Bakhrom M. Mamatkulov1, Abdurashid A. Nematov1, Bakhora V. Urinova2
1School of Public Health, Tashkent Medical Academy, Tashkent, Uzbekistan
2Faculty of Treatment, Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Factors affecting the epidemic process in coronavirus infection are divided into 2 main groups: socio-hygienic and medical-biological. Their effects can be constantly variable and random. On the one hand, the short incubation period, the effective respiratory mechanism of virus infection, the high sensitivity of the population to coronavirus infection contribute to an increase in the high level of contagion of the virus and its rapid spread. Factors that affect constantly and in the long term not only determine the degree of incidence in a particular area, but can also accelerate or reduce the epidemic process in a certain amount.
Keywords:
COVID-19, SARS-CoV-2, Public health, Social-hygienic and medical-biological factors, Mental-emotional factors
Cite this paper: Bakhrom M. Mamatkulov, Abdurashid A. Nematov, Bakhora V. Urinova, The Role of Social-Hygienic and Medical-Biological Factors in the Spread of Coronavirus Infection (SARS-CoV-2) Among the Population, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 943-947. doi: 10.5923/j.ajmms.20221209.20.
1. Introduction
The level of the public health is formed under the influence of medical - biological and socio-hygienic factors, and the presence of these factors also affects their health. It should also be noted that each of the factors can have a cumulative effect on human health. Unsatisfactory level of living, socio-hygienic conditions and medical culture of the population also leads to deterioration of their health indicators. Studies show that focusing on lifestyle issues, prevention of chronic diseases and their complications, and self-isolation remain among the responsibilities of each population group [1,2].It was found that the presence of bad mental condition in families is also important in the origin of diseases. In particular, it has been emphasized in the scientific research of many scientists that the spread of various diseases in family members living a peaceful and prosperous life is less than in families with family conflicts and bad mental environment [2,3,4].When assessing the incidence of COVID-19 in countries around the world including male gender, black ethnicity, social disadvantage (measured by education, housing and income), health worker, unemployed or retired, current or former smoker, obesity, chronic diseases (the presence of factors such as cardiovascular diseases, hypertension, diabetes, chronic respiratory diseases, autoimmune diseases, cancer) among the population included them in the potential risk group for the origin of the COVID-19 disease [3,5,8,9]. Determining and evaluating these indicators for health care will provide practical help in predicting the level of disease incidence in the future and the possibility of falling into severe cases during the disease, as well as in the systematic implementation of proper treatment and preventive measures against the disease [6,7].
2. Aim
Studying and evaluating the impact of social-hygienic and medical-biological factors on the spread of coronavirus infection (SARS-CoV-2).
3. Materials and Methods
600 patients who were treated with COVID-19 at Zangiota №1 and №2 Republican Hospital for Special Infectious Diseases were selected for the study using a random - mechanical selection method and a case group was formed from them. The control group included 600 healthy representatives of the population who did not get sick during the observation period. Data were collected and analyzed using a specially designed questionnaire using a questionnaire-survey method.
4. Results and Discussion
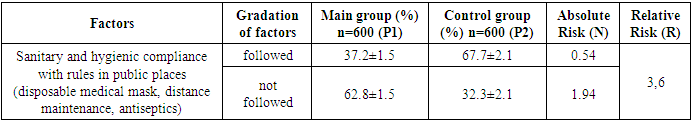
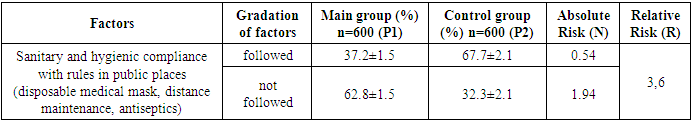
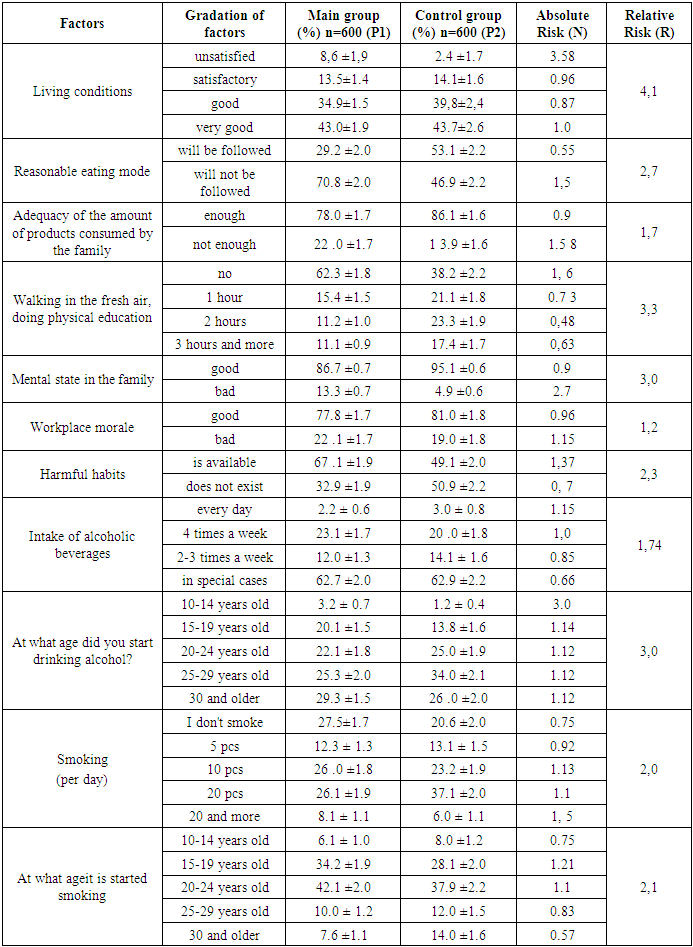
According to the result of our research, the following results were obtained and evaluated as a result of studying the lifestyle and quality of life of patients with coronavirus disease, the medical and social aspects of the disease, the health status of patients, and the risk factors that cause it. Moreover, in order to prevent the spread of the coronavirus infection, it is important to observe sanitary and hygienic rules in public places, in particular, to wear a disposable medical mask, to maintain a distance, and to use antiseptics. When sanitary and hygienic rules are observed in public places, the risk of contracting the disease is reduced by 3.6 times (Table 1).Table 1. The influence of sanitary-hygienic factors
 |
| |
|
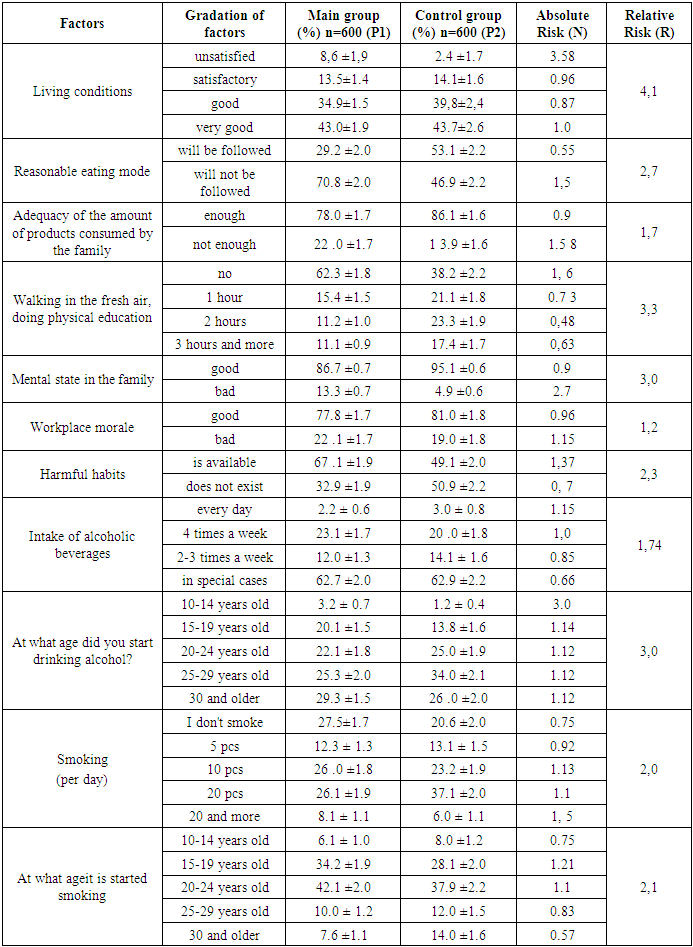
Factors of patients' lifestyle and living conditions (per capita living space, level of household amenities such as drinking water, heating source, gas, lighting source, sewerage, sanitary-hygienic condition of the room including light, humidity, cleanliness, etc.) was analyzed. It was found that 8.6±1.9% of the patients involved in the study had unsatisfactory living conditions, while this indicator was slightly better in the control group (p<0.001) was found to be 4.1 times higher. It was found that the mode and nature of eating (rational nutrition) can have a direct effect on the origin of the disease, its course and severity. According to the analysis of the questionnaire, only 29.2±2% of patients followed the diet, 9.4±1.2% of them ate bitter, salty, 11.9±1.32% cholesterol-rich products, 21.2 ± 1.6% it was confirmed that they take more fried products.During the research, we also analyzed the diet of the main and control groups. According to it, the intake of sufficient amounts of flour, leguminous products, milk, meat products, fish, fruits and vegetables among individuals in the main group was 29.2±2%. In the control group, this indicator is equal to 53.3±1.7% (r<0.001). So, in the main group, it was found that those who do not pay attention to the norm in the diet and who do not properly organize their diet are 2-3 times higher.Proper organization of the daily routine, rest, walking in the fresh air, exercise and sports are important in the prevention of the disease of COVID-19, and even in its treatment.Taking this into account, we studied the attitudes of individuals in the main and control groups involved in the study to these activities. According to the results of the analysis, the duration of walking in the fresh air and physical education among patients is as follows: respondents who walk in the fresh air for up to 1 hour every day have 15.4±1.5%, 3 hours and more - 11.1±0.9%, it was found that 62.3±1.8% of them do not engage in physical education at all. In the control group, this indicator was 38.2±2.2% (p<0.001). It was found that walking in the fresh air and engaging in regular physical activity can reduce people's chances of contracting COVID-19 by 3.3 times.Mental-emotional factors significantly affect the course of diseases. Mental and emotional disorders, stress aggravate the clinical course of the disease and cause a severe course of the disease.Our research revealed the mental state of the families of patients infected with the coronavirus such as negative relationships between family members, disagreements, the fact that one of the family members consumed alcohol, and the loss of a breadwinner had a negative effect on their psyche and health. The results of the study showed that 13.3±0.7% of the main group had a bad mental state at home, and this state was 3 times higher than that of the control group.According to scientific literature, harmful habits associated with an unhealthy lifestyle have a negative effect on the course of any disease. In particular, smoking and drinking alcohol lead to the development of respiratory diseases, the decrease of the body's immune system, and as a result, the development of chronic diseases. 67.1±1.9% of patients and 49.1±2% of control group have harmful habits (p=0.01) (Table 2).Table 2. Influence of lifestyle factors and unhealthy habits on the disease of COVID-19
 |
| |
|
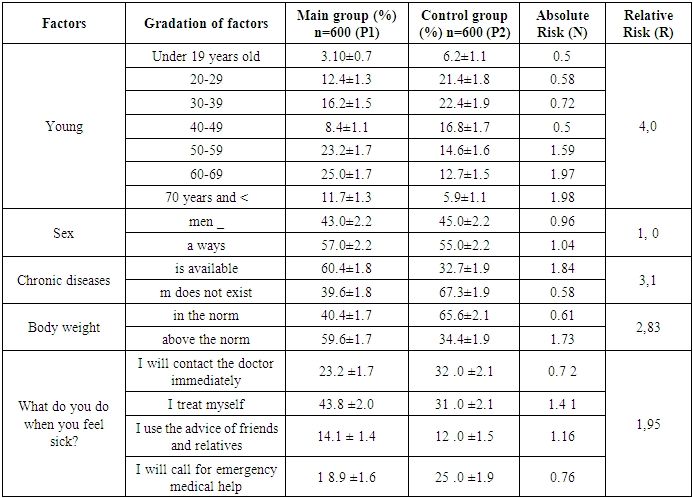
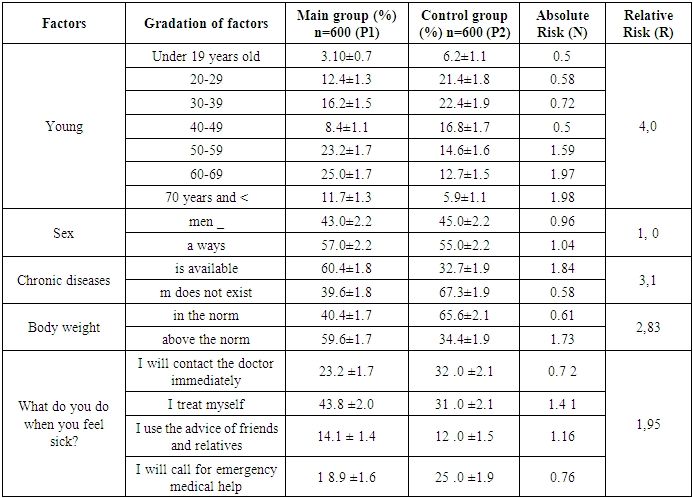
The health status, quality of life of the population and its improvement depend on their medical activity, their attitude to their health, their attention to medical services, and their medical culture. The results of our study showed that 67±1.9% of patients (more than 2/3) do not read medical literature at all. 11±1.3% of patients stated that they read specialized medical literature, 10±1.2% read popular brochures, and 12 ±1.3% read medical jourrnals.Referral to a doctor with acute and chronic diseases was 2 times higher in the control group compared to the incident group, and the lack of understanding about the prevention of chronic diseases was 3.5 times higher. It was found that individuals who do not have these factors have a high probability of contracting the disease of COVID-19 and a strong negative impact on the origin of the disease (r=0.34). During the last 2-3 years, it was confirmed that the rate of complete completion of preventive medical examinations was 3 times lower in the incident group than in the control group (p<0.001).Existing chronic diseases in the body have an effect on the origin and progress of other acute diseases. It worsens the course of the disease, 60.4±1.8% of patients and 32.7±1.9% of the control group have chronic concomitant diseases. People with chronic diseases have a 3.1 times higher probability of contracting COVID-19 than people without chronic diseases, and its severe course was noted (R= 3.1) (Table 3). 24.0±1.7% of patients admitted that they had not undergone a medical examination at all to the question of the questionnaire about having undergone a preventive medical examination in the next 2-3 years. This indicator was 11.1±1.3% in the control group.The age of patients increases the probability of contracting the disease and the severity of the disease. In particular, after the age of 70, the probability of contracting the disease and the severity of the disease increased by 3.96 times (R = 3.96, p<0.01) (Table 3).Table 3. The influence of biological factors and the importance of population medical activity in the spread of COVID-19
 |
| |
|
Excess body weight aggravates the course of any diseases. Based on the questionnaire, the body weight of the main and control groups was analyzed. According to it, 59.6±1.7% of the patients were overweight, 34.4±1.9% of the control group were overweight. It is noted that overweight individuals are 2.83 times more likely to develop a coronavirus disease compared to individuals with normal body weight, and it was found that these individuals have a severe course of the disease (R = 2.83 p<0.001).
5. Conclusions
1. High risk factors for the origin and course of the disease of COVID-19 including living conditions, age structure, non-observance of sanitary and hygienic rules, lack of walking in the fresh air and not engaging in physical activities, presence of chronic diseases, alcohol consumption, excess body weight, a healthy diet, mental state in the family and smoking have a strong influence.2. Regular identification of risk factors among the population over 50 years of age, who primarily refer to the health center, will lead to systematic preventive measures based on them, cases of reinfection with COVID-19, transfer of the disease to severe levels, and the reduction of deaths from this disease.
References
| [1] | Drapkina O. M., Gambaryan M. G., Gorny B. E. et al. Health promotion and prevention of chronic non-communicable diseases in a pandemic and self-isolation. Expert consensus of the National Medical Research Center for Therapy and Preventive Medicine and the Russian Society for the Prevention of Noncommunicable Diseases // Cardiovascular Therapy and Prevention. 2020. No. 19. S. 270-294. DOI: 10.15829/1728-8800-2020-2605. |
| [2] | Kasyanov V.V., Gafiatulina N.Kh., Vaskov M.A. Russian population in conditions of self-isolation regime: analysis of deprivation impact on social health // State and municipal management. 2020. No. 2. S. 204-209. DOI:10.22394/2079-1690-2020-1-2-204-208. |
| [3] | Iokhvidov V. V. Healthy lifestyle under social quarantine restrictions: results and expectations // Humanitarian paradigm. 2020. No. 3. P. 8-15. |
| [4] | Kulabukhov D. A., Mozgovaya E. I., Volkova O. A., Ananchenkova P. I. The COVID-19 pandemic as a factor in the transformation of domestic violence// Problems of social hygiene, health care and the history of medicine. 2021. V. 29, No. 1. S. 41-45. DOI:10.32687/0869-866X-2021-29-1-41-45. |
| [5] | Marc Chadeau-Hyam, 1,2 Barbara Bodinier, 1,2 Joshua Elliott, 1,2,3 Matthew D. Whitaker, 1,2 Ioanna Tzoulaki, 1,2,4 Roel Vermeulen, 5 Michelle Kelly-Irving, 6§ Cyrille Delpierre 6§ and Paul Elliott 1,2§: Risk factors for positive and negative COVID-19 tests:a cautious and in-depth analysis of UK biobank data: International Journal of Epidemiology, 2020, Vol. 0, No. 0 (https://pubmed.ncbi.nlm.nih.gov/32814959/). |
| [6] | Xiaoyu Fang 1,2,*, Shen Li 3,*, Hao Yu 4,*, Penghao Wang 3,*, Yao Zhang 2, Zheng Chen 2, Yang Li 5, Liqing Cheng 6, Wenbin Li 7, Hong Jia 1,#, Xiangyu Ma 2, #Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis AGING 2020, Vol. 12, No. 13. |
| [7] | Marc Chadeau-Hyam, 1,2* Barbara Bodinier, 1,2 Joshua Elliott, 1,2,3 Matthew D. Whitaker, 1,2 Ioanna Tzoulaki, 1,2,4 Roel Vermeulen, 5 Michelle Kelly -Irving, 6§ Cyrille Delpierre 6§ and Paul Elliott 1,2§: Risk factors for positive and negative COVID-19 tests: a cautious and in-depth analysis of UKbiobank data: International Journal of Epidemiology, 2020, Vol. 0, No. 0. |
| [8] | Wu B. (2020). Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob. Health Res. Policy 5 1–3. 10.1080/01634372.2021.1958115 [PMC free article] [PubMed] [CrossRef] [Google Scholar]. |
| [9] | Cacioppo JT, Hawkley LC (2009). Perceived social isolation and cognition. Trends Cogn. Sci. 13 447–454. [PMC free article] [PubMed] [ Google Scholar]. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML