-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 958-962
doi:10.5923/j.ajmms.20221209.23
Received: Aug. 26, 2022; Accepted: Sep. 12, 2022; Published: Sep. 23, 2022

Predictors of Heart Failure Progression after Various Delivery Types in Pregnant Women with Myocarditis
Kamola Abdullajonova1, Zufar Abdurakhmanov2
1Department of Gynecology №1, Republican Specialized Scientific-Practical Medical Center of Obstetrics and Gynecology, Tashkent, Uzbekistan
2Department of Surgical Diseases and Intensive Care, Bukhara State Medical Institute, Bukhara, Uzbekistan
Correspondence to: Zufar Abdurakhmanov, Department of Surgical Diseases and Intensive Care, Bukhara State Medical Institute, Bukhara, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

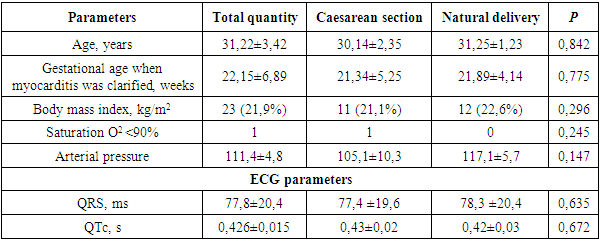
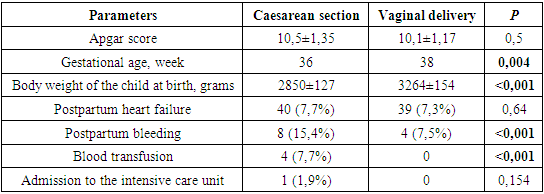
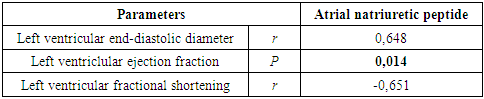
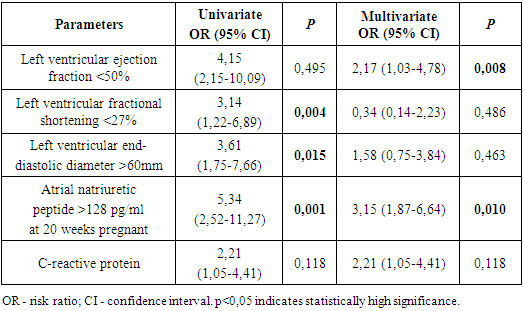
Objective. To study of predictors of transition from NYHA I to NYHA II heart failure (HF) or deterioration in general condition after various types of delivery in pregnant women with myocarditis. Materials and methods. This retrospective analysis included pregnant women with NYHA I myocarditis (n=105) who were hospitalized in the department of gynecology №1 between July 2020 and February 2022. Echocardiographic data were collected and their correlation with the level of atrial natriuretic peptide and C-reactive protein (CRP) in plasma were analyzed. The receiver operating characteristic curve (ROC) was used to determine the endpoints of the study. Univariate and multivariate analyzes were used to evaluate significant prognostic variables for the transformation of NYHA I to NYHA II heart failure in the postpartum period. Results. Caesarean section was performed in 52 pregnant women (49,5%). Planned vaginal delivery was performed in 53 women (51,5%). Apgar scores were not significantly different between women who underwent caesarean section and vaginal delivery (10,5 vs. 10,1; p=0,5). Gestational age (37 vs. 38 weeks; p=0,004) and birth weight (2850 vs. 3164 g, p<0,001) were lower in women who had a caesarean section. Elective caesarean section did not significantly differ from women who gave birth vaginally in terms of postpartum HF (7,7% vs. 7,5%, p=0,64) or postpartum hemorrhage (5,7% vs. 1% p=0,61). Baseline atrial natriuretic peptide positively correlated with left ventricular end-diastolic diameter (r=0,648; p<0,001) and inversely correlated with left ventricular ejection fraction (r=-0,651; p<0,001) and with fractional shortening (r=-0,531; p<0,001). ROC curve data showed that the cut-off level of atrial natriuretic peptide level is higher than 75,54 pg/ml (95% CI, 54,7–98,6; p=0,024) for HF in the postpartum period. Multivariate analyze confirmed that the concentration of atrial natriuretic peptide greater than 75,54 pg/mL (95% CI, 54,7–98,6; p=0,024) is an independent predictor for the transformation of NYHA I to NYHA II HF in the postpartum period. Conclusions. The findings suggest that elective caesarean section compared to vaginal delivery does not show any benefit in terms of freedom from postpartum HF and bleeding, optimal gestational age, birth weight, which justifies vaginal delivery for all pregnant women with myocarditis and NYHA I. Plasma atrial natriuretic peptide has a good predictive value for predicting the onset of HF regardless of delivery method.
Keywords: Myocarditis, Delivery, Heart failure, Postpartum
Cite this paper: Kamola Abdullajonova, Zufar Abdurakhmanov, Predictors of Heart Failure Progression after Various Delivery Types in Pregnant Women with Myocarditis, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 958-962. doi: 10.5923/j.ajmms.20221209.23.
1. Introduction
- Myocarditis in pregnant women is one of the most formidable and life-threatening conditions in cardiology. At the same time, the prevention of sudden death and other complications (long-term persistent dysfunction of the left ventricle (LV), dilated cardiomyopathy, pulmonary embolism) are far unresolved issues in pregnant women with myocarditis [10]. However, the diagnosis of myocarditis is difficult due to the heterogeneity of the clinical manifestations of the disease, which is often non-specific and can vary from asymptomatic and often non-specific electrocardiographic abnormalities observed in Coxsackie B virus or out-patient influenza outbreaks, up to severe dilated cardiomyopathy with fulminant HF, leading to transplantation or death [2]. Modern laboratory diagnostics is also not always informative, especially in the first phase of myocarditis development when myocardial damage occurs without an immune response [3,13].Several publications have demonstrated a relatively high incidence of histologically confirmed myocarditis in patients with peripartum cardiomyopathy. These findings have led to the suggestion that myocarditis is considered an important etiological factor in patients with peripartum cardiomyopathy [1,5]. Some authors inform that myocarditis is associated with deterioration of endothelium-dependent vasodilation in response to the presence of acetylcholine. It may explain the occurrence of myocardial ischemia as a result of endothelial dysfunction of coronary arteries [1,9]. As a result, the relevance of the issue of myocarditis in pregnant women is not only determined by such a frequent complication as dilated cardiomyopathy but also by a high mortality from this complication in the postpartum period, as well as the difficulties of timely diagnosis of ischemic heart disease, differential diagnosis in terms of cardiomyopathy and the correct choice of the method of delivery, methods for diagnosing and predicting the degree of HF progression based on the use of a modern diagnostic algorithm [4,10,12]. The peculiarity of these studies at the present stage is, on the one hand, in an in-depth study of the relationship between echocardiographic data of the heart and HF in the postnatal period, and on the other hand, in obtaining fundamentally new important information based on the analysis of the significance of various predictors of the further or reverse progression of HF which largely determines the life quality of women with myocarditis after delivery [5,16].Recently, an inflammatory marker - CRP, a marker of HF - NT-proBNP (N-terminal pro-brain natriuretic hormone) has been increasingly recognized as predictors of persistent systolic dysfunction of the LV, which is of particular interest in a comprehensive study of their relationship with the peripartum clinical course of myocarditis [10,14,17]. The aim of the study was to identify the predictors of transition from NYHA I to NYHA II after various methods of delivery in pregnant women with myocarditis.
2. Materials and Methods
- The sample size was 250 pregnant women with myocarditis. Based on the inclusion criteria (NYHA I), this retrospective study included 105 pregnant women with myocarditis aged 24 to 40 years who were hospitalized at the Republican specialized scientific and practical medical center for obstetrics and gynaecology from July 2020 to February 2022. Exclusion criteria were NYHA II, III, and IV, all types of congenital heart disease, and comorbidities. Informed consent was obtained from the patients.The collection of information regarding labor includes the planned method of delivery, the applied delivery method, the period of gestation, complications during childbirth.The endpoints for this study were maternal death, postpartum HF, postpartum haemorrhage (when delivered vaginally >500 ml, caesarean section >1000 ml or requiring transfusion), length of pregnancy, occurrence of preterm labor (spontaneous onset of labor <37 weeks gestation) and birth weight.Echocardiographic data and their correlation with the level of atrial natriuretic peptide and CRP in plasma were collected. The study of atrial natriuretic peptide was performed at the 20th week of pregnancy. 24-hour blood pressure monitoring was carried out using autonomous operation of ASUS VivoWatch BP 4-5 times a day and background monitoring every 15 minutes.
3. Results
- The general clinical characteristics of pregnant women, taking into account the method of delivery, are presented in Table 1.
|
|
|
|
4. Discussion
- It is obvious that one of the most important issues of modern cardiology, which underlies the prevention of sudden death in myocarditis in pregnant women, is the prediction of myocarditis progression, clarifying the new predictors of an unfavorable outcome of this disease [6,7,17-19].Basing on our data, it can be concluded that elective caesarean section compared to vaginal delivery does not show any advantage in terms of freedom from postpartum HF and admissions to the intensive care unit, however, was statistically significantly inferior to vaginal delivery in terms of the presence of cases of postpartum hemorrhage, optimal gestational age, body weight of the child at birth that justifies vaginal delivery in all pregnant women with myocarditis and NYHA I.The results of this study revealed the fact that the level of atrial natriuretic peptide has a positive correlation with the end-diastolic diameter of the LV and a negative correlation with the left ventricular ejection fraction shortening fraction, which has a predictive value for detecting the transformation of NYHA I into NYHA II in postpartum period.According to the analysis of ROC curves, left ventricular ejection fraction <50%, left ventricular shortening fraction <27%, left ventricular end-diastolic diameter >60 mm, atrial natriuretic peptide >128 pg/ml and C-reactive protein >4 mg/l are study endpoints to predict worsening HF. Basing on the data of multivariate regression, of 4 predictors, left ventricular ejection fraction <50%, atrial natriuretic peptide >128 pg/ml are independent predictors of the transformation of NYHA I into NYHA II in the postpartum period, which are 2,17 and 3,15 times, respectively increase the risk of worsening HF.
5. Conclusions
- As caesarean section showed itself non-superior versus vaginal delivery in terms of postpartum heart failure, admission to the intensive care unit, and inferior regarding gestational age, child body weight at birth, postpartum bleeding, vaginal delivery is considered as a safe labor method in women with non-progressive NYHA 1. Determining the 2 predictors (ejection fraction <50%, atrial natriuretic peptide >128 pg/ml) may help identify worsening HF in pregnant women with myocarditis. Accordingly, prenatal diagnosis at week 20 based on echocardiography and identification of a marker of HF may help identify pregnant women at high risk of further development of HF and provide timely conservative therapy with subsequent improvement in left ventricular systolic function and a possible reduction in maternal death. In addition, future studies should focus on analyzing the marker of cardiac muscle breakdown and identifying its correlation with echocardiographic parameters of left ventricular systolic function and the level of atrial natriuretic peptide, as well as the effect of conservative treatment of myocarditis on the above values in the postnatal period.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML