Bakhrom M. Mamatkulov1, Bakhodir Sh. Turayev1, Bakhora V. Urinova2
1School of Public Health, Tashkent Medical Academy, Tashkent, Uzbekistan
2Faculty of Treatment, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Bakhodir Sh. Turayev, School of Public Health, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Medico-biological and socio-hygienic factors were studied in 300 men who sought medical help for problems with conception and the manifestation of pathological changes in the spermogram, as well as 300 men with normal spermogram parameters (control group). The data of both groups were compared and the odds ratio was estimated. As a result of the study, it was found that the leading risk factors that negatively have an effect on the male reproductive system are unfavorable living conditions, low material security, low physical activity, bad habits, poor nutrition, promiscuity, overweight or obesity, mumps and the presence of a varicocele.
Keywords:
Reproductive health, Infertility, Male infertility, Spermogram, Risk factors
Cite this paper: Bakhrom M. Mamatkulov, Bakhodir Sh. Turayev, Bakhora V. Urinova, Assessment of Risk Factors Affecting the Reproductive Health of Men Living in Uzbekistan, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 953-957. doi: 10.5923/j.ajmms.20221209.22.
1. Introduction
Currently, human health is affected by many endogenous and exogenous factors. The reproductive system is particularly vulnerable to factors that adversely affect health. In recent years, there has been a decline in the quality of human sperm. Studies show that this problem of reproductive health is becoming more relevant among men in different countries [3,8].Despite evidence of declining sperm counts worldwide and an increasing prevalence of male infertility, documentation of potential causes and risk factors for male infertility is limited [4].It is conditionally possible to group all factors influencing the male reproductive system into uncontrollable (age, congenital and genetic factors) and controllable (lifestyle, working conditions, environmental factors). When determining the risk of developing the disease, the interaction of these factors should also be taken into account, since in most cases in male infertility, an interaction of 2-3 or more factors can be observed [1,3,6]. More research in recent years has demonstrated the negative impact of environmental and lifestyle factors on male fertility. In particular, smoking, diabetes, psychological stress, drug or alcohol, endocrine disruptors, and nutrition have been shown to have detrimental effects on sperm parameters [7,9].The negative impact of numerous potential risk factors that can impair male fertility may well be largely overcome through behavioral change and better lifestyle choices, as well as improved health education [4].An examination of the literature review indicates the limited knowledge of the actual causes of male infertility in published studies. Gaps in knowledge have been noted that need to be addressed in order to better understand the actual causes of male infertility. Researchers believe that a better understanding of the causes of male infertility will help determine more effective methods for the primary prevention and treatment of male infertility [2,3,5].
2. Aim
Study and evaluation of socio-hygienic and biomedical risk factors affecting male reproductive health.
3. Materials and Methods
By questioning the medical, biological and socio-hygienic characteristics of 300 men (main group) who had pathological changes in the spermogram and 300 men with normal spermogram parameters (control group) who applied to the Republican Specialized Scientific and Practical Medical Center of Obstetrics and Gynecology for problems with childbearing were studied and analyzed. The results obtained were compared (odds ratio) and their significance was assessed (p, Student's t-test, chi-square test).
4. Results and Discussion
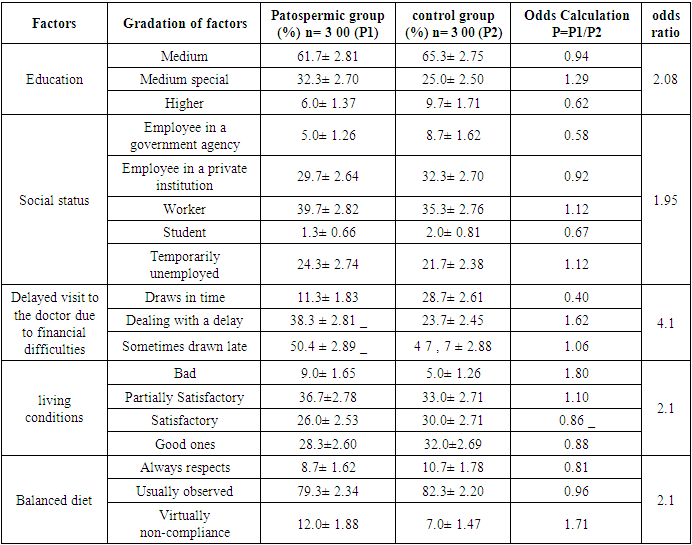
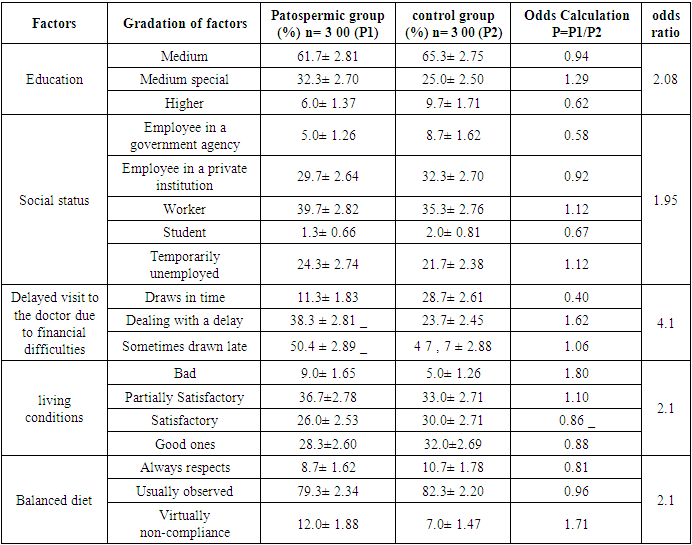
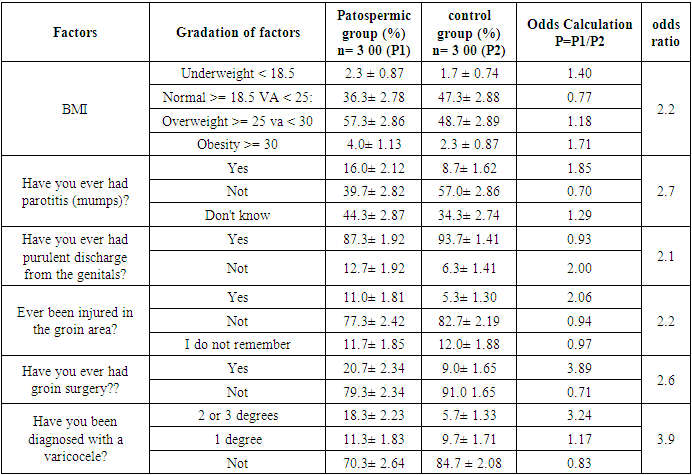
Age is one of the important factors affecting male reproductive health. The average age of men who sought medical help for infertility and identified changes in spermogram was 30.9±0.33 years, for men with normospermia -29.7±0.31 years. The average duration of childlessness was 2.85±0.14 years. According to the results of our research, the average age of marriage for men was 25.1±2.0 years, and for women 21.2±2.0 years. the majority of men (58%) started a family at the age of 24-29, and women at the age of 21-25 (63%). The age at which men started a family was almost 4 years higher than that of women.The analysis of the obtained data on the social status and living conditions of the respondents is presented in the following table (Table 1). Table 1. Odds ratio of male infertility by social factors
 |
| |
|
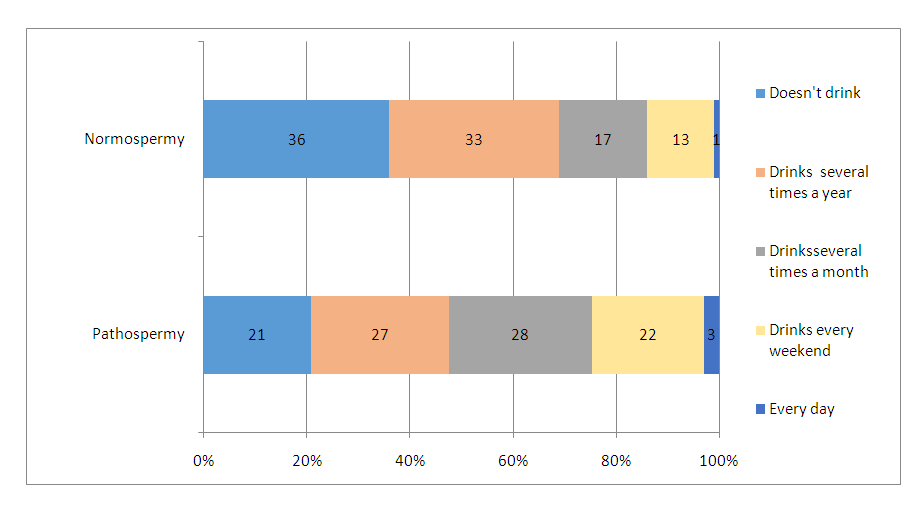
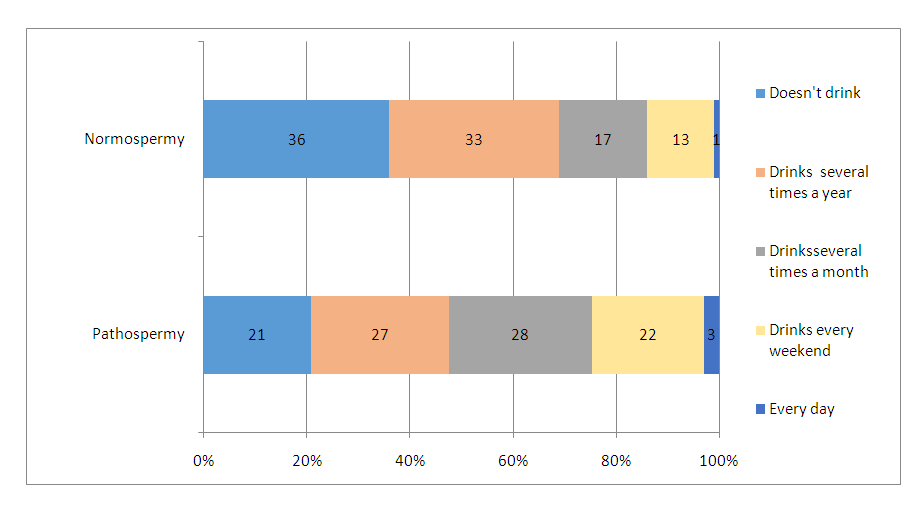 | Figure 1. Alcohol consumption by respondents |
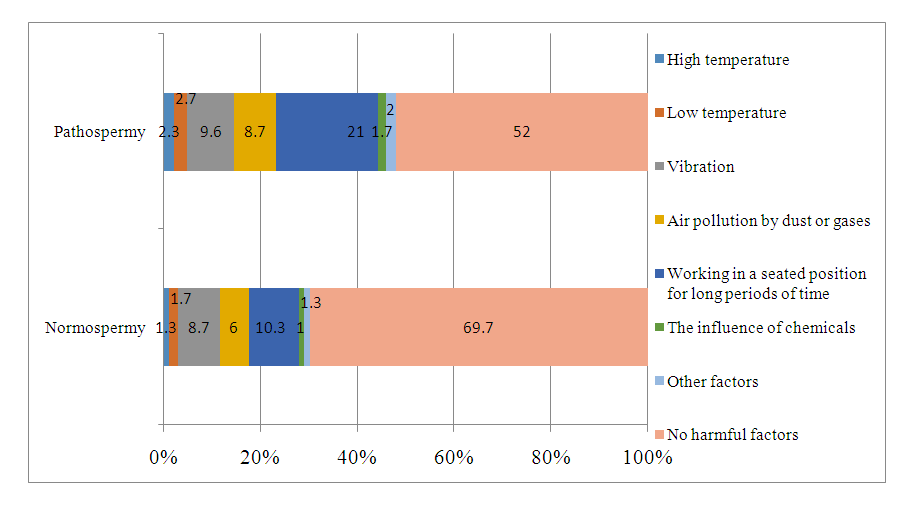
In both study groups, men with secondary and secondary specialized education made up the majority of the respondents. Among men diagnosed with pathospermia, there were 1.61 times fewer people with higher education than men with normospermia, and 1.3 times more people with secondary specialized education. No statistically significant relationship was found between the level of education and infertility (n'=2, χ2=5.706, p=0.058). In turn, no statistical relationship was found between social status and pathospermia/normospermia (p=0.297).To study the relationship between living conditions and the reproductive health of men, we used a form for assessing housing conditions developed by scientists in our country, summarizing the type of house, living space, provision with communal and sanitary and hygienic conditions, and hygienic condition (B. Mamatkulov, 2013). In accordance with it, the studied families were divided into poor, partially satisfactory, satisfactory and good groups. According to the results obtained, it was shown that in the group of pathospermia, people living in unfavorable living conditions are 1.8 times more likely than those with normospermia, and compared with people living in very good conditions, the probability of getting sick is 2.1 times higher (p=0.047).Among the men of the normospermic group, the daily consumption of meat products was 1.3 times more common than in the pathospermic group. It has been established that in the group of pathospermia, persons who rarely consume meat products are found 1.5 times more often than in the group of normospermia. Sufficient consumption of meat products can have a positive effect on spermogram parameters (n'=3, χ2=9.720, p=0.022). It was found that men of the normospermic group consume more fruits and vegetables (n'=3, χ2=11.039, p=0.012).In the study of smoking tobacco products, 38.67±2.81% of respondents from the pathospermic group and 30.67±2.66% of the normospermic group reported the presence of harmful inoculations as smoking. A statistically significant relationship was found between smoking and pathospermia (p=0.040). It should be noted that 84.62±2.50% of smokers also consume alcohol, while a combined effect of two harmful factors is observed.The results of the study of harmful factors associated with the profession of the respondents are presented in the following figure (Fig. 2).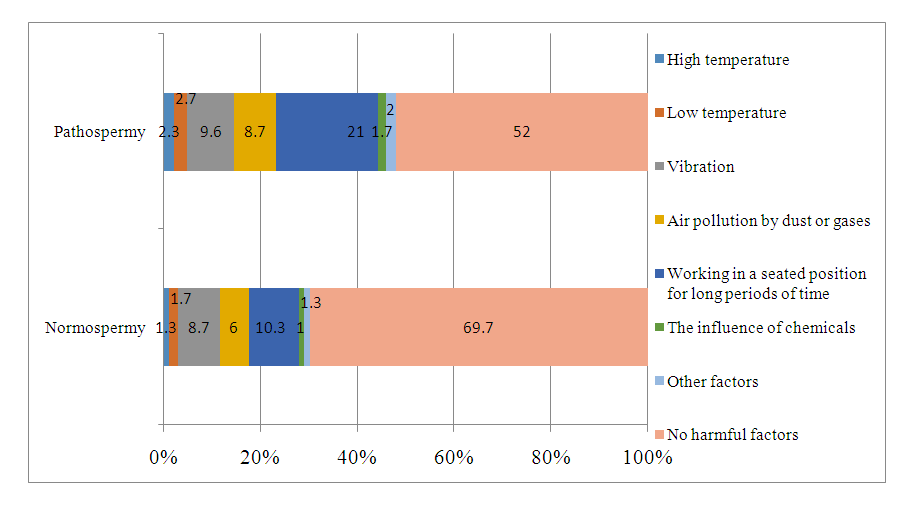 | Figure 2. Leading risk factors associated with working conditions that affect reproductive health |
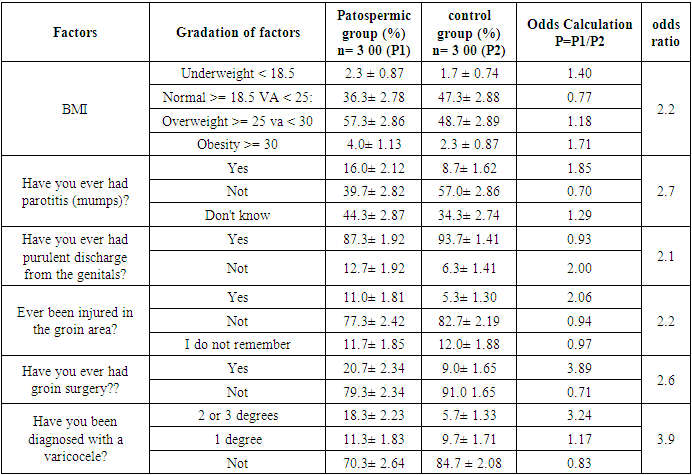
The absence of harmful factors associated with working conditions was reported by 52.0±2.88% of respondents in the pathospermia group and 69.7±2.73% in the normospermia group. Among the harmful factors associated with professional activity, a long sitting working posture attracts attention (21.0±2.35% in the pathospermia group and 10.3±1.76% in the normospermia group). Statistical analysis of the obtained data shows that occupational hazards can negatively affect reproductive health (OR = 2.03, p<0.01).In the group of normospermia, 19.0±2.26% of the respondents stated that they go in for physical culture every day. In the group of pathospermia, this figure is 10.3±1.76% and is almost 2 times lower than in the group of normospermia. Regular exercise has a positive effect on the reproductive system. At the same time, the duration of physical culture lessons is also of great importance, the proportion of respondents who add 30 minutes to the duration of each workout was 65% in the normospermia group and 43% in the pathospermia group (p = 0.010).In those who started sexual activity before the age of 18, the probability of pathological changes in the spermogram is 1.5 times higher than in those who started after 18 years (p=0.034). In the group of pathospermia 15.3±2.08% of respondents and in the group of normospermia 10.7±1.78% use the services of commercial sex several times a year, and their risk of developing pathospermia is 1.8 times higher than it used to be. we use these services.Data on the medical and biological status of the respondents is presented in the following table (Table 2).Table 2. Data on the medical and biological status of the respondents
 |
| |
|
Diabetes mellitus was detected in 2 patients in the group of pathospermia and is 0.7±0.4%. Respondents with normospermia do not have diabetes mellitus.Varicocele was detected in 29.7% of patients in the pathospermia group and in 15.3% in the normospermia group. Grade 1 varicocele occurred with almost the same frequency in both groups, but grade 2 varicocele was significantly more common in the pathospermia group than in the normospermia group (18.3% and 5.7%, respectively). In the group with normospermia, grade 3 varicocele was not detected. It can be said that varicocele remains one of the leading factors negatively affecting the male reproductive system (p<0.001).
5. Conclusions
1. There are a number of risk factors that can potentially affect male reproductive health. These include lifestyle factors, tobacco smoking, alcohol use, overweight and obesity, sedentary lifestyle, diet, sexual activity, varicocele, etc. Their negative impact can largely be overcome through behavior modification and better lifestyle choices. 2. The negative impact of each risk factor on male fertility varies in strength. According to the results of our studies, the leading factors are varicocele, financial difficulties, bad habits, promiscuous sex life, sedentary and sedentary lifestyle and work. The impact of these risk factors does not occur separately, but simultaneously, and each of them has a different duration and severity.
References
| [1] | G. Nosova, Yu. V. Fedortsova, V. V. Morev, I. A. Korneev. The study of risk factors for the development of infertility in men who applied to the center of assisted reproductive technologies. Urological statements. Volume III No. 3 2013. ISSN 2225-9074. With. 18-21. |
| [2] | D.D. Zybin. The role of standards in the organization of medical care for men with infertility. Problems of standardization in health care. 3-4, 2018. p. 19-22. |
| [3] | O.R. Radzhenko. A.V. Shulaev. Methodological approaches to the organization of work to reduce risk factors and prevent male infertility. Guidelines. Kazan 2018. 28 p. |
| [4] | Damayanthi Durairajanayagam. Lifestyle causes of male infertility. Arab J Urol. 2018 Feb 13; 16(1): 10-20. doi: 10.1016/j.aju.2017.12.004. eCollection 2018 May. |
| [5] | Friday Ebhodaghe Okonofua, 1 , 2 , 3 Lorretta Favour Chizomam Ntoimo, 3 , 4 Akhere Omonkhua, 2 , 5 Oladiran Ayodeji, 6 Celestina Olafusi, 6 Emmanuel Unuabonah, 7 and Victor Ohenhen 8 Causes and Risk Factors for Male Infertility: A Scoping Review of Published Studies. Int J Gen Med. 2022; 15: 5985–5997. Published online 2022 Jul 4. doi: 10.2147/IJGM.S363959. |
| [6] | Gameiro S, Boivin J, Dancet E, Emery M, Thorn P, Van den Broeck U, et al. Qualitative research in the ESHRE Guideline ‘Routine psychosocial care in infertility and medically assisted reproduction - a guide for staff Guideline Development Group of the ESHRE Guideline on Psychosocial Care in Infertility and Medically Assisted Reproduction. Hum Reprod. 2016; 31: 1928–9. |
| [7] | Marie Bisconti, Jean-François Simon, Sarah Grassi, Baptiste Leroy, Baptiste Martinet, Vanessa Arcolia, Vladimir Isachenko, Elise Hennebert. Influence of Risk Factors for Male Infertility on Sperm Protein Composition Int J Mol Sci. 2021 Dec; 22(23): 13164. Published online 2021 Dec 6. doi: 10.3390/ijms222313164. |
| [8] | Sengupta P., Borges E., Jr, Dutta S., Krajewska-Kulak E. Decline in sperm count in European men during the past 50 years. Hum Exp Toxicol. 2017. |
| [9] | Shi X., Chan C., Waters T., Chi L., Chan D., Li T.C. Lifestyle and demographic factors associated with human semen quality and sperm function. Syst. Biol. Reprod. Med. 2018; 64: 358–367. doi: 10.1080/19396368.2018.1491074. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML