-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(9): 920-923
doi:10.5923/j.ajmms.20221209.15
Received: Aug. 20, 2022; Accepted: Sep. 8, 2022; Published: Sep. 15, 2022

Evaluation of the State of the Oral Mucosa and Tactics of Its Treatment in Patients with Coronovirus Infection Complicated by Arterial Hypertension
Khabibova Nazira Nasullaevna1, Razikova Dilnoza Kadyrovna2
1Bukhara State Medical Institute, Uzbekistan
2Bukhara Regional Second Children's Dental Clinic, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

At the present stage of the development of medicine, the features of dental morbidity in the population are the high prevalence and intensity of damage to the dentition, the simultaneous development of several types of dental pathology of carious and non-carious origin, as well as inflammatory diseases of the periodontium and oral mucosa. The pathogenesis of SARS-CoV-2 lesions has not been studied. It is believed that the virus enters the cell by attaching to angiotensin-converting enzyme-2 (ACE2) receptors. Diseases of the oral cavity in most cases are the first clinical signs of systemic disorders.
Keywords: COVID-19, Blood pressure, Overproduction of pro-inflammatory cytokines, Interleukin-6
Cite this paper: Khabibova Nazira Nasullaevna, Razikova Dilnoza Kadyrovna, Evaluation of the State of the Oral Mucosa and Tactics of Its Treatment in Patients with Coronovirus Infection Complicated by Arterial Hypertension, American Journal of Medicine and Medical Sciences, Vol. 12 No. 9, 2022, pp. 920-923. doi: 10.5923/j.ajmms.20221209.15.
Article Outline
1. Introduction
- To study the clinical and laboratory parameters of the oral fluid and blood in patients who underwent COVID-19 against the background of arterial hypertension, and also, based on the study of the state of the oral mucosa, to develop tactics for managing these groups of patients. Once infected, the virus spreads through the mucus through the respiratory tract, causing a significant release of cytokines and an immune response in the body. There is a decrease in the number of lymphocytes in the blood, in particular T-lymphocytes [9,10]. Currently, it is known that the infectious process, including COVID-19, can cause the development of decompensation of chronic cardiovascular diseases (heart failure - HF, coronary artery disease, increased risk of thrombotic complications). Acute myocardial injury has also been described against the background of COVID-19. Dysregulation of the renin-angiotensin-aldosterone system (RAAS), respiratory failure, hypoxia, oxidative stress, mitochondrial dysfunction, and inflammation are discussed as the main mechanisms.
2. Research Objectives
- - to study the features of clinical and laboratory manifestations of the main dental diseases in patients who have undergone COVID-19 complicated by arterial hypertension;- to assess the state of the protective system of the oral cavity and the functional state of the endothelium in patients with arterial hypertension;- to study the state of the endothelium in patients who underwent coronavirus against the background of chronic inflammation of the oral mucosa with combined arterial hypertension;
3. Relevance of the Topic
- Arterial hypertension remains one of the determining risk factors for the development of severe cardiovascular pathology in people of working age.The significant prevalence of arterial hypertension and the frequency of its complications determine the relevance of research on the active detection, treatment and prevention of the disease at the population level.Along with an increase in the frequency of detection of cardiovascular diseases, their incidence and mortality from them in young working-age people has increased significantly, thereby increasing the importance of early diagnosis of arterial hypertension, which makes it possible to have an effective effect before irreversible organic changes occur in target organs [6,10,15].Diseases of the oral mucosa and pathological processes in periodontal tissues in arterial hypertension are explained by the pathogenetic commonality of these processes.One of the most important factors in the pathogenesis of hypertension is a violation in the microcirculatory bed, which is the basis of inflammatory-destructive diseases of periodontal tissues and oral mucosa [5,6,9].The change in the microcirculatory bed progresses with the development of the disease and closely correlates not only with the severity of arterial hypertension, but also with the degree of circulatory disorders in the periodontium.It has been established that the periodontal microvasculature, an active zone in the hemodynamics of the whole organism, undergoes changes with constant or frequently occurring stresses in the vascular system [4,8,9].Great importance in the occurrence and development of hypertension, generalized periodontitis and periodontal disease is given to increased activation of the sympathetic division of the autonomic nervous system, which leads to dysfunction of the centers that regulate vascular tone and blood pressure, microcirculatory disorders, increased vascular permeability, including including in periodontal tissues [8,11,16,17].It should also be taken into account that in patients with chronic generalized periodontitis and periodontal disease, combined with arterial hypertension, hypoxia contributes to an increase in the excitability of the sympathetic-adrenal system, swelling of the endothelium of arterial vessels, deterioration of redox processes in periodontal tissues, lower ¬niya adaptive capabilities of the microvasculature and connective tissue.Given the prevalence of coronary heart disease, a comprehensive assessment of the dental status of such patients is necessary, the identification of odontogenic foci of inflammation, inflammatory periodontal diseases and their sanitation, the development of recommendations for individual oral hygiene, taking into account the possible occurrence of dry mucous membranes. The traditional inclusion of pastes and rinses based on chlorhexidine in the complex treatment can cause such undesirable consequences as dysbiotic changes, staining of the tongue and teeth, taste disturbance. That is why studies aimed at identifying the characteristics of the dental status of patients with coronary artery disease, evaluating the effectiveness of personal oral hygiene products of constant use, which have anti-inflammatory, antiseptic and moisturizing effects, but do not cause dysbiotic changes in the oral cavity, are relevant.
4. Material and Research Methods
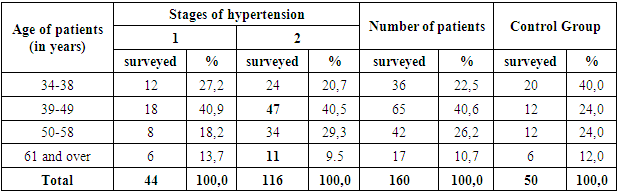
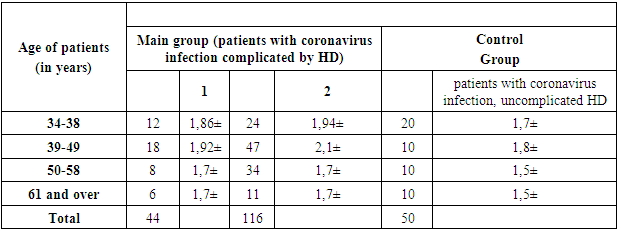
- The results of clinical and functional studies of the state of the oral mucosa in patients with coronavirus infection complicated by hypertension (stages I and II) and in persons without arterial pressure served to solve the tasks. The examination of the oral mucosa was carried out on the basis of the infectious diseases hospital of the city of Bukhara.The total number of examined persons of the main and control groups was 210 patients.Patients with coronavirus infection complicated by hypertension underwent a clinical examination, which included subjective, objective and additional research methods. During the examination, all patients underwent repeated measurements of blood pressure and in the anamnesis, they took into account how long the disease of hypertension began, the presence of dizziness and tinnitus, whether the head hurts (the nature and duration of the headache), goosebumps, fatigue, physical weakness, as well as concomitant and past diseases, heredity of hypertension, bad habits, occupational hazards, psycho-emotional stress and taking antihypertensive drugs.
|
|
5. Conclusions
- It has been established that in patients with OM pathology combined with hypertension, there is a decrease in thromboresistance of the vascular wall, which is manifested by inhibition of the anticoagulant and fibrinolytic activity of the endothelium, which is apparently associated with a change in thromboresistance of the vascular endothelium. A decrease in the anticoagulant activity of the vascular endothelium in patients of the main group is manifested by inhibition of the release of antithrombin III by the endothelium of the vascular wall. Inhibition of the fibrinolytic activity of the vascular endothelium may be associated with a decrease in the release of tissue plasminogen activator t-PA and an increase in the level of homocysteine.In chronic inflammatory diseases of the oral mucosa with a combination of its hypertension, especially in those who had coronavirus, a slight increase in the concentration of pro-inflammatory cytokines IL-1b, IL-6 was noted in the blood and oral fluid. At the same time, the concentration of lactoferrin and cortisol in the oral fluid has a multidirectional character in patients who have undergone coronavirus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML