokines in the blood of patients infected with Covid-19 has been found in a large number of observations. Even the term "cytokine storm" has been coined in medicine to describe the cause of death of patients suffering from coronavirus in many cases. However, until now, there is not enough information on the dynamic changes of inflammatory cytokines, in particular interleukin-6, in patients who have clinically recovered from Covid-19. Moreover, their relationship with inflammatory markers in the intestinal wall, in particular calprotectin, has not been studied. In our observation, the reliable positive correlation between interleukin-6 and calprotectin confirms that inflammatory cytokines persist for a long time and cause inflammatory processes in intestinal walls even in patients who have clinically recovered from coronavirus infection (Fig. 1).
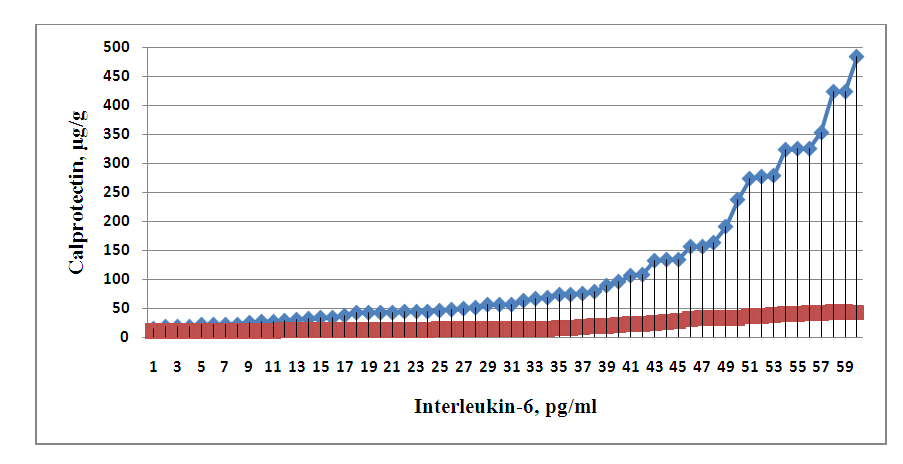 | Figure 1. Correlation between interleukin-6 and calprotectin in patients clinically recovered from Covid-19 |
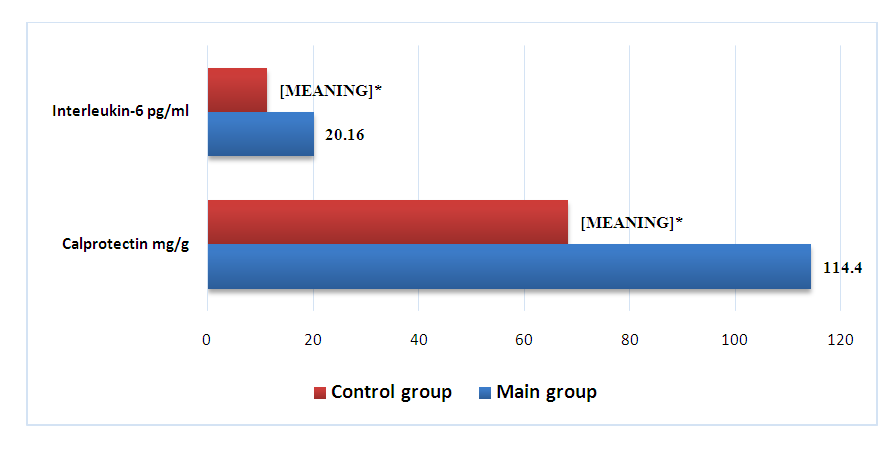 | Figure 2. Interleukin-6 and calprotectin levels of patients of the main (who have had Covid-19) and the control (who haven’t had the infection) groups (* - p<0.05) |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML